INTRODUCTION
Bisphosphonate is analogues of pyrophosphate compounds and inhibits bone absorption effectively by suppressing osteoclast. In addition, it is utilized in a wide range of treatments including postmenopausal osteoporosis, Paget's disease, cancer-related osteolysis and hypercalcemia. Although bisphosphonate is known to be safe mostly, side effects such as gastrointestinal side effects, flu-like syndrome, nephrotoxicity, osteonecrosis of the jaw and hypocalcemia can be problematic.[1]
Recently, as elderly population increases due to increase of average life-expectancy, bisphosphonate utilization in purpose of prevention and treatment of osteoporotic fracture also tends to increase. Therefore, more attention needs to be paid regarding the side effects. Since the authors experienced a case of severe hypocalcemia after utilizing intravenous bisphosphonate in the treatment of osteoporosis, we would like to report the case with literature review.
CASE
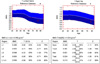
A 78-year-old female patient who had loss of appetite, lethargy, disorientation, and speech disturbance for several days came to our hospital in emergency room due to mental deterioration. About a month before the hospital visit, the patient had femur neck fracture caused by hitting on a table and then received hip arthroplasty under spinal anesthesia. At the time of the visit, blood pressure, body temperature, pulse rate, and respiratory rate were 120/70 mmHg, 36.5℃, 70 times/minute, and 20 times/minute, respectively, and the patient responded to pains but couldn't communicate. Brain magnetic resonance imaging (MRI) was carried out in order to check the occurrence of cerebrovascular event but acute lesion was not observed. Laboratory test showed the result of leukocyte count 6,530/µL, hemoglobin 11.3 g/dL, platelet count 197,000/µL, blood urea nitrogen 36.9 mg/dL (8-23), serum creatinine 3.67 mg/dL (0.6-1.2), fractional excretion of sodium (FENa) 5.9%, serum albumin 3.3 g/dL (3.2-4.5), sodium 143.4 mEq/L (136-142), potassium 3.3 mEq/L (3.8-5.0), corrected calcium concentration 3.96 mg/dL (9-11), phosphorus 2.5 mg/dL (2.3-4.7), parathyroid hormone (PTH) 486.6 pg/mL (12-88), ionized calcium 1.8 mg/dL (4-4.8), and magnesium 1.4 mg/dL (1.3-2.1). The corrected calcium concentration was calculated utilizing equation of 'total calcium concentration in serum (mg/dL) + (0.8 × (4.0 - serum albumin concentration [g/dL])'. On electrocardiography, corrected QT interval (519 msec) was prolonged, but Trousseau's phenomenon or Chvostek's sign was not exhibited. In the past medical history, no special diseases such as hypertension and diabetes were present and the patient was a non-smoker and a non-drinker. When the patient had femur neck fracture about a month ago, bone mineral density (BMD) was measured utilizing dual-energy X-ray absorptiometry (DXA; Hologic QDR-4500W; Hologic, Inc., Bedford, MA, USA). In result, osteoporosis was considered with T-scores of -3.9 and -3.4 in lumbar spine (L1-4) and hip, respectively (Fig. 1). Therefore, 5 mg of zoledronate (Aclasta®) was injected intravenously for 15 minutes on the day after the surgery and then calcium supplements were continuously being given until visiting the emergency room. In the blood test at the time of injecting zoledronate intravenously, serum creatinine concentration was 2.83 mg/dL and corrected calcium concentration was 8.4 mg/dL.
The patient was diagnosed intravenous zoledronate-induced hypocalcemia and then 20 mL of calcium gluconate (diluted in 100 mL of normal saline) and 1 µg/day of vitamin D (calcitriol, Bonky®) were started to inject intravenously. From the day after the intravenous injection of calcium, the patient showed gradual improvement in consciousness as well as lethargy and fatigue. However, in spite of continuous supplying of oral calcium carbonate, 3 g/day, and oral vitamin D, 0.5 µg/day, serum calcium concentration was not improved as much with 4.68 mg/dL of corrected calcium concentration in 2 weeks after the hospital visit. In the follow up examination performed in out-patient clinic after discharging from the hospital, serum creatinine concentration was 3.14 mg/dL and calcium concentration was 7.2 mg/dL (4 weeks after the symptom occurrence) and 9.3 mg/dL (4 months after the symptom occurrence) (Fig. 2).
DISCUSSION
Bisphosphonates are generally considered as safe drugs but, can be associated with laboratory abnormalities, particularly, elevated serum creatinine levels and hypocalcemia.[1] Sporadic episodes of acute and subacute renal failure have been reported, whereas hypocalcemia has not yet been the subject of detailed research.
Theoretically, intravenous bisphosphonate guarantees 100% absorption without gastrointestinal adverse effects thereby advantageous over oral bisphosphonate. Particularly, zoledronate has gained popularity as an osteoporosis treatment since its injection time (15 minutes) is shorter than that of other intravenous bisphosphonates and the injection is performed only once a year.
