Abstract
X-linked hypophosphatemia (XLH) is a hereditary metabolic disease caused by the loss of phosphate through the renal tubules into the urine, and an associated decrease in serum calcium and potassium phosphate. Its dental features include spontaneous dental abscesses that occur in the absence of trauma or dental caries. The aim of this case report was to describe the dental problems of XLH patients and to evaluate limitations in their treatment. A 14 year old male and a 38 year old female with XLH were referred to the Department of Conservative Dentistry for endodontic treatment. The dental findings were periapical abscesses without obvious trauma or caries. Conservative endodontic treatment was performed in teeth with pulp necrosis and abscess. In case 1, the treated teeth showed improvements in bone healing, without clinical symptoms. However, in case 2, the implants and the treated tooth showed hypermobility, and the final restoration was therefore postponed. Early diagnosis, periodic examinations, and communication with the patient's pediatrician are important in the dental management of patients with XLH.
Hypophosphatemic vitamin D-resistant rickets is a metabolic disorder involving decreased levels of calcium and potassium phosphate due to the abnormal excretion of phosphate from the kidneys. It is the most common heritable form of rickets.12 The various forms of hereditary hypophosphatemic rickets are distinguished by patterns of inheritance and the genetic cause, and autosomal dominant, autosomal recessive, and X-linked dominant forms have been identified.3 The X-linked dominant form is the most common.4
Untreated X-linked hypophosphatemia (XLH) is associated with growth retardation and skeletal deformities. The signs and symptoms of XLH include bowed legs due to the body load, immature skeletal bone calcification, elevated risk of bone fractures, enlargement of the costal cartilage, compression of the spinal cord (spinal stenosis), short stature, thickening of the wrists and ankles, beading of the ribs known as rachitic rosary, and thickening of the frontal and parietal bones, which produces frontal bossing that leads to a square-shaped head.56
Dental alterations and delays in eruption are found in both the deciduous and permanent teeth of XLH patients. On radiographs, XLH is associated with osseous structure deformities, such as a thin bony trabecular pattern and the complete or partial absence of the lamina dura.7 The teeth show shortened roots, enlarged pulp chambers, and prominent pulp horns.89 Histological examinations show slightly hypoplastic enamel morphology.1011 Large tubular clefts or lacunae extending up to the dentinoenamel junction are detected in histological studies of the dentin. Dentin mineralization is a process of growth and fusion of calcospherites. The lack of fusion of calcospherites in the circumpulpal dentin results in a large interglobular space filled with non-mineralized organic matrix in hypophosphatemic patients.23101213 Invasion of bacteria into the pulp is facilitated even in the absence of dentin matrix destruction, resulting in spontaneous dental abscesses. Periapical abscesses without caries or a history of traumatic injuries are considered a characteristic dental finding in XLH patients.2 This article describes the problems and limitations of dental treatment in XLH patients.
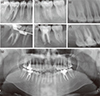
A 14 year old boy was referred from the Department of Pediatric Dentistry to the Department of Conservative Dentistry at Chonnam National University Dental Hospital for evaluation and treatment of the lower right first molar. It was reported that the patient had XLH. Since diagnosis at the age of approximately 1 year, the patient had been undergoing basic therapy for the replacement of phosphate and calcium. At the age of 1, he underwent an operation for cleft palate and lip. Orthodontic treatment was initiated when the patient was 10 years old and had continued since. On physical examination, the patient exhibited a short height and an abnormality of the lower extremities characterized by bowing of the legs. He also had prominent frontal bossing and thorax. In an intraoral examination, he showed Class III malocclusion, and a congenitally missing upper left lateral incisor (tooth #22). A sinus tract was present on the buccal gingiva of the lower right first molar (tooth #46), which appeared to be a normal tooth otherwise, without any carious lesions or history of trauma. On radiographs, slightly enlarged radicular canals and pulp chambers, delayed apical closure, and periradicular radiolucencies were observed on tooth #46 (Figure 1a). A radiograph with gutta-percha cone tracing indicated that tooth #46 was the origin of the sinus tract (Figure 2a). Microscopic observation (Carl Zeiss Surgical GmbH, Carl Zeiss, Oberkochen, Germany) confirmed that no crack was present. Based on these findings, the right mandibular first molar was diagnosed as having a chronic periapical abscess, and the decision was made to perform conventional root canal treatment.
