Abstract
Background
On retrospective basis, we investigated the detection of osteoporotic vertebral fractures (OVFs) without radiologic collapse using a modified Yoshida's classification, which was designed by the authors.
Methods
We observed 82 cases in 76 patients with confirmed OVFs without collapse at the thoracolumbar junction. The following factors were measured: age, gender, body mass index (BMI, kg/m2), bone mineral density (BMD, mg/cm3), type of a modified Yoshida's classification. The correct diagnosis rate for the presence and location of OVFs and the correct diagnosis rate according to the morphological type by a modified Yoshida's classification of the OVFs were analyzed.
Results
The mean BMI was 21.2; mean BMD, 44.1; and T-score, -4.4. As for the four subtypes of anterior cortical morphological change, there were 14 cases of the protruding type, 12 cases of the indented type, 5 cases of the disrupted type and 8 cases of the prow type. As for the three subtypes of endplate depression, there were 20 cases of upper endplate depression, 12 cases of lower endplate depression and 11 cases of endplate slippage type. According to the examiners, there was a significant difference between being informed before and after the modified Yoshida's classification. For the relationship of examiners and the type of fracture, there was a significant difference between being informed before and after the modified Yoshida's classification, particularly in the protruding type and the upper plate type.
Osteoporotic vertebral fractures (OVFs) are associated with increased morbidity and mortality.[1] Morbidity associated with these fractures includes pain and decreased physical function, which have a significant impact on the quality of life.[2] Therefore, early diagnosis and treatment of OVFs is crucial. The detection of OVF is based primarily on the identification of vertebral collapse; however, this can be misleading in the presence of a fracture without radiologic collapse or normal variants and degenerative change of the vertebrae. Hence, a semi-quantitative approach was developed in an attempt to reduce the subjectivity associated with the visual diagnosis of OVFs.[3-5] However, there is still no internationally agreed definition for vertebral fractures.[6] According to several studies, vertebral fractures were frequently underdiagnosed radiologically worldwide, with false-negative rates as high as 30% despite a strict radiographic protocol minimizing underdiagnosis.[7-10]
Recently, the definition of occult OVFs has been established; yet, its diagnosis is difficult with simple radiographs.[11] The semi-quantitative method can be difficult to be accurately applied to the occult OVFs; further, the criterion of 20 to 25% for the identification of Genant's Grade I is ambiguous.[4] Although magnetic resonance imaging (MRI) has a high accuracy rate for the definite diagnosis of OVFs, it is not possible to use MRI with all patients due to the limitations in equipment and economical cost. Therefore, we investigated the detection of occult OVFs with a modified Yoshida's classification in a simple radiograph on a retrospective basis.
We retrospectively reviewed 82 cases in 76 patients (Male/Female: 20/56) who are over sixty-five years of age, diagnosed with acute OVFs without radiologic collapse at the thoracolumbar junction (from T11 to L2) in one hospital from June 2006 to December 2012. The inclusion criteria for this study were as follows: 1) painful OVFs, also known as fresh OVFs, refer to symptomatic fractures, which were confirmed by MRI; 2) fractured vertebrae which appeared normal or with minimal deformation were rated according to Genant's grade from 0 to 0.5; however, the vertebral height was visually normal; 3) fractures with osteoporosis (bone mineral density [BMD, mg/cm3]<80 mg/cm3 and T-score<-2.5). We excluded patients who had vertebral fractures from high velocity injuries, such as a motor vehicle accidents or falling accidents, as well as those who were under sixty-five years of age and had undergone a previous spine fusion operation. All patients were checked with a simple thoracolumbar lateral radiograph, and the BMD measurement of the lumbar spine was taken at the time of injury. We measured age and gender, body mass index (BMI, kg/m2) with weight and height, and whether the patient had undergone percutaneous vertebroplasty. BMD was measured by utilizing the quantitative computed tomography (QCT; Somatom sensation 16, Simens, Erlangen, Germany) of the thoracolumbar vertebrae, enabling separate analyses of cortical, trabecular and total bone density, including the T-score.
