Abstract
Objectives
This study aimed to evaluate the healing rate of non-surgical endodontic treatment between C-shaped and non-C-shaped mandibular second molars.
Materials and Methods
Clinical records and radiological images of patients who had undergone endodontic treatment on mandibular second molars between 2007 and 2014 were screened. The periapical index scoring system was applied to compare healing outcomes. Information about preoperative and postoperative factors as well as the demographic data of the patients was acquired and evaluated using chi-square and multinomial logistic regression tests.
Results
The total healing rate was 68.4%. Healing rates for the mandibular second molar were 70.9% in C-shaped canals (n = 79) and 66.6% in non-C-shaped ones (n = 117). The difference was not statistically significant.
Conclusions
The presence of a C-shaped canal in the mandibular second molar did not have a significantly negative effect on healing after treatment. Instead, proper pulpal diagnosis and final restoration were indicated as having significantly greater influence on the healing outcomes of C-shaped and non-C-shaped canals, respectively.
A thorough understanding of root canal anatomy and its variation plays a very important role in carrying out successful endodontic treatment. To advance our knowledge about root canal anatomy, many studies have reported different kinds of root canal morphologies, one of which is a C-shaped root canal.123 The C-shaped root canal, first named by Cooke and Cox in 1979, is an unusual variation of canal morphology.4 Although clinical cases have reported a C-shaped root canal in the maxillary and mandibular first molar, it is primarily found in the mandibular second molar.5 Studies have mapped the incidence of a C-shaped root canal in different populations. It shows an increasing tendency from Northeast Africa to East Asian countries such as China, Korea, and Japan.67
Because of the unusual morphology and structural complexity of a C-shaped root canal, many technologies have been recommended to facilitate successful endodontic treatment. For example, some studies have proposed the use of ultrasonic equipment in combination with a nickel-titanium (NiTi) rotary instrument for effective cleaning89 and the use of a continuous wave technique, instead of cold lateral compaction, for achieving fillings with greater density.10 Nonetheless, a C-shaped root canal is generally believed to complicate endodontic treatment and might have an unfavorable effect on healing outcomes. Although this belief is based on the complexity of the C-shaped root canal, there are no studies that directly compare the healing rates of endodontic treatment between C-shaped and non-C-shaped root canals.
This study aims to evaluate the healing rate of non-surgical root canal treatment between C-shaped and non-C-shaped mandibular second molars. In addition, this study aims to identify factors that significantly affect treatment outcome.
The protocol of this study was approved by the Institutional Review Board of Wonkwang University Daejeon Dental Hospital (W1406/001-001). This study included patients who received endodontic treatment on mandibular second molars from 2007 to 2014 at the Department of Conservative Dentistry of Wonkwang University Daejeon Dental Hospital (Daejeon, Korea).
Mandibular second molars treated with endodontic retreatment or surgical treatment like intentional replantation and cases with a follow-up period shorter than 6 months were excluded. Patients with a notable medical history, including conditions such as diabetes, cancer, chemotherapy, HIV infection, or other immunocompromising disease, were also excluded.
Endodontic treatments were performed under rubber dam isolation, with a straight-line access prepared using diamond high-speed burs. Then the coronal third of the canal was enlarged with Gates-Glidden burs at low speed. The working length (WL) was determined with Root ZX (J. Morita Corp., Tokyo, Japan) and periapical radiography. The apical third was then prepared using ProTaper NiTi files (Dentsply Tulsa Dental, Tulsa, OK, USA) and Profile NiTi files (Dentsply Tulsa Dental). Five mL sodium hypochlorite at 2.5% was used as an irrigant. Compacted warm gutta-percha cones (DiaDent, Cheongwon, Korea) and AH Plus (Dentsply Tulsa Dental) sealer filled the canals. A final radiograph was exposed after removal of the rubber dam.
The personal details (including age at the time of last follow-up and sex) of 195 patients were recorded. Information about the involved tooth, including the location of the tooth, the presence of a C-shaped canal, pulpal and periapical status like vital or nonvital pulp, normal or pathologic periapex, and the presence of cracks or fractures, was collected to determine the set of preoperative factors. The restorative status of the tooth such as the presence of full-coverage restoration was also noted as a postoperative factor.
At the initial visit and at every follow-up visit, patients were asked about tooth pain (spontaneous, or upon chewing or with pressure) and the tooth was then examined clinically and radiographically. Radiographs were taken using the paralleling technique. The exposure time for each tooth type was standardized. Radiographic evaluation was performed preoperatively and postoperatively, at the endpoint of follow-up visits, double-blind, by two additional examiners. Before evaluating the radiographs, the two examiners were calibrated with well-defined instructions and reference radiographs with different periapical types of lesions. When the two examiners disagreed, the radiograph was subjected to joint evaluation. Irrespective of the number of treated roots, the tooth was always considered as the unit of evaluation and rated according to the worst value.
The presence of a C-shaped root canal was identified on radiographs using the radiographic features recommended by Fan et al.11 Mandibular second molars having a conical or square root whose canals are merged into 1 major canal or separated by a radiolucent longitudinal separating line were recognized as C-shaped.11 These were also confirmed by clinical inspection during endodontic treatment for the identification of C-shaped canals.