After obtaining informed consent, the endodontic procedure was initiated. Under rubber dam isolation, an access cavity was prepared. The necrotic pulp tissue was removed and the working length was established with an apex locator (DentaPort ZX, J Morita USA, Irvine, CA, USA) and the conventional radiographic method. Four canals were cleaned and shaped using nickel-titanium rotary instruments (ProTaper, Dentsply Tulsa Dental, Tulsa, OK, USA) with a crown-down technique and enlarged to the size of a No. F2. During instrumentation, copious irrigation was performed using 5.25% sodium hypochlorite solution and sterile saline. Sterile paper points were used to dry the canals, and a closed dressing was put in place with a sterilized cotton pellet and Caviton (GC, Tokyo, Japan) in the pulp chamber. At the sixth appointment (approximately 2 months later), the gingival sinus tract disappeared, but weeping canals were noted. A calcium hydroxide dressing was put in place for 3 months, and the canals were obturated using a continuous wave technique with gutta-percha and AH26 plus (Dentsply DeTrey, Konstanz, Germany) (Figure 2d).
After 2 years and 8 months, the patient visited our department again due to pain in the lower left first molar (tooth #36). The clinical examination revealed swelling and tenderness of tooth #36. The tooth responded to percussion, but not to the electric pulp test. Microscopic observation (Carl Zeiss Surgical GmbH) confirmed that no crack was present. Tooth #36 was diagnosed as having an acute apical abscess, and root canal therapy was performed (Figures 2b and 2e). Three months later, he visited our department for pain in the upper right first molar (tooth #16). Although the symptom was similar to that experienced with tooth #46, tooth #16 showed a positive response to the electric pulp test, but at a higher threshold than the adjacent teeth, and a delayed pain response to the cold test. Tooth #16 was diagnosed as having irreversible pulpitis, and root canal therapy was performed.
When the patient was between 14 and 17 years of age, he regularly experienced spontaneous abscesses in the first molar area. Each tooth was sound, with no caries, cracks, or history of dental trauma. The cause of the spontaneous abscesses was considered to be excessive contact with the Frankel III appliance. The patient stopped wearing the Frankel III appliance, and wore a sagittal appliance anchored on the upper canines and molars. After 3 months of wearing a sagittal appliance, he visited our department for cold sensitivity in the upper canines and premolars. We doubted that the teeth were cracked, and we decided to perform follow-up and observe the patient's symptoms. After 3 months, the upper right canine did not respond to the electric pulp test. This tooth was diagnosed with pulp necrosis, and root canal therapy was performed. The patient was put on periodic recall to observe the progress of all his teeth.
A 38 year old female was referred to the Department of Conservative Dentistry at Chonnam National University Dental Hospital for pain control on the upper right side while biting. She had received medical therapy since being diagnosed with XLH at the age of 2 years. She underwent 2 corrective operations for her legs at the age of 32 years. She reported that she had stopped taking medication due to pregnancy and breastfeeding. A physical examination demonstrated a short height and abnormalities of the cranium (flattening of the cranium and prominent frontal bossing) and the lower extremities, which were characterized by bowing of the legs. An intraoral examination showed the absence of caries, dental abrasions, and periodontal inflammation. A radiographic examination showed ample radicular canals, pulp chambers, and pulp horns. General alveolar bone loss causing tooth mobility was observed (Figure 3). In the clinical examination, the upper right second premolar (tooth #15) was responsive to percussion and nonresponsive to the electric pulp test. Microscopic observation (Carl Zeiss Surgical GmbH) confirmed that no crack was present. The tooth was diagnosed with acute apical periodontitis and root canal therapy was performed (Figure 4).
Under rubber dam isolation, an access cavity was prepared. The pulp tissue was removed and the working length was established with an apex locator (DentaPort ZX) and the radiographic method. Two canals were cleaned and shaped using ProTaper NiTi rotary instruments with a crown-down technique. During instrumentation, copious irrigation was performed using 5.25% sodium hypochlorite solution and sterile saline. The canals were dried and calcium hydroxide was applied as a medicament for a month. The access cavity was temporarily sealed with Caviton (GC). After 1 month, the canals were filled with gutta-percha and AH26 plus (Dentsply DeTrey) using a continuous wave technique. After root canal therapy, she complained of discomfort during biting.
In this patient, implants were placed after the extraction of the upper right and left central incisors due to hypermobility and discomfort, as was the case for the upper right second premolar. Since the implants showed consistent hypermobility after 1 year and 6 months of implant installation, the final restorations were postponed.