The morphological classification used in the current study was a modified Yoshida's classification designed by the authors based on the classification of Yoshida. Yoshida's criteria is classified into four types: protruding type, indented type, end plate slippage type and endplate compression type.[12] The modification of Yoshida's classification by the authors includes two types and seven subtypes as follows: anterior cortical morphological change type has four subtypes: protruding type, indented type, disrupted type and prow type; endplate depression type has three subtypes: upper endplate depression, lower endplate depression type and endplate slippage type (Fig. 1). The diagnostic assessment of radiographic vertebral fractures has been conducted by three radiologists and two orthopedic surgeons. During the assessment, there was no information regarding the patient's age, sex, the presence of fracture, BMD and BMI. We analyzed the correct diagnosis rate as well as the type of fracture before and after the examiners informed us of the morphology using the modified Yoshida's classification of the occult OVFs, along with the relevance of the relationship in the examiners and the type of fracture. Inter-examiners reliability was analyzed using the Kendall's coefficient of concordance (W=0.427).
The results of the study were obtained using the chi-square test. All values recorded in this study were presented as frequency (%). SPSS software (version 19.0; SPSS Inc., Chicago, IL, USA) was used for all statistical calculations and the statistical significance was set at P<0.05 for all tests.
The mean age was 76.7 years. The mean BMI was 21.2 kg/m2; mean BMD, 44.1 mg/cm3; and T-score, -4.4. The most common fracture site was L1 (40.2%). As for the four subtypes of anterior cortical morphological change, there were 14 cases of the protruding type, 12 cases of the indented type, 5 cases of the disrupted type and 8 cases of the prow type. As for the three subtypes of endplate depression, there were 20 cases of upper endplate depression, 12 cases of lower endplate depression and 11 cases of endplate slippage type (Fig. 2, 3). Among the 61 patients who had surgery, 39 cases and 22 cases underwent vertebroplasty kyphoplasty, respectively.
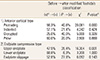
The overall correct diagnosis rate of the examiners was 64.5%. When informed of the modified Yoshida's classification, the correct diagnosis rate was 81.5% (P<0.05) (Table 1). There was no significant difference between being informed before and after the modified Yoshida's classification for the type of fracture (χ2=9.727, P>0.05). According to the examiners, there was a significant difference between being informed before and after the modified Yoshida's classification (χ2=41.616, P<0.001). In the relationship of the examiners and the type of fracture, there was a significant difference between being informed before and after the modified Yoshida's classification, particularly in the protruding type (χ2=20.081, P<0.001) and the upper endplate type (χ2=16.304, P<0.01). In the relationship of the examiners and the type of fracture, there was no significant difference between being informed before and after the modified Yoshida's classification, particularly in the indented (χ2=4.242, P>0.05), disrupted (χ2=5.000, P>0.05), prow (χ2=2.500, P>0.05), lower endplate (χ2=3.200, P> 0.05) and endplate slippage (χ2=6.092, P> 0.05) type (Table 2). In particular, there was no difference at all between being informed before and after the modified Yoshida's classification with the lower endplate type (P=1.000). The correct diagnosis rate was significantly higher in the OVFs, even when both the protruding and upper plate types (P< 0.05) existed. Conversely, the correct diagnosis rate was low in the low endplate type.
Vertebral fractures are the hallmark of osteoporosis and are associated with increased morbidity and mortality.[1,2] Thus, the evaluation of spinal radiographs for the early diagnosis of OVFs is essential in order to reduce the progressive vertebral body collapse with deformity as well as the sustained pain with decreased physical function, along with the decreased quality of life. Based on clinical practice, OVFs can be divided into three categories according to fracture symptoms and presence of vertebral deformation on plain radiographs: 1) painful OVFs, also known as fresh OVFs, refer to symptomatic fractures with loss of the vertebral height; 2) painless OVFs, also known as old OVFs, are asymptomatic fractures with vertebral collapse; and 3) occult OVFs, which imply painful vertebral fractures without radiographic measurable compression.[13] The diagnosis of painful occult OVFs is difficult due to the unapparent radiographic finding. Pham et al.[11] reported that 21 cases of vertebral fractures in 16 patients were presented with a typical history of acute back pain in a setting of osteoporosis; however, there was no substantial deformation of the vertebral body at the initial plain radiographs. They stated that the osteoporotic spine is consistent with the well-known fractures found in the so-called "occult" or "insufficiency" fractures of the sacrum or femoral neck. Kanchiku et al.[14] reported that 10 out of 95 OVFs showing signal intensity changes on MRI were difficult to identify on plain radiographs due to almost no collapse of the vertebral body.
