Abstract
Bisphosphonate, a potent anti-resorptive agent, is generally accepted as a safe, effective, well tolerated treatment for postmenopausal osteoporosis. Atypical femoral fracture (AFF) and bisphosphonate related osteonecrosis of jaw (BRONJ) are the increasing morbidities in patients treated with long term bisphosphonate. Pathogenic mechanisms of AFF and BRONJ are not fully identified and not identical. We report a case of BRONJ followed by AFF and its nonunion in a 67-year-old woman patient receiving an oral bisphosphonate during 7 years for the treatment of osteoporosis.
Bisphosphonate, a potent anti-resorptive agent, is generally accepted as a safe, effective, well tolerated treatment for postmenopausal osteoporosis. Although the short-term safety and the efficacy of these drugs have been investigated and documented, an increasing number of recent reports draw attention to the possible correlation between long-term bisphosphonate therapy and the occurrence of morbidities mediated by inhibition of osteoclast function serves to decrease resorption.[1] Recent reports have noted atypical femoral fractures (AFF) and bisphosphonate related osteonecrosis of jaw (BRONJ) are the increasing morbidity in patients who have undergone long-term bisphosphonate therapy for osteoporosis. [2,3,4,5,6,7] Pathogenic mechanisms of AFF and BRONJ are not identified and not identical. We experienced a rare case of BRONJ followed by AFF and its nonunion in a same patient who was treated by long-term bisphosphonate administration for osteoporosis.
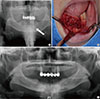
A 67-year-old woman was diagnosed oseteoporosis and treated with oral Risedronate (150 mg/month for 2 years), Ibandronate (150 mg/month for 2 years) and Alendronate (70 mg/week for 3 years) for 7 years. She presented with sudden developed right hip pain despite no evidence of definite trauma. On the radiograph, transverse, noncomminuted subtrochanteric fracture with medical beak was noted. She was treated with closed reduction using long proximal femoral nail (Long Gamma-3 nail, Stryker) in the regional hospital (Fig. 1). Osteoporosis treatment has been discontinued. But from 6 months after the surgery she discontinued the schedule of our out-patient department. After three years of operation, she showed up at our out-patient department with pain in the right hip joint while walking despite no evidence of trauma. On the radiograph, nonunion of subtrochanteric fracture and breakage of long Gamma-3 nail was noticed (Fig. 2). Her height was 145 cm, body weight 55 kg, and body mass index (BMI) 26.1 kg/m2. The bone mineral density (BMD) of lumbar spine measured by dual energy X-ray absorptiometry (Discovery™, Hologic, Bedford, MA, USA) was 0.490 g/cm2, of which the T score was -3.6 and the Z score -1.2. The levels of serum calcium and phosphorus were 9.1 mg/dL (normal 8.6-10.0 mg/dL) and 4.5 mg/dL (normal 2.8-4.5 mg/dL), respectively. The serum C-terminal telopeptides of type I collagen (CTx) and urinary N-terminal telopeptides of type I collagen (NTx) levels measured by enzyme-linked immunosorbent assay (ELISA) were 55.7 nmoL bone collagen equivalents (BCE)/mmoL Cr (normal 6.0-125.7 nmoL BCE/mmoL Cr) and 0.26 ng/mL (normal 0.11-1.00 ng/mL). We removed the broken nail and exchanged to cephalomedullary nailing and autogenous iliac bone graft was done (Zimmer Natural Nail Cephalomedullary nail, Zimmer). We performed osteotomy at lateral cortex below the lag screw to making a notch for sliding (Fig. 3). After the revision operation, she was treated with daily subcutaneous injection of teriparatide (recombinant human parathyroid hormone 1-34) at a dose of 20 µg per day and her symptom resolved gradually for 6 months. She underwent outpatient follow up of dental clinic due to extraction of the mandibular right lateral incisor, right central incisor, left central incisor 1 year before visit to our outpatients department (OPD) clinic, following which the extraction socket never healed and pain and pus discharge for 2 months (Fig. 4). Oral antibiotics treatment and local debridement were ineffective. Sequestrectomy of mandible and incision and drainage of submental abscess was done. Intravenous antibiotics for 2 weeks and oral antibiotics for 10 weeks were administrated postoperatively. No more abscess drainage oral cavity and no more pain was complaint. BRONJ was diagnosed at 9 years after the osteoporosis treatment.
Bisphosphonate is the most widely prescribing agent for treating osteoporosis. As one of the strong bone resorption inhibitors, it reduces the risks of major fractures in females with osteoporosis. However, many reports have suggested that long-term use of bisphosphonate is associated with AFF or BRONJ.[2,3,8,9] The patient of this case was treated with oral bisphosphonate for 7 years and discontinued as AFF was considered. Park-Wyllie et al.[10] reported that bisphosphonate treatment of more than five years was associated with an increased risk of atypical subtrochanteric or femoral shaft fractures. The incidence of AFF reported 3.2 to 5.9 cases per 100,000 person-years (with American Society for Bone and Mineral Research major criteria) and 113.1 cases per 100,000 cases per year for 8 to 9 years of use or 130 per 100,000 cases per year for 6 years of use.[9,10,11,12,13] Although incidence of BRONJ is small as 1/100,000-1/10,000 annually.[14] The risk of developing BRONJ associated with oral bisphosphonates appears to increase when the duration of therapy exceeds three years.[3] Many reports suggest that the use of intravenous bisphosphonates in cancer patients is associated with BRONJ.[3] But, with lower dose of oral bisphosphonate, BRONJ cases were also reported sporadically.[1,15,16] Association of Oral and Maxillofacial Surgeons reported local risk factor of BRONJ as 1) Extractions, 2) Dental implant placement, 3) Periapical surgery, 4) Periodontal surgery involving osseous injury and suggest three months of drug discontinuation prior to elective dental invasive procedure reduces the risk of developing BRONJ.[3] A common pathogenesis of BRONJ and AFF explains that the Jaw bone and lateral cortex of subtrochanteric area of femur demand to endure higher mechanical stress than the other bones that are comparable. Since bone remodeling removes old or damaged bone and replaces it with new bone, the suppression of remodeling may reduce damage repair of continuous mechanical stress.[2,9,17] The pathogenesis of BRONJ explains in several ways 1) Depletion of first line immune cell in the oral cavity; γδ T cells.[18] 2) Inhibition of epithelial migration and capillary tube formation for neo-angiogenesis.[19] The pathogenesis of AFF differ from that of BRONJ explains in several ways 1) Reduced heterogenecity, which reduces local stress and enhance energy dissipation, of organic matrix and mineral properties.[2] 2) high strain in the lateral cortex of the subtrochanteric area during various stage of gait cycle, especially in single stance phase. However, the current level of evidence of exact pathophysiology does not fully support relationship between AFF and BRONJ.
We experienced a rare case of AFF followed by BRONJ related to long-term use of oral bisphosphonate therapy for osteoporosis who have 2 year of drug holidays in an elderly patient. When AFF was noticed, it is crucial for remind that a AFF can be a high risk factor of development of BRONJ and patients education for BRONJ should be considered, as senile patient have much chance for all invasive dental procedures.
Figures and Tables
 | Fig. 1(A) Preoperative radiograph shows subtrochanteric fracture of left femur: Transverse fracture with medial beak were noticed. (B) Postoperative radiograph after the initial operation. |
Notes
References
1. Allen MR, Burr DB. Bisphosphonate effects on bone turnover, microdamage, and mechanical properties: what we think we know and what we know that we don't know. Bone. 2011; 49:56–65.

