Abstract
Root canal anatomy is complex, and the recognition of anatomic variations could be a challenge for clinicians. This case report describes the importance of cone beam computed tomographyic (CBCT) imaging during endodontic treatment. A 23 year old woman was referred by her general dental practitioner with the chief complaint of spontaneous pain in her right posterior maxilla. From the clinical and radiographic findings, a diagnosis of symptomatic irreversible pulpitis was made and endodontic treatment was suggested to the patient. The patient underwent CBCT examination, and CBCT scan slices revealed seven canals: three mesiobuccal (MB1, MB2, and MB3), two distobuccal (DB1 and DB2), and two palatal (P1 and P2). Canals were successfully treated with reciprocating files and filled using single-cone filling technique. Precise knowledge of root canal morphology and its variation is important during root canal treatment. CBCT examination is an excellent tool for identifying and managing these complex root canal systems.
A comprehensive understanding of the complexity of root canal systems is imperative for successful root canal treatment.123 Recognition of anatomic variations is a real challenge for clinicians before undertaking therapy, regardless of the teeth that are to be treated. Maxillary first molars have been frequently investigated because of their complex root anatomy and canal morphology.456 Based on the published results, it is generally accepted that most maxillary first molars have 3 roots and 4 canals.456 Most studies reported incidences of a second canal in the mesiobuccal root in over 50% of the cases.456 Additional anatomic variations include distobuccal and palatal roots with more than 1 canal totalizing 5 root canals, as well as C-shaped canals.45678
Case reports with more than 6 root canals are not unusual. In contrast, maxillary first molars with more than 6 canals are rare, and only few cases have been reported in endodontic literature (Table 1).789101112131415 We present here a rare case report of a maxillary first molar with 7 separate canals: 3 canals in the mesiobuccal root, 2 canals in the distobuccal root, and 2 canals in the palatal root.
A 23 year old woman was referred by her general dental practitioner to the Department of Endodontics, Health Science Institute, Faculdades Unidas do Norte de Minas (FUNORTE), with the chief complaint of spontaneous pain in her right posterior maxilla for 3 days. The patient medical history was unremarkable and non-contributory. A clinical examination revealed extensive restoration in the maxillary right first molar, which was tender to percussion. Palpation of the buccal and palatal aspect of the tooth did not reveal any tenderness. The tooth was not mobile and periodontal probing around the tooth was within physiological limits. Vitality testing of the involved tooth with Endo Ice (Coltene/Whaledent GmbH+ Co. KG, Langenau, Germany) caused an intense lingering pain. A preoperative radiograph revealed restoration approaching the pulp space (Figure 1a). From the clinical and radiographic findings, a diagnosis of symptomatic irreversible pulpitis with symptomatic apical periodontitis was made, and endodontic treatment was suggested to the patient. The patient's consent form was obtained.
The radiographic evaluation of the involved tooth did not indicate any variation in the canal anatomy (Figure 1a). The tooth was anesthetized using 1.8 mL 2% lidocaine with 1:100,000 epinephrine (DFL, Rio de Janeiro, Brazil). Then rubber dam isolation was performed and endodontic access cavity was established using high-speed diamond round and Endo-Z burs (Dentsply Maillefer, Konstanz, Germany). Clinical examination revealed three canal openings in the mesiobuccal root, two in the distobuccal root, and one in the palatal root (Figure 1b).
In order to evaluate this unusual morphology, the patient underwent cone beam computed tomographic (CBCT) examination. An informed consent was obtained from the patient, and a CBCT scan of the maxilla was performed (Eagle 3D CBCT unit, Dabi Atlante, São Paulo, Brazil). The involved tooth was focused, and the morphology was obtained in transverse, axial, and sagittal sections of 0.5 mm thickness. CBCT scan slices revealed seven canals: three mesiobuccal (MB1, MB2, and MB3), two distobuccal (DB1 and DB2), and two palatal (P1 and P2) canals in the right maxillary first molar (Figure 1c). Surprisingly, in the palatal root, a Vertucci's type VI configuration (two separate canals leaving the pulp chamber, merging in the body of the root, and re-devising short of the apex to exit as two distinct canals) was found (Figure 1d).16
At the second appointment, the tooth was anesthetized using 1.8 mL 2% lidocaine with 1:100,000 epinephrine (DFL), cleaning and shaping was performed under rubber dam isolation using R25 Reciproc file (VDW, Munich, Germany) used in a reciprocating with slow in-and-out pecking motion according to the manufacturer's instructions, and continuous irrigation with 2.5% sodium hypochlorite solution and 17% EDTA and bidistilled water as the final irrigant. The canals were dried with absorbent paper points (VDW), and were then obturated with the single-cone obturating technique using complementing gutta-percha points (VDW) in each canal and AH Plus sealer (Dentsply Maillefer) (Figures 1e - 1g).
The tooth was then restored with a composite resin core (Filtek Z350, 3M ESPE, St. Paul, MN, USA). The patient was advised of a full-coverage porcelain crown, and the tooth was asymptomatic during the follow-up period of 1 year (Figure 1h).