Several standardized approaches have been proposed to describe vertebral fractures.[3-6,15] There were various methods for evaluating OVFs based on simple radiography, including visual assessment of standard radiographs, Genant's semi-quantitative assessment, Jiang's qualitative methods, morphometric radiography and dual energy X-ray absorptiometry (DXA) measurement.[15] The preferred method may be Genant's semi-quantitative method, which was developed in an attempt to reduce the subjectivity associated with the visual diagnosis of OVFs. Recently, vertebral fracture assessment (VFA) by DXA is also used to detect vertebral fractures in asymptomatic patients undergoing routine BMD measurements.[16] However, there is still no gold standard for the definition of vertebral fractures. To our knowledge, there is only one available publication for the correct diagnosis rate regarding the presence and location of incident vertebral fractures according to Yoshida's classification.[12] Thus, we applied the detection of occult OVFs using a modified Yoshida's classification which was designed by the authors. It may be difficult to differentiae OVFs from deformities. Some of the more common mimickers are normal variants (Cupid's bow or limbus vertebra), metastatic disease (including multiple myeloma), Scheuermann's disease and Schmorl nodes.[17] The difficulty of reporting OVFs is due to the parallax effect (normal vertebrae to appear compressed). Further, a lack of consistency with the adjacent vertebrae need to be taken into consideration when diagnosing OVFs and moreover, strict morphometric measurements on radiographs can over- or under diagnose OVFs.[16,17] Large scale prospective studies have found that only about one-fourth of incident radiographic OVFs are diagnosed.[10] Retrospective studies on standard radiographs obtained in emergency treatment centers revealed a 55-65% diagnosis rate for OVFs.[18,19] Williams et al.[8] reported discovering a diagnosis rate of only 13% for OVFs by radiologists in the emergency treatment center. The false-negative fractured vertebrae rate was 25.8%, despite the standardized protocol of acquisition.[9] Further, a multinational study of 2,000 postmenopausal women with osteoporosis was conducted, in part, to assess the accuracy of radiographic diagnosis of OVFs, which reported a false-negative rate from 27% to 45%, despite the strict radiographic protocol.[7] In our study, the incorrect diagnosis rates of OVFs before and after being informed of the modified Yoshida's classification were 35.5% and 18.5%, respectively.
The diagnostic accuracy of MRI for incident vertebral fractures for sensitivity and specificity was 99.0% and 98.7%, respectively.[20] Kanchiku et al.[14] reported a diagnostic rate of 98% in the fractured vertebral body on MRI, which was higher than the 87% on plain radiography. Thus, MRI examination is an important diagnosis tool for the early diagnosis of occult OVFs. However, it is difficult to complete a different diagnosis of tumor and infection. The typical MRI finding in acute compression fracture is hypointensity on T1-weighted images, hypointensity or heterogeneous intensity on T2-weighted images, and hyperintensity on fat-suppressed T2-weighted images or on short-inversion time-inversion recovery images.[21,22] In our study, the fracture may escape detection on standard radiographs, only being confirmed through an MRI.
However, there is a limitation to this study. That is, we did not analyze the odds ratio of age, sex, BMI and BMD of the patients during examination.
In summary, a modified Yoshida's classification can be helpful for the diagnosis of OVFs without radiologic collapse in simple radiographs. This study presents the method of making a close observation of anterior cortical morphological change and endplate depression during an examination of OVFs in a simple radiograph.
Figures and Tables
Fig. 1
A modified Yoshida classified into two types and seven subtypes. Anterior cortical morphological change types: Protrusion type, the anterior bony cortex disrupted protrudes anteriorly; indented type, the anterior bony cortex disrupted indents posteriorly; disrupted type, the anterior bony cortex disrupted with no displacement; prow type, the anterior bony cortex disrupted mixed of anterior and posterior. Endplate compression types: upper endplate depression type, the center of the upper endplate disrupted and depression; lower endplate depression type, the center of the lower endplate disrupted and depression; endplate slippage type, the anterior edge of the endplate disrupted anteriorly.

