Abstract
Objectives
This study aimed to analyze the mineral composition of naturally- and artificially-produced caries-affected root dentin and to determine the elemental incorporation of resin-modified glass ionomer (RMGI) into the demineralized dentin.
Materials and Methods
Box-formed cavities were prepared on buccal and lingual root surfaces of sound human premolars (n = 15). One cavity was exposed to a microbial caries model using a strain of Streptococcus mutans. The other cavity was subjected to a chemical model under pH cycling. Premolars and molars with root surface caries were used as a natural caries model (n = 15). Outer caries lesion was removed using a carbide bur and a hand excavator under a dyeing technique and restored with RMGI (FujiII LC, GC Corp.). The weight percentages of calcium (Ca), phosphate (P), and strontium (Sr) and the widths of demineralized dentin were determined by electron probe microanalysis and compared among the groups using ANOVA and Tukey test (p < 0.05).
Results
There was a pattern of demineralization in all models, as visualized with scanning electron microscopy. Artificial models induced greater losses of Ca and P and larger widths of demineralized dentin than did a natural caries model (p < 0.05). Sr was diffused into the demineralized dentin layer from RMGI.
Conclusions
Both microbial and chemical caries models produced similar patterns of mineral composition on the caries-affected dentin. However, the artificial lesions had a relatively larger extent of demineralization than did the natural lesions. RMGI was incorporated into the superficial layer of the caries-affected dentin.
The incidence of root surface caries is increasing as the population ages, and the elderly maintain natural dentition. The surface of roots may become exposed due to periodontal diseases and by mechanical instrumentation during scaling and root planing. Root dentin is vulnerable to acidic dissolution than enamel because of its higher critical pH for demineralization (6.2 - 6.4) than that of enamel (5.5).1 Developing root surface caries is often manifested as lesion enveloping the broad surface of the entire root.2 It is difficult to define the proper retentive form of the cavity and the cavity margins are based on a tooth structure often devoid of sound enamel. In addition, unlike sound dentin, caries-affected dentin undergoes histopathological changes that results in decreased bonding efficiency.3 In order to overcome the clinical dilemmas in performing bonded restoration to caries-affected root dentin, numerous variables must be testified under various experimental setups. Therefore, it would be beneficial to have artificially mineral-depleted lesions produced in a standardized manner, resembling naturally-progressed root caries lesions.
In caries research, the mineral content within a tooth structure reflects the extent of demineralization and remineralization processes. Recently, electron probe microanalysis (EPMA) has been used to measure the concentration and distribution of elements in a lesion. While conventional transverse microradiography measures the sum of total mineral deposits over the thickness of the section, EPMA can identify individual elements and provide information about trace elements incorporated from external sources.4 In a study by Ngo et al., EPMA validated an elemental migration from glass ionomer cement (GIC) into calcium-depleted dentin spaces.5 Previous studies using EPMA have mostly focused on occlusal caries to evaluate the remineralizing potential of inner caries-affected dentin after outer infected dentin is removed. In cases of root surface caries, minimally-invasive caries excavation is more important, when the cavity floor and pulpal space are close in proximity, to avoid the cost and risk of endodontic treatment. When bonded restoration is placed over partially demineralized caries-affected dentin, the altered characteristics of the bonded interface may affect the long-term stability of the root surface restoration.6
In this study, artificially demineralized root dentin was produced using microbial and chemical models in order to compare them to natural caries lesions. After the carious dentin was excavated using a dyeing technique, the cavities were restored with resin-modified glass ionomer (RMGI). EPMA measured calcium (Ca), phosphate (P), and strontium (Sr) in weight percentages across the bonded interface. Scanning electron microscopy (SEM) exhibited the topographical features of caries-affected dentin. The aims of the study were to compare the mineral compositions of demineralized root dentin produced by microbial and chemical models to those of naturally occurring caries, and to verify Sr incorporation into the demineralized dentinal structure from RMGI.