For radiographic evaluation, periapical and panoramic views were used. PAI scoring system was used to compare the differences in periapical status before and after treatment at the last follow-up point. With this method, periapical radiolucencies are scored on a 5 point scale ranging from 1 to 5: score 1 represents a radiographically healthy periapex; score 2 is a small change in periapical bone structure (< 0.5 mm); score 3 denotes changes in periapical bone structure with some mineral loss (0.5 - 1 mm); score 4 is demineralization of the periapical bone with a well-defined radiolucent area (2 - 4 mm); score 5 represents demineralization of the periapical bone with exacerbating features (≥ 5 mm).1213 In multi-rooted teeth, the scoring was assigned to the root with the highest PAI score.
In studies on endodontic outcomes, the criteria for healing were based on clinical symptoms and radiographic findings. Four categories were used for the classification of healing following endodontic treatment. These criteria were modified from the three categories presented by Dammaschke et al., which classified healing following endodontic treatment into complete healing, incomplete healing, and no healing.14 Details of radiographic changes for the modified four criteria are based on the PAI scoring system (Table 1). Completely and incompletely healed are considered as healed, while uncertain and unsatisfactory healing belongs to the non-healing category.
All data were analyzed using IBM SPSS Statistics for Windows version 21.0 software program (IBM Corp., Armonk, NY, USA). To differentiate the demographic characteristics of selected patients, an analysis of frequency was done. In order to evaluate the effect of the identified factors on the healing outcome, chi-square analysis and regression analysis were used. Multinomial logistic regression was also chosen to predict the possibilities of different potential healing outcomes. All the statistical tests were set at 95% significance level (p < 0.05).
The demographic data distribution of this study is shown in Table 2. A total of 330 patients were treated with non-surgical root canal treatment on mandibular second molars. After applying subject criteria and excluding those lost during follow-up, a total of 195 patients consisting of 59.9% male (115/195) and 41.1% female (80/195) were included. The recall rate was 69.9%. The distribution of tooth locations was 51.0% for the left mandibular second molar and 49.0% for the right. The mean age was 46.0 (± 14.9) years, ranging from 12 to 81. The mean follow-up duration was 24.4 (± 17.3) months. The longest duration of recall was 80 months and the shortest duration was 6 months. Total 196 teeth from 195 patients were included in this study.
Among the 196 teeth, the total healing rate was 68.4%, which includes 103 completely healed teeth (52.6%) and 31 incompletely healed teeth (15.8%). Among C-shaped root canals (n = 79), 44 teeth (55.7%) had completely healed and 12 teeth (15.2%) had incompletely healed, which means the healing rate was 70.9%. In the case of non-C-shaped root canals (n = 117), 59 teeth (50.4%) underwent complete healing and 19 teeth (16.2%) incompletely healed, demonstrating a healing rate of 66.6%. The difference in healing rates between the two groups was not statistically significantly.
A chi-square analysis was conducted in order to reveal the factors that affect healing outcome. The results of the chisquare test of C-shaped root canals (n = 79) are shown in Table 3. This indicates that in teeth with C-shaped root canals, only the presence of final full crown restoration had a significant correlation with healing outcome (p < 0.05). To see the direction of correlation, a multinomial logistic regression analysis was also done. The results are summarized in Table 4. Absence of full crown restoration had a positive correlation with the cases rated for incomplete or unsatisfactory healing.
The cases of non-C-shaped root canals were also analyzed for comparison with C-shaped root canals. The results are shown in Table 5. As mentioned above, a multinomial logistic regression analysis was also applied to see the direction of correlation. The results are summarized in Table 6. Age had a significant correlation with incomplete healing and normal pulp had a correlation with uncertain healing.
The follow-up period was calculated from the day of canal filling to last follow-up. With the follow-up period set as an independent variable and healing outcome as a dependent variable, regression analysis results showed that the follow-up period significantly affected healing outcome (p < 0.05). The mean follow-up period was 24.4 months.
The PAI scoring system, which was suggested by Orstarvik et al.,15 has been accepted as a useful tool for revealing changes caused by periapical inflammation and for evaluating root canal treatment outcomes.16 This system was developed for use in clinical trials and epidemiological surveys.17 Although scoring with the use of periapical radiographs was first suggested, panoramic views have also been used for scoring in many studies and so are considered to be valid tools for periapical lesion detection.13 As such, both of them were used in this study.
The main anatomic feature of the C-shaped root canal is the fin or the web that connects individual root canals.5 The apical third is generally regarded as an important section where complete debridement is critical for a good prognosis for root canal treatment; hence, a C-shaped root canal undoubtedly poses a challenge to clinicians.5 However, the results of this study show that there were no significant correlations between the healing outcomes of non-surgical root canal treatment of C-shaped and non-C-shaped root canals. Therefore, the presence of C-shaped root canal morphology did not significantly affect healing outcome.