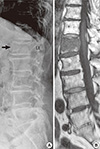
Fig. 2
An 87-year-old woman with occult osteoporotic vertebral fractures of L1 (A), confirmed by magnetic resonance imaging (B). L1 has a change of anterior cortex morphology (protruding type of modified Yoshida's classification) (arrow).

Fig. 3
A 92-year-old woman with occult osteoporotic vertebral fractures of L1 (A), confirmed by MRI (B). L1 has a change of endplate morphology (upper endplate slippage type of modified Yoshida's classification) (arrow).
References
1. Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009; 301:513–521.

2. O'Neill TW, Cockerill W, Matthis C, et al. Back pain, disability, and radiographic vertebral fracture in European women: a prospective study. Osteoporos Int. 2004; 15:760–765.
3. Grados F, Fechtenbaum J, Flipon E, et al. Radiographic methods for evaluating osteoporotic vertebral fractures. Joint Bone Spine. 2009; 76:241–247.

4. Genant HK, Jergas M. Assessment of prevalent and incident vertebral fractures in osteoporosis research. Osteoporos Int. 2003; 14:Suppl 3. S43–S55.

5. Lenchik L, Rogers LF, Delmas PD, et al. Diagnosis of osteoporotic vertebral fractures: importance of recognition and description by radiologists. AJR Am J Roentgenol. 2004; 183:949–958.

6. Grigoryan M, Guermazi A, Roemer FW, et al. Recognizing and reporting osteoporotic vertebral fractures. Eur Spine J. 2003; 12:Suppl 2. S104–S112.

7. Delmas PD, van de Langerijt L, Watts NB, et al. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005; 20:557–563.

8. Williams AL, Al-Busaidi A, Sparrow PJ, et al. Under-reporting of osteoporotic vertebral fractures on computed tomography. Eur J Radiol. 2009; 69:179–183.

9. Fechtenbaum J, Cropet C, Kolta S, et al. Reporting of vertebral fractures on spine X-rays. Osteoporos Int. 2005; 16:1823–1826.

10. Fink HA, Milavetz DL, Palermo L, et al. What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res. 2005; 20:1216–1222.

11. Pham T, Azulay-Parrado J, Champsaur P, et al. "Occult" osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976). 2005; 30:2430–2435.
12. Ito Z, Harada A, Matsui Y, et al. Can you diagnose for vertebral fracture correctly by plain X-ray? Osteoporos Int. 2006; 17:1584–1591.

13. Mao H, Zou J, Geng D, et al. Osteoporotic vertebral fractures without compression: key factors of diagnosis and initial outcome of treatment with cement augmentation. Neuroradiology. 2012; 54:1137–1143.

14. Kanchiku T, Taguchi T, Kawai S. Magnetic resonance imaging diagnosis and new classification of the osteoporotic vertebral fracture. J Orthop Sci. 2003; 8:463–466.

15. Chae SU, Kim GD. Radiographic diagnosis of the osteoporotic vertebral fractures. Osteoporosis. 2013; 11:59–65.
16. Guglielmi G, Diacinti D, van Kuijk C, et al. Vertebral morphometry: current methods and recent advances. Eur Radiol. 2008; 18:1484–1496.

17. Bennett DL, Post RD. The role of the radiologist when encountering osteoporosis in women. AJR Am J Roentgenol. 2011; 196:331–337.

18. Kim N, Rowe BH, Raymond G, et al. Underreporting of vertebral fractures on routine chest radiography. AJR Am J Roentgenol. 2004; 182:297–300.

19. Majumdar SR, Kim N, Colman I, et al. Incidental vertebral fractures discovered with chest radiography in the emergency department: prevalence, recognition, and osteoporosis management in a cohort of elderly patients. Arch Intern Med. 2005; 165:905–909.

20. Nakano T, Ochi R, Miyazono K, et al. Diagnosis precision of MRI for fresh osteoporotic vertebral body fracture and a diagnosis by follow-up roentgenogram (in Japanese). Osteoporos Jpn. 2004; 12:89–90.
21. Tanigawa N, Komemushi A, Kariya S, et al. Percutaneous vertebroplasty: relationship between vertebral body bone marrow edema pattern on MR images and initial clinical response. Radiology. 2006; 239:195–200.

22. Yamato M, Nishimura G, Kuramochi E, et al. MR appearance at different ages of osteoporotic compression fractures of the vertebrae. Radiat Med. 1998; 16:329–334.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download