All procedures performed in this study involving human participants (human teeth collected after extraction) were in accordance with the ethical standards of the institutional committee. This study was approved by the Institutional Review Board at Seoul National University Dental Hospital (CRI13010). Fifteen sound human premolars extracted during dental treatment were selected as a source of root dentin for the artificial models. A total of 15 extracted premolars and molars with root surface caries extending to 1/3 to 2/3 the depth of dentin were selected for the natural model. All teeth were disinfected in a 0.5% chloramine-T solution for one week and were then stored in distilled water at 4℃. For the artificial models, box-formed cavities were prepared on the buccal and lingual root surfaces. The upper margin of the cavity was 1.5 mm from the dentinoenamel junction. The cavity was 2 mm wide mesiodistally, 5 mm long vertically, and 2 mm deep pulpally. All specimens were vertically sectioned in half mesiodistally. Either the buccal or lingual cavity was randomly allocated to one of two different caries models. The specimens were covered completely with an acid-resistant nail varnish except for the inner walls of the cavity, which would be exposed to a caries-inducing environment.
In order to produce microbially induced caries, Streptococcus mutans (S. mutans, ATCC 25175) was obtained from a frozen stock. Cultures were grown in sterile Trypticase Soy Broth (TSB, Difco Laboratories, Detroit, MI, USA) with 5% sucrose (Amresco, Solon, OH, USA) for 48 hours. Aliquots of 1 mL were then transferred to each 15 mL conical tube containing one root specimen and 10 mL of TSB. Fifteen specimens, each with a half section of a tooth, were incubated in 10% CO2 at 37℃ for 2 weeks. The broth was freshly replaced every 48 hours. In order to avoid contamination, all microbiological manipulations were done under aseptic conditions in a flow chamber.
In order to produce chemically induced caries, 15 specimens from the other sections of the teeth were immersed in 2.5 mL of demineralizing solution (1.5 mM CaCl2, 0.9 mM KH2PO4, 50 mM acetate buffer, pH 4.8)7 for 24 hours. Next, they were immersed in 2.5 mL of remineralizing solution (1.5 mM CaCl2, 0.9 mM KH2PO4, 20 mM HEPES [4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid], pH 7.0) for 24 hours. The specimens were rinsed with deionized water for 20 seconds during every solution change. The cycling was performed at 37℃ for 2 weeks.
The cavities in artificial caries specimens were stained with Sable Seek Caries indicator (Ultradent, South Jordan, UT, USA). Softened dentin was excavated using a low-speed carbide bur and a spoon excavator until no traces of dye remained. When the root caries lesion was undermining enamel tissue, the overlying enamel of natural root caries was removed using a tungsten carbide bur (No. 330) in a high-speed handpiece until the carious dentin was exposed. The carious dentin was then excavated in the same manner as that used for the artificial caries specimens. All the cavities were conditioned using Dentin Conditioner (GC Corp., Tokyo, Japan) for 10 seconds, washed with water spray for 15 seconds, dried with dry compressed air for 15 seconds, and filled with RMGI (Fuji II LC capsule, GC Corp.) according to the manufacturer's instructions. The restoration was cured for 20 seconds using a light-emitting diode curing light (Elipar FreeLight 2, 3M ESPE, St. Paul, MN, USA) with an intensity of 1,200 mW/cm2. The restored teeth were stored in distilled water in a sealed container at 37℃.
Specimens were embedded in epoxy resin (Epofix, Struers, Glasgow, UK) and horizontally cross-sectioned along the midline of the cavity. The exposed cut surfaces were serially polished with 1,200, 2,400, and 4,000 grit aluminum oxide abrasive papers, followed by 1 µm diamond polishing suspensions (Struers, Copenhagen, Denmark). The specimens were ultrasonically cleaned in deionized water for 10 minutes, dried for 72 hours in a desiccator, and then sputter-coated with carbon. The demineralization areas on the cross-sectioned dentinal surfaces were identified using the phase contrast of the backscattered electron imaging (BSI) mode of SEM (JEOL JSM-6610LV, JEOL, Akishima, Japan). Two-line analyses were performed perpendicular to both lateral walls of the cavity at 0.5 µm pixel intervals (Figure 1). The weight percentages of Ca, P, and Sr were measured using an electron microprobe (JEOL JXA-8100, JEOL). The operating conditions for the elemental analyses included 15 kV of accelerating voltage and 30 nA of beam current. A fluorapatite crystal (3.38% F) was used as a standard comparison to analyze Ca and P. Strontium Carbonate (SrCO3) was used as a standard comparison for Sr.
The Kolmogorov-Smirnov test was used to test the samples' normality and homogeneity. The weight percentages of Ca, P, and Sr were compared among the groups using ANOVA and Tukey post hoc test in the areas of RMGI, caries-affected dentin, and sound dentin. The Ca and P contents in the sound dentin were set to 100%. The percentages of Ca and P lost in the demineralized area were calculated (Figure 2). The width (µm) of the demineralized area in the caries-affected dentin was measured where the Ca content ranged between 10 and 95% of that of sound dentin.5 The mean width of the caries-affected dentin and loss of Ca and P contents were compared among all groups using ANOVA and Tukey post hoc test. A p value of 0.05 was selected as the threshold for statistical significance. Analyses were performed using SPSS version 12.0 statistical software (SPSS Inc., Chicago, IL, USA).