As shown in the results of the multinomial logistic analysis of C-shaped root canal cases (n = 79), unsatisfactory healing significantly increased without final full crown restoration. This agrees with the studies of Ray and Trope,17 Pirani et al.,18 and Katebzadeh et al.,19 which demonstrated that the coronal seal above the canal filling material is critical in preventing coronal leakage and root canal re-infection. In the study by Ray and Trope,17 teeth with poor restoration had a significantly higher presence of periradicular inflammation when compared to teeth with good restoration.17 Considering the structural complexity of the C-shaped root canal and the retention of debris and a smear layer along the apical third of canal walls, an isthmus and fins are commonly seen in C-shaped root canals. It is also difficult to remove diseased or necrotic pulp tissue from these parts of the root completely.6 This results in an absence of sealing material in these areas, which might contribute to a higher degree of microleakage. Although apical leakage from the complexity of the C-shaped canal has not been adequately proven, the above-mentioned results can be assumed to be consequences of the combination of coronal leakage because of the absence of full crown restoration and partial apical leakage from the complex canal structure.
In the case of a non-C-shaped root canal, treatment outcomes were significantly related to the preoperative status of the pulp. This is in accordance with a Tennessee study that evaluated factors affecting healing outcome and the time following non-surgical root canal treatment. The outcome was significantly affected by the preoperative pulp condition, with a more favorable outcome in vital pulps than non-vital ones.20 Another study by Sjogren et al.21 showed similar results.
The multinomial logistic regression was used to assess whether independent variables (age, gender, location, pulp, periapex, full crown, and crack or fracture) were related to the potential outcomes of periapical healing after endodontic treatment in terms of the four categories of the PAI scoring system. In the case of follow-up period, solely to determine if this factor affects healing outcomes, a regression analysis was chosen. In the regression analysis, the R2 value refers to the Nagelkerke R2 for the explanation of goodness-of-fit. Regarding the impact of follow-up periods in this study, the results showed that the duration of follow-up had a significant relationship with healing outcomes, in a negative direction. This means that a longer follow-up period resulted in a less successful treatment outcome. However, as the R2 value was 0.03, this relationship is not important. This consequence seemingly resulted from the fact that other variables were not taken into consideration in this analysis.
For the evaluation of healing, according to the change value of the PAI score, four categories including 'completely healed', 'incompletely healed', 'uncertain healing', and 'no healing' were applied. Typically based on histological correlation, PAI scores of 1 and 2 are regarded as healed or minimally inflamed and scores of 3 - 5 are defined as diseased.22 Therefore, in cases with the same scores, a change could imply a different healing outcome. For example, cases with PAI scores changing from 4 to 2 were included in the 'incompletely healed' category and cases with PAI scores changing from 5 to 3 were included in the 'uncertain healing' category. A study by Azim et al. divided the 'not healing' cases into two categories: 'uncertain healing', which shows no change in the size of the lesion or clinical signs and symptoms and 'unsatisfactory healing', which indicates the presence of a new lesion, an increase in size, or clinical signs and symptoms.20 Considering this, it can be said that the utilization of the change value of the PAI score system in this study is meaningful because a more detailed division of healing outcome, including uncertain healing, was possible.
As a retrospective study, the main limitation of this study is the non-standardization of intra-operative factors in detailed clinical procedures. Important features such as properly controlled procedures and significant parameters for the outcome should be appropriately monitored in order to provide good evidence. It is suggested that in future studies the healing rate of root canal treatment of C-shaped root canals be clinically studied prospectively.23
Given that the reported average survival rate of non-surgical endodontic treatment in the literature is between 85 and 95%,24252627 the healing rate of this study is quite low. This is because, usually, the criteria for the healing rate apply a stricter standard than for the survival or retention rate of endodontic treatment. Another study concerning the diagnosis of cracked teeth in Koreans agreed that patients are referred to endodontists only following a long period since the initial manifestation of the symptoms; hence, they were referred for late diagnosis, which required advanced treatment.28 Since most studies that evaluate healing outcome after root canal treatment recommend a 1 year follow-up period on average,293031 a mean follow-up period of 24.4 months might also be the reason for the relatively lower healing rate considering that more time gives more opportunity for healing.
This study evaluated the non-surgical root canal treatment outcomes of 196 mandibular second molars based on radiographic images and the clinical records of 195 Koreans with a comparison between C-shaped and non-C-shaped root canals. The results showed a healing rate of 70.9% in C-shaped root canals (n = 79), and 66.6% in non-C-shaped ones (n = 117). This study revealed that the presence of a C-shaped root canal in the mandibular second molar did not have a significantly negative effect on the root canal treatment outcome. Out of all the evaluated factors, the presence of final restoration significantly affected the healing outcomes of C-shaped root canals and the preoperative pulp status significantly affected that of non-C-shaped ones.
Figures and Tables
Table 1
The classification of healing outcome