2. Unnanuntana A, Saleh A, Mensah KA, et al. Atypical femoral fractures: what do we know about them?: AAOS Exhibit Selection. J Bone Joint Surg Am. 2013; 95:e8 1–e8 13.
3. Ruggiero SL, Dodson TB, Assael LA, et al. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws-2009 update. J Oral Maxillofac Surg. 2009; 67:2–12.

4. Pazianas M, Miller P, Blumentals WA, et al. A review of the literature on osteonecrosis of the jaw in patients with osteoporosis treated with oral bisphosphonates: prevalence, risk factors, and clinical characteristics. Clin Ther. 2007; 29:1548–1558.

5. Giusti A, Hamdy NA, Papapoulos SE. Atypical fractures of the femur and bisphosphonate therapy: a systematic review of case/case series studies. Bone. 2010; 47:169–180.

6. Almăşan HA, Băciuţ M, Rotaru H, et al. Osteonecrosis of the jaws associated with the use of bisphosphonates. Discussion over 52 cases. Rom J Morphol Embryol. 2011; 52:1233–1241.
7. Advisory Task Force on Bisphosphonate-Related Ostenonecrosis of the Jaws. American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2007; 65:369–376.
8. Seraphim A, Al-Hadithy N, Mordecai SC, et al. Do bisphosphonates cause femoral insufficiency fractures? J Orthop Traumatol. 2012; 13:171–177.

9. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the american society for bone and mineral research. J Bone Miner Res. 2014; 29:1–23.

10. Park-Wyllie LY, Mamdani MM, Juurlink DN, et al. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA. 2011; 305:783–789.

11. Dell RM, Adams AL, Greene DF, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res. 2012; 27:2544–2550.

12. Meier RP, Perneger TV, Stern R, et al. Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med. 2012; 172:930–936.

13. Feldstein AC, Black D, Perrin N, et al. Incidence and demography of femur fractures with and without atypical features. J Bone Miner Res. 2012; 27:977–986.

14. Khosla S, Burr D, Cauley J, et al. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2007; 22:1479–1491.

15. Ruggiero SL, Mehrotra B, Rosenberg TJ, et al. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004; 62:527–534.

16. Salesi N, Pistilli R, Marcelli V, et al. Bisphosphonates and oral cavity avascular bone necrosis: a review of twelve cases. Anticancer Res. 2006; 26:3111–3115.
17. Reid IR. Osteonecrosis of the jaw: who gets it, and why? Bone. 2009; 44:4–10.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download