The mean weight percentages of Ca, P, and Sr in three observational areas (RMGI, caries-affected dentin, and sound dentin) were shown in Table 1. In the RMGI and sound dentin, the contents of three elements are not different among the groups. In the caries-affected dentin, Ca, P, and Sr contents were higher in the natural model than in the chemical and microbial models (p < 0.05). In the same area, Ca and Sr were higher in the chemical model than in the microbial model (p < 0.05). The mean width of lesion was smallest in the natural model, followed by the chemical and microbial model (p < 0.05, Table 2). The mean loss of Ca in the natural model (26.73 ± 6.27%) was lower than in the chemical model (50.76 ± 4.11%) and in the microbial model (56.01 ± 3.78%, p < 0.05). The mean loss of P was in the natural model (26.25 ± 8.73%) was lower than in the chemical model (51.53 ± 4.55%) and in the microbial model (56.46 ± 3.63%, p < 0.05). The mean ratios of Ca/P in the caries-affected and sound dentin were not significantly different among the groups.
SEM showed a similar pattern of demineralization in caries-affected dentin among all samples such as mineral-depleted tubular spaces and loosely packed intertubular dentinal structures (Figure 3). EPMA demonstrated the elemental compositions of Ca, P, and Sr in the sound dentin, caries-affected dentin, and RMGI areas (Figure 4). Ca and P contents gradually recovered reaching to the sound dentin area with varying gradients in the three groups. There was an increase in the Sr content where the caries-affected dentin began, indicating a high accumulation of the element on the surface.
Proper management of root surface caries requires careful excavation of the infected tissue and application of adhesive materials on the remaining dentinal surfaces. Our primary goal was to create artificially demineralized root dentin and to compare it to natural lesions with regard to microscopic features and mineral composition. Natural caries process is a dynamic phenomenon which is repeated stagnation and progression of acid dissolution for a prolonged period of time.8 No laboratory method is able to replicate natural caries lesions per se. However, partially demineralized dentinal tissue obtained after excavation of a superficially softened layer is close to natural caries-affected dentin, which has a minimally affected collagen matrix and is still capable of mineral aggregation.9 The mineral contents of our artificial caries-affected dentin were around 50% of those of sound dentin, which was in accordance with the outcomes of other studies.1011 We used microbial and chemical methods to simulate the acid-mediated demineralization process that occurs naturally. The microbial method is more physiologic than is the chemical method; however, organic acid production by cariogenic bacteria takes more time to demineralize the dental tissue than does the chemical method, and tends to accelerate at a certain point.11 In this study, S. mutans, the most representative cariogenic pathogen in the oral microbiota, was used in the biological model, which was a far simplified mono-culture setting. Shen et al. demonstrated that the demineralization ability and cariogenicity of S. mutans were able to induce demineralization of dental tissue at a comparable level as multi-species models comprised of S. mutans, Lactobacillus acidophilus, and Actinomyces israelii.12 Our study also observed the formation of a small demineralized zone in a mono-culture model. The chemical method using an acidic solution involves a simpler technique that makes it relatively easy to control the experimental condition. Regardless, both systems produce a varying degree of demineralization over time with a change of duration and severity in acidic challenge. A demineralized layer can be gradually produced with a largely mineral-depleted outer lesion and less demineralized inner lesion.
This study investigated the interfacial features of caries-affected dentin restored with RMGI after excavation of outer soft lesion. The biological method of artificial caries produced a greater width of demineralized dentin and a marginally higher loss of Ca than did the chemical method, likely due to accelerated acid production in the biological model. Both artificial lesions produced similar microscopic features including mineral-depleted tubular structures. There was also gradual recovery of Ca and P levels across both types of artificial lesions. The natural caries lesions varied in the extents of demineralization depending on the activity and duration of the previous caries process. This variation is reflected by a large standard deviation in the mineral contents. In general, there was a smaller extent of caries-affected dentin beyond sound dentin in the natural caries lesions than there was in the