Table 2
The demographic data of the study
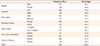
Table 3
The results of a chi-square analysis of C-shaped root canals (n = 79)

Table 4
The results of a multinomial logistic regression analysis showing the detailed direction of correlation of C-shaped root canals (n = 79)

Table 5
The results of a chi-square analysis of non-C-shaped root canals (n = 117)

Table 6
The results of a multinomial logistic regression analysis showing the detailed direction of correlation of non-C-shaped root canals (n = 117)

References
1. Fan B, Cheung GS, Fan M, Gutmann JL, Bian Z. C-shaped canal system in mandibular second molars: part I-anatomical features. J Endod. 2004; 30:899–903.

2. Min Y, Fan B, Cheung GS, Gutmann JL, Fan M. C-shaped canal system in mandibular second molars: part III-the morphology of the pulp chamber floor. J Endod. 2006; 32:1155–1159.

3. Gao Y, Fan B, Cheung GS, Gutmann JL, Fan M. C-shaped canal system in mandibular second molars: part IV-morphological analysis and transverse measurement. J Endod. 2006; 32:1062–1065.

4. Cooke HG 3rd, Cox FL. C-shaped canal configurations in mandibular molars. J Am Dent Assoc. 1979; 99:836–839.

5. Cheung GS, Yang J, Fan B. Morphometric study of the apical anatomy of C-shaped root canal systems in mandibular second molars. Int Endod J. 2007; 40:239–246.