Maximum plasma concentrations of zoledronic acid are reached, as expected, at the end of the IV infusion. Blood levels then rapidly decline to less than 10% at four hours and to less than 1% at 24 hours after infusion. Half-life is known to be as long as 146 hours.[2] About 61% of the administered dose is taken up rapidly by bone tissue, tending to localize in areas of increased turnover rate, and is then slowly released back into the circulation. The remaining 39% is excreted unchanged via glomerular filtration by the kidneys. Zoledronic acid administration is not recommended in those with a creatinine clearance below 35 mL/min. There is no need to adjust the dose in patients who have a creatinine clearance of 35 mL/min or higher. Zoledronic acid does not inhibit the P450 enzyme, and there is therefore no interaction with other medications metabolized via cytochrome P450. However, caution should be exercised in patients on medications that have the potential of reducing the serum calcium level, such as loop diuretics and aminoglycosides, and potentially nephrotoxic medications, such as nonsteroidal anti-inflammatory drugs.
In the literature, there is well-known direct association between the risk for renal failure and drug infusion time and dose. High-dose (8 mg i.v.) with a short infusion time (5 minutes) is strongly nephrotoxic. In contrast, using the recommended infusion time and dosage (15 minutes and 4 mg i.v., respectively), this drug showed a favorable renal safety profile, comparable with that of placebo.[3,4]
Hypocalcemia is defined as a serum level of total calcium lower than 8.5 mg/dL (2.12 mmol/L). Calcium is mostly (99%) distributed in bone but serum calcium exists in three forms: (1) free or ionized calcium, the physiologically active form (50%); (2) calcium complexed to anions, including bicarbonate, lactate, phosphate, and citrate (10%); and (3) as calcium bound to plasma proteins (40%). Since approximately 80% of the protein-bound calcium fraction is associated with albumin, serum albumin can affect serum calcium level if the serum albumin is abnormally high or low. Therefore, in order to diagnose hypocalcemia accurately, serum albumin concentration should be measured first and then, based upon the measured albumin concentration calcium level should be corrected or biologically important ionized calcium concentration should be measured.
Bisphosphonates are potent inhibitors of osteoclastic bone resorption. Such inhibition reduces calcium efflux from bone, which is normally followed by a transient period of slight hypocalcemia. Most patients do not become hypocalcemic because of compensatory mechanisms, the most important of which is increased secretion of PTH.[5] If serum calcium level decreases, formation of 1,25-dihydroxyvitamin D increases due to compensatory increase of PTH. Calcium reabsorption in distal renal tubule of kidney and calcium absorption in small intestine increase thereby preventing persistent hypocalcemia. Disease states that impair these compensatory mechanisms can potentially lead to hypocalcemia after bisphosphonate use. In other words, when surgical hypoparathyroidism, hypomagnesemic hypoparathyroidism, and pre-existing secondary hyperparathyroidism are present, it can cause restriction in compensatory increase of PTH. Hypocalcemia also occurs in case of vitamin D deficiency. Moreover, the clearance of bisphosphonates is reduced in patients with impaired renal function, possibly leading to greater delivery to bone remodeling sites and to prolonged antiresorptive action. In patients with severe renal dysfunction, the combination of retained bisphosphonate and impaired intestinal calcium absorption attributable to decreased production of 1,25-dihydroxyvitamin D could potentially exaggerate the risk of developing hypocalcemia. It has been known that the potency of bisphosphonate is somewhat involved as well.[5]
The first case of bisphosphonate-associated symptomatic hypocalcemia was reported in 1987,[6] the case was associated with the use of pamidronate. And then reports of hypocalcemia associated with the use of alendronate[7] and risedronate[8] were followed. In the study performed by Conte et al.,[9] hypocalcemia was observed in 17% of patients out of 143 patients who were injected intravenously with pamidronate in order to treat bone metastasis of breast cancer, but all of them were asymptomatic. It is known that zoledronate is 100-1,000 times stronger than alendronate, risedronate, and pamidronate so that the risk of hypocalcemia is considered to be higher as well due to the strong effectiveness.
There are several studies done investigating incidence of zoledronate-induced hypocalcemia. Saad et al.[4] reported that severe hypocalcemia was exhibited in 2% of the patients and Kohno et al.[10] reported high incidence (39%) of hypocalcemia but no severe cases were present. Lyles et al.[11] reported that only 0.3% patients showed hypocalcemia and considered that this might be due to vitamin D loading before the utilization of zoledronate.
Impaired renal function and vitamin D deficiency are the most significant risk factors in hypocalcemia occurrence. Besides, hypoparathyroidism and hypomagnesemia were significant risk factors as well.[12] Furthermore, simultaneous injection of steroid, pre-existing hypocalcemia, and bone metastasis in more than 3 places had also reported as the risk factors of bisphosphonate-induced hypocalcemia.[13]
In case of the patient in our study, PTH level was elevated already. Although serum 1,25-dihydroxyvitamin D level was not measured in advance but we can guess formation of 1,25-dihydroxyvitamin D must be reduced due to impaired renal function. Then, calcium absorption in small intestine also decreased. In result, the inadequate compensatory mechanism and prolonged action of bisphosphonate caused severe hypocalcemia regardless of oral calcium supply.