artificial lesions. There may be a physiological defense mechanisms that counteracts the acidic dissolution of hydroxyapatite in an in vivo condition, which would have been absent in the artificial models. In the artificial caries model, we used sound premolars mostly extracted for orthodontic treatment of relatively young patients in order to obtain standardized substrates as possible, in terms of anatomical and histochemical features. Also, the box-formed cavities prepared in the buccal and lingual surfaces of premolars were different from actual cavities for root surface restoration with an extension from a decalcified area. Conversely, natural caries lesions were largely obtained from premolars and molars extracted due to advanced periodontal disease or caries. This could also have contributed to the disparities in demineralization between natural and artificial lesions. However, there were no significant differences between the models with regard to the Ca/P ratio, suggesting that mineral proportions were maintained under various acid-challenged processes.
Our secondary aim was to characterize the elemental migration from RMGI into the partially demineralized caries-affected dentin. Conventional GIC or RMGI is useful in caries management because it exhibits chemical adherence and fluoride release.2 RMGI is the material of choice in root surface restoration because light-cured resin polymerization can be used, which allows for immediate setting, improved strength, and esthetic enhancement.1314 RMGI has bonding capacity that enhances its ionic bonding to hydroxyapatite and it exhibits micromechanical interlocking similar to that of conventional GIC.15 Previous studies have mostly investigated conventional GIC and determined the contents of F or Sr, which is representative of GIC and an apatite-forming element.51617 Ngo et al. presented an in vitro model of the atraumatic restorative technique by applying GIC on demineralized dentin without removing the outer soft layer.5 Using EPMA with a relatively broader resolution (5 µm), they demonstrated that Sr migrated across a broadly-demineralized dentinal zone. With RMGI we found that the elevated Sr level in the caries-affected dentin gradually decreased toward the sound dentin; this gradient was reversed with regard to the Ca and P contents. The natural caries lesions had shallower demineralized layers than did the artificial lesions. However, there was still Sr incorporation into the mineral-depleted apatite lattice of the natural lesions. This process may be driven via diffusion, because the Sr level was highest at the surface and disappeared deep into the sound dentin. This ionic exchange occurred at a very superficial level where a thin hybrid layer allows chemical and micromechanical adhesion. The peak Sr level in the surface of the demineralized layer indicated regional accumulation in the superficial dentin. This phenomenon was observed in both artificial and natural caries lesions.
In our study, the outer layer of carious dentin was stained with caries detector dye to reduce subjective judgment and to do standardized caries removal. This dyeing technique has been challenged by concerns of overexcavation of caries-affected, mineralizable dentin. However, many studies using dyeing techniques did not precisely simulate clinical conditions: the dyes were applied to cross-sectioned dentinal surface not to the surface of pulpal floor or were applied at the end of bur excavation of dentin, not on gross carious dentin immediately after gaining access to caries.18 According to Boston and Liao, all five commercial dyes evaluated in their study, including Sable Seek Caries Indicator, stained non-carious dentin to some extent; however, this stain could be differentiated from the staining of outer infectious dentin.19
There was a difference between artificial and natural root caries lesions with regard to the extent of demineralization of the caries-affected dentin. Future studies are needed to produce various degrees of demineralization with altered experimental conditions. It will also be beneficial to simulate slowly- and rapidly-progressing caries processes. Artificial lesions at various stages of caries progression may be useful to examine the interfacial hybridization between adhesive materials and caries-affected dentin.
Based on this in vitro study, two types of artificially demineralized root dentin by microbial and chemical methods exhibited similar patterns of mineral depletion along the depth of the lesion. The artificial samples produced an extended demineralization zone as compared to that of natural caries lesions. In both artificial and natural caries lesions, Sr was incorporated into the demineralized dentin from RMGI.
Figures and Tables
Figure 1
Images of the cross-sectioned surfaces of the specimens from the microbial model (a) and the chemical model (b). EPMA analysis was performed perpendicular to the interface between the caries-affected dentinal wall and RMGI restoration (arrows). EPMA, electron probe microanalysis; RMGI, resin-modified glass ionomer.