XLH is the most common heritable form of vitamin-D resistant rickets. XLH is a disorder of the kidney, in which renal defects lead to reduced phosphate reabsorption in the glomerular filtration system of the proximal renal tubules. This deficiency leads to hypophosphatemia and hyperphosphaturia, resulting in in bone and dental abnormalities.713 The phosphate-regulating gene with homologies to endopeptidases on the X chromosome (PHEX), located on Xp22.1, has been identified as the gene defective in XLH.1415 PHEX is expressed in osteoblasts, osteocytes, odontoblasts, and the parathyroid gland. Inactivating mutations in PHEX activity may be involved in skeletal and dental abnormalities.11
In case 1, the patient's teeth had large pulp chambers and thin dentinal walls, but a generally normal tooth structure. The first symptom of this patient appeared at the age of 14 years, when he underwent orthodontic treatment for a dentinal cleft. It was thought that the cause of abscesses on the lower right first molar was excessive contact with the orthodontic appliance. Once he stopped wearing the orthodontic appliance, no further symptoms occurred in that molar. However, changing the orthodontic appliance led to symptoms in different teeth. It is believed that this symptom was caused by traumatic forces to the teeth due to excessive contact with the orthodontic appliance. These symptoms are thought to have resulted from the following sequence of events: undesired heavy forces → pulp hyperemia → pulpitis → transient apical breakdown with periapical lesion (still reversible through revitalization) → pulp necrosis → apical periodontitis. Therefore, for a patient with this condition, the prevention of trauma is extremely important.
The patient in case 1 had received neutral phosphate as a medication since the age of 1 year. However, the patient in the case 2 had stopped taking medication due to pregnancy and breastfeeding. She stated that the upper right and central incisor were extracted due to hypermobility of the teeth and discomfort during pregnancy, and then implants were placed after giving birth. When she presented to the Department of Conservative Dentistry at Chonnam National University Dental Hospital due to discomfort in the upper right second premolar, she was not taking any medication due to breastfeeding. Although it is common to complete the final prosthetic restoration between 6 months and 1 year, the implants showed consistent hypermobility 1 year and 6 months after implant installation. The hypermobility of several teeth in this patient may have been due to the interruption of medication.
Perforation is very likely in teeth with thin and weak dentinal walls. Preparation and instrumentation should be performed carefully during endodontic treatment. In addition, chemical irrigation is preferred to mechanical instrumentation.4 Implant installation is not absolutely contraindicated for patients with XLH. A case study of successful implant installation with guided bone regeneration in XLH patients has been reported.16 However, uncertain prognoses are possible, as in the patient in case 2 who underwent implant installation after extraction. Some studies have reported that the interruption of medication in XLH patients may have a negative influence on bone healing.1718 Blood calcium and phosphate concentrations in XLH patients should be monitored carefully before periodontal surgery.
Patients with XLH may frequently experience dental caries or attrition, and bacteria can easily invade the dental pulp through defects in the enamel and dentin, resulting in pulpitis. Consequently, to prevent dental abscesses, the early treatment of disease and the preventive treatment of caries and attrition are essential. In the deciduous dentition, prefabricated metal or polycarbonate crowns have been suggested to be useful in the prevention of attrition and enamel cracks.1920 However, not all the pulp is infected, and iatrogenic pulp infection could take place during tooth preparation, so this preventive treatment should not be performed in all patients with XLH. In patients with XLH, it is important to maintain good oral hygiene with professional dental care.21 Dentists are recommended to provide information about the dental signs and symptoms of XLH to pediatricians. Both dentists and pediatricians should recognize the dental features of XLH, so that early preventive interventions can help avoid serious and invasive dental procedures.
Figures and Tables
Figure 2
Radiographs of the patient in case 1. Preoperative (a) and postoperative (d) radiographs of the lower right first molar. Preoperative (b) and postoperative (e) radiographs of the lower left first molar. Preoperative (c) and postoperative (f) radiographs of the upper right first molar. Postoperative panoramic view (g).
Acknowledgement
This study was supported by a grant (CRI 15017-1) from the Chonnam National University Hospital Biomedical Research Institute and a National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No. 2016R1C1B1012703).
References
1. Moreland LW. Rheumatology and immunology therapy (A to Z essentials): hypophosphatemic vitamin D resistant rickets. Springer;2004. p. 428.
2. Beltes C, Zachou E. Endodontic management in a patient with vitamin D-resistant rickets. J Endod. 2012; 38:255–258.