Diagnosis and treatment of osteoporosis in patients with impaired renal function have not defined certainly yet. National Kidney Foundation (NKF)-Kidney Disease Outcomes Quality Initiative (K/DOQI) classifies chronic kidney disease (CKD) into 5 stages based upon degree of glomerular filtration rate (GFR) and recommends treatment and prognosis determination by each stage. Bone diseases are accompanied in many patients with CKD, called renal osteodystrophy. Renal osteodystrophy is roughly classified into 3 types; 1) high turn-over diseases with main histological finding of osteitis fibrosa caused by hyperparathyroidism, 2) low turn-over diseases including osteomalacia caused by aluminum toxicity or adynamic bone disease caused by excessive suppression of PTH, and 3) a mixed type including characteristics of both osteitis fibrosa and osteomalacia.[14] It has been known that all three types can decrease BMD and increase the risk of fractures. Therefore, in diagnosis of osteoporosis in CKD patients with decreased BMD, renal osteodystrophy should be excluded by biochemical parameters and clinical aspects, however, bone biopsy should be performed to confirm the diagnosis. If osteoporosis is diagnosed only by using examination of BMD and treated with bisphosphonate, low turn-over bone diseases could be included and get worse thereby requesting more attention.
In spite of concerns regarding the safety of bisphosphonate in CKD, some studies have also mentioned that utilization is too limited[15] because bisphosphonate is effective to decrease the risk of fractures in the patients with CKD and the frequency of side effects is quite low. Also, studies including CKD patients who had severely impaired renal function with 15 mL/min of GFR reported that alendronate[16] and risedronate[17] reduced the risk of fractures effectively without increase of side effects including nephrotoxicity.
Although it is still controversial, given the multiple literatures regarding use of bisphosphonate in CKD patients with reduced BMD,[15,18,19] in CKD stage 1-3 patients without abnormal biochemical parameters, bisphosphonate can be used as it is for the treatment in patients with normal renal function because patients in these stages represent more frequent osteoporosis, rather than renal osteodystrophy and bisphosphonate is relatively safe. In case of CKD stage 4 and 5, there are not so many studies done and frequency of renal osteodystrophy is high in these stages so that condition of each patient should be evaluated with various perspectives in order to utilize bisphosphonate. Performing bone biopsy ahead of time is the best option. Mostly, for CKD stage 4 patients with high risk of fractures, oral drugs with recommended dosage can be given and intravenous drugs can be injected 2 times slower than that of recommended injection rate. For CKD stage 5 patients with fractures, dosage of oral drugs should be reduced by half of the recommended dosage and utilized for less than 3 years and the intravenous drugs should be injected 4 times slower than that of recommended rate.
In the present case, the estimated GFR was 17 mL/min using equation of Modification of Diet in Renal Disease (MDRD) based upon serum creatinine measured at the time of femur fracture. Therefore, the patient corresponded to CKD stage 4 and high risk group since she was an elderly female patient with fracture. PTH level was 486.6 pg/mL. It is difficult to classify renal osteodystrophy based upon clinical or biochemical aspects in general, however, studies reported that low turn-over disease such as adynamic bone disease is rare before CKD stage 5 and the case with less than 150 pg/mL of PTH is useful as a parameter of low turn-over disease (sensitivity 78.1%, specificity 76.2%).[20] Based upon these results, chance to have low turn-over diseases is considered to be low in this patient so bisphosphonate treatment can be considered. However, reduction in BMD of the patient in the present case is highly considered to be caused by renal osteodystrophy rather than simple osteoporosis. As the patient showed elevated PTH level, vitamin D concentration should have been measured in advance and vitamin D and calcium should have been given. Then, more attention should have been paid on drug selection and treatment determination. If treatment with oral drugs was considered or zoledronate was injected intravenously more than 2 times slower than that of the recommended injection rate of people with normal renal function, serious hypocalcemia could have been prevented.
In conclusion, there has been no specific guideline established preventing the occurrence of hypocalcemia yet in spite of a wide range of bisphosphonate utilization. Given the many studies performed previously, when bisphosphonate is administered in the patients with osteoporosis, evaluation regarding renal function, presence or absence of vitamin D deficiency, parathyroid gland function, serum calcium, and levels of phosphorus and magnesium are needed in advance. Proper supply of calcium and vitamin D is requested in accordance with bisphosphonate injection and calcium and creatinine levels should be measured periodically. If hypocalcemia is suspicious, albumin concentration should be examined and then appropriate treatment should be carried out. In addition, when patients had impaired renal function, GFR is mandatory to calculate and the risk of fractures and presence or absence of renal osteodystrophy is required to be evaluated. Then, whether or not to inject bisphosphonate should be determined carefully.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download