6. Kato A, Ziegler A, Higuchi N, Nakata K, Nakamura H, Ohno N. Aetiology, incidence and morphology of the C-shaped root canal system and its impact on clinical endodontics. Int Endod J. 2014; 47:1012–1033.

7. Seo MS, Park DS. C-shaped root canals of mandibular second molars in a Korean population: clinical observation and in vitro analysis. Int Endod J. 2004; 37:139–144.

8. Cheung LH, Cheung GS. Evaluation of a rotary instrumentation method for C-shaped canals with micro-computed tomography. J Endod. 2008; 34:1233–1238.

9. Yin X, Cheung GS, Zhang C, Masuda YM, Kimura Y, Matsumoto K. Micro-computed tomographic comparison of nickel-titanium rotary versus traditional instruments in C-shaped root canal system. J Endod. 2010; 36:708–712.

10. Lea CS, Apicella MJ, Mines P, Yancich PP, Parker MH. Comparison of the obturation density of cold lateral compaction versus warm vertical compaction using the continuous wave of condensation technique. J Endod. 2005; 31:37–39.

11. Fan B, Cheung GS, Fan M, Gutmann JL, Fan W. C-shaped canal system in mandibular second molars: part II-radiographic features. J Endod. 2004; 30:904–908.

12. Doyle SL, Hodges JS, Pesun IJ, Law AS, Bowles WR. Retrospective cross sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants. J Endod. 2006; 32:822–827.

13. Tolias D, Koletsi K, Mamai-Homata E, Margaritis V, Kontakiotis E. Apical periodontitis in association with the quality of root fillings and coronal restorations: a 14-year investigation in young Greek adults. Oral Health Prev Dent. 2012; 10:297–303.
14. Dammaschke T, Steven D, Kaup M, Ott KH. Long-term survival of root-canal-treated teeth: a retrospective study over 10 years. J Endod. 2003; 29:638–643.

15. Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986; 2:20–34.

16. Wu MK, Shemesh H, Wesselink PR. Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment. Int Endod J. 2009; 42:656–666.

17. Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995; 28:12–18.

18. Pirani C, Chersoni S, Montebugnoli L, Prati C. Long-term outcome of non-surgical root canal treatment: a retrospective analysis. Odontology. 2015; 103:185–193.

19. Katebzadeh N, Sigurdsson A, Trope M. Radiographic evaluation of periapical healing after obturation of infected root canals: an in vivo study. Int Endod J. 2000; 33:60–66.

20. Azim AA, Griggs JA, Huang GT. The Tennessee study: factors affecting treatment outcome and healing time following nonsurgical root canal treatment. Int Endod J. 2016; 49:6–16.

21. Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997; 30:297–306.

22. Trope M, Delano EO, Orstavik D. Endodontic treatment of teeth with apical periodontitis: single vs. multivisit treatment. J Endod. 1999; 25:345–350.

24. Basmadjian-Charles CL, Farge P, Bourgeois DM, Lebrun T. Factors influencing the long-term results of endodontic treatment: a review of the literature. Int Dent J. 2002; 52:81–86.

25. Chugal NM, Clive JM, Spångberg LS. Endodontic infection: some biologic and treatment factors associated with outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 96:81–90.

26. Chugal NM, Clive JM, Spångberg LS. A prognostic model for assessment of the outcome of endodontic treatment: effect of biologic and diagnostic variables. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:342–352.

28. Kim SY, Kim SH, Cho SB, Lee GO, Yang SE. Different treatment protocols for different pulpal and periapical diagnoses of 72 cracked teeth. J Endod. 2013; 39:449–452.

29. Siqueira JF Jr, Rôças IN, Riche FN, Provenzano JC. Clinical outcome of the endodontic treatment of teeth with apical periodontitis using an antimicrobial protocol. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:757–762.

30. Reit C. Decision strategies in endodontics: on the design of recall program. Endod Dent Traumatol. 1987; 3:233–239.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download