This case describes a maxillary first molar with three mesiobuccal (MB1, MB2, and MB3), two distobuccal (DB1 and DB2), and two palatal (P1 and P2) canals. Anatomic variations are not uncommon in maxillary first molars, and additional canals in the distobuccal and palatal roots have been reported in the literature; however, case reports with more than 6 canals are not usual and only few cases have been previously published.9101112131415 Diagnosis and management of these complexities present an endodontic challenge, and failure to identify and treat these extra canals can negatively influence treatment outcome. In these cases, careful examination of preoperative image exams can be helpful.3789 Periapical radiographs taken in different angulations are an essential part of endodontic treatment for the identification of root and canal configuration. However, the amount of information gained from periapical radiographs is limited by the fact that radiographs are compressed 2 dimensional image of a 3 dimensional object, and this may be the reason the radiographic evaluation of the tooth did not indicate any aberration in the canal anatomy.
In the present case, after identifying an unusual anatomy through clinical examination, the patient underwent CBCT examination. CBCT has been used in several areas of dentistry since it shows the dental structures in a threedimensional view, as well as it offers clear structural images with high contrast. CBCT imaging confirmed the presence of three mesiobuccal and two distobuccal canals, observed during clinical examination and also identified two palatal canals, not observed clinically.
Several studies showed the quality of CBCT imaging and its clinical application for studying root canal morphology before clinical endodontic treatment.3789 Yet, the use of CBCT imaging should be indicated only in cases in which complex anatomy and/or morphology is suspected. Although minimal, CBCT imaging still uses ionizing radiation. Therefore, endodontic cases should be judged individually, and patients should always be exposed to the least amount of radiation that is possible to gain the most useful information for proper diagnosis. In cases in which an unexpected complex anatomy is visualized after access or when canals are not found, intraoperative CBCT imaging is always an excellent possibility as recently proposed by Ball et al.17
Single-cone obturation is considered a simple technique that improves practice and cause less stress for clinician and patient. The use of a single cone that match the geometry of nickel-titanium instrumentation systems allows a good adaptation of gutta-percha to canal walls and only little space remains between gutta-percha and the canal wall, which is filled by root canal sealer. Several previous studies that compared single-cone technique to other root canal filling techniques reported similar sealing ability and leakage at coronal and apical area.181920 Therefore, we decided to use this technique in the present case report.
Post-obturation radiographic evaluation immediately after root canal obturation is necessary to assess the apical sealing, condensation, and containment of the root canal filling material within the root canal system. Several intraoral views at different horizontal angulations may be necessary for complex root canal configuration so that all the gutta-percha points will be evaluated in relation to the apex.21 However, it should be noted that multiple intraoral radiographs at different angulations do not guarantee the identification of all relevant anatomy and may not reveal much more than a single exposure. Depending on the x-ray beam angulation and tooth position, even an improper root canal treatment with insufficient condensation and adaptation can be assumed appropriate.22 The American Association of Endodontists (AAE) and American Academy of Oral and Maxillofacial Radiology (AAOMR) joint position statement regarding the use of CBCT in Endodontics does not recommend the use of CBCT for immediate postoperative imaging.23 However, it is important to emphasize that this case report does not have an usual root canal anatomy. As described previously, maxillary molars with 7 root canals is not commonly observed. For this reason, a post-obturation CBCT scan was performed in this case which facilitated the assessment of the integrity of root canal fillings, always keeping in mind the As Low As Reasonably Achievable (ALARA) protocol and the evidenced based data. The use of CBCT imaging in limited field of view may actually reduce the potential radiation exposure of the patient during the course of endodontic treatment. This technology can provide images of several teeth in single exposure with approximately the same radiation dose as 4 to 5 periapical radiographs (100 mSv and 86 - 107.5 mSv, respectively), and they may provide a dose savings over multiple traditional images in complex cases.
Lack of knowledge about accurate anatomical configurations of the root canals may lead dentists to leave remaining necrotic tissue, toxic products, and microorganisms in nontreated missing canals, resulting in an unsuccessful endodontic treatment. CBCT is an important technological resource which will definitely be helpful in identifying and treating all the root canals successfully.
Figures and Tables
Figure 1
(a) A preoperative radiograph of the right maxillary first molar; (b) Clinical view of access cavity and 7 root canals; (c and d) Cone beam computed tomographic (CBCT) images of right maxillary first molar showing 3 roots and 7 canals; (e - g) Post-filling CBCT images of the right maxillary first molar; (h) One-year follow-up x-ray. MB, mesiobuccal canal; DB, distobuccal canal; P, palatal canal.