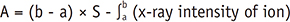
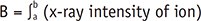
Figure 2
Schematic diagram of the calculation of mineral loss (A) in percentage in the lesion area. The Ca and P contents in the sound dentin (S) were set to 100%. The percentages of Ca and P lost in the demineralized area were calculated. The width (µm) of the demineralized area in the caries-affected dentin was measured where the Ca content ranged between 10% (a) and 95% (b) of that of sound dentin. S is an average mineral content of sound dentin. cps, counts per second.

Figure 3
SEM images (×300) of the cross-sectioned specimens with artificial caries produced from the (a) microbial, (b) chemical, and (c) natural caries models. All three specimens demonstrate features of caries-affected dentin. A dark band of demineralization zone (dark arrows) is comprised of mineral-depleted intratubular dentin and widened intertubular spaces. The white lines (light arrows) perpendicular to the interface between RMGI and dentin are EPMA scan lines. SEM, scanning electron microscopy; RMGI, resin-modified glass ionomer; EPMA, electron probe microanalysis.

Figure 4
The mean weight percentages of Ca, P, and Sr were measured at intervals of 0.5 µm starting from the surface of the caries-affected dentin to the deep sound dentin in the microbial, chemical, and natural caries models. (a and b) The Ca and P contents quickly recovered within 20 - 30 µm of the natural caries lesion. Loss of Ca and P gradually recovered at a depth of 80 µm in the chemical caries lesion, while the loss extended to a depth of 140 µm in the microbial caries lesion; (c) The Sr content arose at the surface of the caries-affected dentin within 20 µm, more narrowly in the natural caries lesion. Ca, calcium; P, phosphate; Sr, strontium.