3. Souza MA, Soares Junior LA, Santos MA, Vaisbich MH. Dental abnormalities and oral health in patients with Hypophosphatemic rickets. Clinics(Sao Paulo). 2010; 65:1023–1026.

4. Pereira CM, de Andrade CR, Vargas PA, Coletta RD, de Almeida OP, Lopes MA. Dental alterations associated with X-linked hypophosphatemic rickets. J Endod. 2004; 30:241–245.

5. Thomas MK, Demay MB. Vitamin D deficiency and disorders of vitamin D metabolism. Endocrinol Metab Clin North Am. 2000; 29:611–627.

6. Feng JQ, Clinkenbeard EL, Yuan B, White KE, Drezner MK. Osteocyte regulation of phosphate homeostasis and bone mineralization underlies the pathophysiology of the heritable disorders of rickets and osteomalacia. Bone. 2013; 54:213–221.

7. Koehne T, Marshall RP, Jeschke A, Kahl-Nieke B, Schinke T, Amling M. Osteopetrosis, osteopetrorickets and hypophosphatemic rickets differentially affect dentin and enamel mineralization. Bone. 2013; 53:25–33.

8. Murayama T, Iwatsubo R, Akiyama S, Amano A, Morisaki I. Familial hypophosphatemic vitamin D-resistant rickets: dental findings and histologic study of teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90:310–316.

9. Chaussain-Miller C, Sinding C, Septier D, Wolikow M, Goldberg M, Garabedian M. Dentin structure in familial hypophosphatemic rickets: benefits of vitamin D and Dental management in X-linked hypophosphatemia phosphate treatment. Oral Dis. 2007; 13:482–489.

10. Zambrano M, Nikitakis NG, Sanchez-Quevedo MC, Sauk JJ, Sedano H, Rivera H. Oral and dental manifestations of vitamin D-dependent rickets type I: report of a pediatric case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:705–709.

11. Baroncelli GI, Angiolini M, Ninni E, Galli V, Saggese R, Giuca MR. Prevalence and pathogenesis of dental and periodontal lesions in children with X-linked hypophosphatemic rickets. Eur J Paediatr Dent. 2006; 7:61–66.
12. Douyere D, Joseph C, Gaucher C, Chaussain C, Courson F. Familial hypophosphatemic vitamin D-resistant rickets-prevention of spontaneous dental abscesses on primary teeth: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:525–530.

13. Opsahl Vital S, Gaucher C, Bardet C, Rowe PS, George A, Linglart A, Chaussain C. Tooth dentin defects reflect genetic disorders affecting bone mineralization. Bone. 2012; 50:989–997.

14. Holm IA, Nelson AE, Robinson BG, Mason RS, Marsh DJ, Cowell CT, Carpenter TO. Mutational analysis and genotype-phenotype correlation of the PHEX gene in X-linked hypophosphatemic rickets. J Clin Endocrinol Metab. 2001; 86:3889–3899.

15. Imel EA, Gray AK, Padgett LR, Econs MJ. Iron and fibroblast growth factor 23 in X-linked hypophosphatemia. Bone. 2014; 60:87–92.

16. Resnick D. Implant placement and guided tissue regeneration in a patient with congenital vitamin D-resistant rickets. J Oral Implantol. 1998; 24:214–218.

17. Mäkitie O, Doria A, Kooh SW, Cole WG, Daneman A, Sochett E. Early treatment improves growth and biochemical and radiographic outcome in X-linked hypophosphatemic rickets. J Clin Endocrinol Metab. 2003; 88:3591–3597.

18. Carpenter TO, Insogna KL, Zhang JH, Ellis B, Nieman S, Simpson C, Olear E, Gundberg CM. Circulating levels of soluble klotho and FGF23 in X-linked hypophosphatemia: circadian variance, effects of treatment, and relationship to parathyroid status. J Clin Endocrinol Metab. 2010; 95:E352–E357.

19. Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL. A clinician's guide to X-linked hypophosphatemia. J Bone Miner Res. 2011; 26:1381–1388.

20. Tumen EC, Yavuz I, Tumen DS, Atakul F. Dental and histologic findings of X-linked hypophosphataemic vitamin D-resistant rickets: a case report. Int Dent Med Disord. 2008; 1:37–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download