Table 1
Variations of canal configuration reported in maxillary molars with 7 or more canals
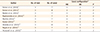
| Author | No. of root | No. of canal | Canal configuration* | ||
|---|---|---|---|---|---|
| MB | DB | P | |||
| Kotoor et al. (2010)7 | 3 | 7 | 3 | 2 | 2 |
| Kotoor et al. (2011)8 | 3 | 8 | 3 | 3 | 2 |
| Badole et al. (2014)9 | 3 | 7 | 3 | 2 | 2 |
| Raghavendra et al. (2014)10 | 3 | 7 | 3 | 2 | 2 |
| Martins (2014)11 | 3 | 7 | 4 | 2 | 1 |
| Kumar (2014)12 | 3 | 7 | 3 | 2 | 2 |
| Almeida et al. (2015)13 | 3 | 8 | 3 | 3 | 2 |
| Nayak et al. (2015)14 | 3 | 7 | 3 | 3 | 1 |
| Munavalli et al. (2015)15 | 3 | 7 | 3 | 2 | 2 |
References
1. Ida RD, Gutmann JL. Importance of anatomic variables in endodontic treatment outcomes: case report. Endod Dent Traumatol. 1995; 11:199–203.

2. Lin LM, Pascon EA, Skribner J, Gängler P, Langeland K. Clinical, radiographic, and histologic study of endodontic treatment failures. Oral Surg Oral Med Oral Pathol. 1991; 71:603–611.

3. Jain D, Reddy S, Vanigalla BS, Kamishetty S. Endodontic management of a mandibular first molar with six root canal systems. J Conserv Dent. 2015; 18:419–422.

4. Neelakantan P, Subbarao C, Ahuja R, Subbarao CV, Gutmann JL. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod. 2010; 36:1622–1627.

5. Lee JH, Kim KD, Lee JK, Park W, Jeong JS, Lee Y, Gu Y, Chang SW, Son WJ, Lee WC, Baek SH, Bae KS, Kum KY. Mesiobuccal root canal anatomy of Korean maxillary first and second molars by cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 111:785–791.

6. Silva EJ, Nejaim Y, Silva AI, Haiter-Neto F, Zaia AA, Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. J Endod. 2014; 40:173–176.

7. Kottoor J, Velmurugan N, Sudha R, Hemamalathi S. Maxillary first molar with seven root canals diagnosed with cone-beam computed tomography scanning: a case report. J Endod. 2010; 36:915–921.

8. Kottoor J, Velmurugan N, Surendran S. Endodontic management of a maxillary first molar with eight root canal systems evaluated using cone-beam computed tomography scanning: a case report. J Endod. 2011; 37:715–719.

9. Badole GP, Warhadpande MM, Shenoi PR, Lachure C, Badole SG. A rare root canal configuration of bilateral maxillary first molar with 7 root canals diagnosed using cone-beam computed tomographic scanning: a case report. J Endod. 2014; 40:296–301.

10. Raghavendra SS, Hindlekar AN, Desai NN, Vyavahare NK, Napte BD. Endodontic management of maxillary first molar with seven root canals diagnosed using cone beam computed tomography scanning. Indian J Dent. 2014; 5:152–156.

11. Martins JN. Endodontic treatment of a maxillary first molar with seven root canals confirmed with cone beam computer tomography - case report. J Clin Diagn Res. 2014; 8:ZD13–ZD15.
12. Kumar R. Report of a rare case: a maxillary first molar with seven canals confirmed with cone-beam computed tomography. Iran Endod J. 2014; 9:153–157.
13. Almeida G, Machado R, Sanches Cunha R, Vansan LP, Neelakantan P. Maxillary first molar with 8 root canals detected by CBCT scanning: a case report. Gen Dent. 2015; 63:68–70.
14. Nayak G, Singh KK, Shekhar R. Endodontic management of a maxillary first molar with three roots and seven root canals with the aid of cone-beam computed tomography. Restor Dent Endod. 2015; 40:241–248.

15. Munavalli A, Kambale S, Bandekar S, Ajgaonkar N. Maxillary first molar with seven root canals diagnosed with cone-beam computed tomography scanning. Indian J Dent Res. 2015; 26:82–85.

16. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984; 58:589–599.

17. Ball RL, Barbizam JV, Cohenca N. Intraoperative endodontic applications of cone-beam computed tomography. J Endod. 2013; 39:548–557.

18. Wu MK, van der Sluis LW, Wesselink PR. A 1-year follow-up study on leakage of single-cone fillings with RoekoRSA sealer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:662–667.

19. Wu MK, Bud MG, Wesselink PR. The quality of single cone and laterally compacted gutta-percha fillings in small and curved root canals as evidenced by bidirectional radiographs and fluid transport measurements. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:946–951.

20. Yilmaz Z, Tuncel B, Ozdemir HO, Serper A. Microleakage evaluation of roots filled with differene obturation techniques and sealers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:124–128.

21. Barton DJ, Clark SJ, Eleazer PD, Scheetz JP, Farman AG. Tuned-aperture computed tomography versus parallax analog and digital radiographic images in detecting second mesiobuccal canals in maxillary first molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 96:223–228.

22. Kersten HW, Wesselink PR, Thoden Van Velzen SK. The diagnostic reliability of the buccal radiograph after root canal filling. Int Endod J. 1987; 20:20–24.

23. Special Committee to revise the Joint AAE/AAOMR position statement on use of CBCT in Endodontics. AAE and AAOMR Joint position statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 120:508–512.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download