Table 1
The elemental contents (x-ray intensity, cps) of Ca, P, and Sr in the RMGI, caries-affected dentin, and sound dentin in the microbial, chemical, and natural caries models

Table 2
The lesion width, the mineral loss of Ca and P, and the Ca/P ratio in the caries-affected dentin of the microbial, chemical and natural caries models

Acknowledgement
This study was supported by grant No. 04-2013-0072 from the Seoul National University Dental Hospital Research Fund.
References
1. Heijnsbroek M, Paraskevas S, Van der Weijden GA. Fluoride interventions for root caries: a review. Oral Health Prev Dent. 2007; 5:145–152.
2. Amer RS, Kolker JL. Restoration of root surface caries in vulnerable elderly patients: a review of the literature. Spec Care Dentist. 2013; 33:141–149.

3. Perdigão J. Dentin bonding-variables related to the clinical situation and the substrate treatment. Dent Mater. 2010; 26:e24–e37.

4. Ngo H, Ruben J, Arends J, White D, Mount GJ, Peters MC, Faller RV, Pfarrer A. Electron probe microanalysis and transverse microradiography studies of artificial lesions in enamel and dentin: a comparative study. Adv Dent Res. 1997; 11:426–432.

5. Ngo HC, Mount G, McIntyre J, Do L. An in vitro model for the study of chemical exchange between glass ionomer restorations and partially demineralized dentin using a minimally invasive restorative technique. J Dent. 2011; 39:Supplement 2. S20–S26.
6. Hevinga MA, Opdam NJ, Frencken JE, Truin GJ, Huysmans MC. Does incomplete caries removal reduce strength of restored teeth? J Dent Res. 2010; 89:1270–1275.

7. ten Cate JM, Buijs MJ, Miller CC, Exterkate RA. Elevated fluoride products enhance remineralization of advanced enamel lesions. J Dent Res. 2008; 87:943–947.

8. Kidd EA, Fejerskov O. What constitutes dental caries? Histopathology of carious enamel and dentin related to the action of cariogenic biofilms. J Dent Res. 2004; 83(Spec No C):C35–C38.

9. Schwendicke F, Meyer-Lueckel H, Schulz M, Dörfer CE, Paris S. Radiopaque tagging masks caries lesions following incomplete excavation in vitro. J Dent Res. 2014; 93:565–570.

10. Pugach MK, Strother J, Darling CL, Fried D, Gansky SA, Marshall SJ, Marshall GW. Dentin caries zones: mineral, structure, and properties. J Dent Res. 2009; 88:71–76.

11. Joves GJ, Inoue G, Nakashima S, Sadr A, Nikaido T, Tagami J. Mineral density, morphology and bond strength of natural versus artificial caries-affected dentin. Dent Mater J. 2013; 32:138–143.

12. Shen S, Samaranayake LP, Yip HK. In vitro growth, acidogenicity and cariogenicity of predominant human root caries flora. J Dent. 2004; 32:667–678.

13. McComb D, Erickson RL, Maxymiw WG, Wood RE. A clinical comparison of glass ionomer, resin-modified glass ionomer and resin composite restorations in the treatment of cervical caries in xerostomic head and neck radiation patients. Oper Dent. 2002; 27:430–437.
14. De Moor RJ, Stassen IG, van't Veldt Y, Torbeyns D, Hommez GM. Two-year clinical performance of glass ionomer and resin composite restorations in xerostomic head- and neck-irradiated cancer patients. Clin Oral Investig. 2011; 15:31–38.

15. Coutinho E, Yoshida Y, Inoue S, Fukuda R, Snauwaert J, Nakayama Y, De Munck J, Lambrechts P, Suzuki K, Van Meerbeek B. Gel phase formation at resin-modified glass-ionomer/tooth interfaces. J Dent Res. 2007; 86:656–661.

16. AL-Helal AS, Armstrong SR, Xie XJ, Wefel JS. Effect of smear layer on root demineralization adjacent to resin-modified glass ionomer. J Dent Res. 2003; 82:146–150.

17. Ab-Ghani Z, Ngo H, McIntyre J. Effect of remineralization /demineralization cycles on mineral profiles of Fuji IX Fast in vitro using electron probe microanalysis. Aust Dent J. 2007; 52:276–281.

18. Borczyk D, Piatowska D, Krzemiński Z. An in vitro study of affected dentin as a risk factor for the development of secondary caries. Caries Res. 2006; 40:47–51.

19. Boston DW, Liao J. Staining of non-carious human coronal dentin by caries dyes. Oper Dent. 2004; 29:280–286.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download