Abstract
The reconstruction of structurally compromised posterior teeth is a rather challenging procedure. The tendency of endodontically treated teeth (ETT) to fracture is considerably higher than vital teeth. Although posts and core build-ups followed by conventional crowns have been generally employed for the purpose of reconstruction, this procedure entails sacrificing a considerable amount of residual sound enamel and dentin. This has drawn the attention of researchers to fibre reinforcement. Fibre-reinforced composite (FRC), designed to replace dentin, enables the biomimetic restoration of teeth. Besides improving the strength of the restoration, the incorporation of glass fibres into composite resins leads to favorable fracture patterns because the fibre layer acts as a stress breaker and stops crack propagation. The following case report presents a technique for reinforcing a badly broken-down ETT with biomimetic materials and FRC. The proper utilization of FRC in structurally compromised teeth can be considered to be an economical and practical measure that may obviate the use of extensive prosthetic treatment.
The rehabilitation of a heavily damaged endodontically treated molar poses a challenge to clinicians. The successful restoration of endodontically treated teeth (ETT) requires an effective coronal seal, protection of the remaining tooth, restored function, and acceptable aesthetics. The use of custom-made or prefabricated posts has gained popularity and is now frequently employed for the reconstruction of ETT. However, one mode of failure of post-restored teeth is root fracture, which underscores the need for a minimally invasive procedure.1
The biomechanics of an ETT are primarily altered by tissue loss due to prior pathologies (caries and trauma), endodontic treatment (access cavity, cleaning, and shaping), and invasive restorative procedures (post placement and crown fabrication). All of these factors collectively result in a consistent elimination of coronal and radicular tissue, thereby increasing the fragility of an ETT and thus the risk that it may be fractured.2
Therefore, the intracoronal strengthening of teeth to protect them against fracture is important, particularly in posterior teeth where the stresses generated by forces of occlusion can lead to the fracture of unprotected cusps.3 More importantly, the amount of remaining tooth structure following endodontic therapy is an important factor in the evaluation of a tooth's prognosis regarding restorative and/or prosthetic procedures.4
With the growing advances in adhesive techniques over the past few decades, conservative restoration of ETT is now a practical alternative. Bonded coronal restorations are preferred over the more radical full-crown preparations to prevent further loss of healthy tissues, as adhesion ensures sufficient material retention and eliminates the need for aggressive macroretentive features, thereby providing a more economical and time-saving option.2
The incorporation of reinforcing short fibres into composite resins has solved many problems related to the restoration of badly broken-down teeth. Fibre-reinforced composites (FRCs) are intended to be used in high stress-bearing areas, especially in molars. In vitro studies have revealed substantial improvements in the load-bearing capacity, flexural strength, fracture toughness, and control of the polymerization shrinkage stress by fibre orientation, which contribute to reduced microleakage of composites reinforced with short E-glass fibres in comparison with conventional particulate filler restorative composite resin.56 The following case report describes a conservative technique for the restoration of a badly broken-down endodontically treated molar.
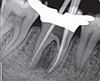
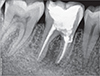
A 25 year old female patient presented to the Department of Conservative Dentistry and Endodontics with a chief complaint of pain in the region of the mandibular right first molar. She reported that an emergency access opening was performed one week prior for the same. Upon clinical examination, extensive destruction of the coronal tooth structure was noted (Figure 1). Radiographic analysis revealed a periapical radiolucent lesion around the mesial and distal root of tooth #46, and the periradicular dentin at the coronal third of the mesial root was compromised as a result of the poor endodontic access cavity (Figure 2).
Based on the clinical and radiographic findings, a treatment plan was made. Endodontic therapy was initiated (Figure 3). Following the cleaning and shaping of the canals, calcium hydroxide (Avue Cal, Dental Avenue, Param Enterprises, Pune, India) was placed as an intracanal medicament for one and half months. The dressing was changed every two weeks. Once the tooth demonstrated signs of radiographic healing of the periapical lesion and the absence of symptoms, the obturation was completed with cold lateral condensation and resin-based sealer (AH Plus, Dentsply DeTrey, Konstanz, Germany, Figures 4 and 5) and the tooth was temporised. Since the remaining amount of dentin around the mesial orifice and on the floor of the chamber was compromised and nearly approached the furcation, we decided to place Biodentine (Septodont, Saint-Maur-des-Fossés, France) as a dentin substitute base. The following day, a 2 mm thick layer of Biodentine was placed on the floor and around the mesial orifice (Figure 6).
In order to reinforce the remaining tooth structure and avoid any aggressive prosthetic procedures, it was elected to conservatively restore the tooth using FRC. EverX Posterior (GC Dental Products Corp., Aichi, Japan) was chosen for the procedure. After the setting of Biodentine, the adhesive protocol was followed, which included etching with 36% phosphoric acid (Conditioner 36, Dentsply DeTrey) for 10 seconds, a thorough washing with water and brief blot drying. Two coats of the total etch bonding agent (Prime and Bond NT, Dentsply Caulk, Milford, DE, USA) was applied with the applicator tip, lightly air-dried for 10 seconds, and light-cured for 10 seconds. Following this, the FRC was extruded from the compoule and compacted into the cavity incrementally (Figure 7). Each increment was light-cured for 20 seconds. The overlying 2 mm of the occlusal surface was reconstructed using nanofiller composite (CeramX, Dentsply DeTrey). Finishing and polishing of the restoration was carried out (Figures 8 and 9). The patient returned for follow-up after 6, 12, and 20 months, and the radiographs revealed appreciable healing in the periapical area (Figures 10, 11, 12, 13).
It is very well understood that ETT have special needs that far exceed the requirements of vital teeth. Although metallic restorations and conventional porcelain fused to metal crowns supported by radicular custom-made or prefabricated posts remain widespread, their invasiveness in the root as well as in the crown has been extensively criticized, with the consensus slowly shifting towards minimally invasive adhesive techniques.2 Advancements in adhesive technology, as well as new and stronger composite materials, have paved the way for conservative, highly aesthetically pleasing, and economical restorations that are bonded directly to the teeth.3 However, the use of composite resins in cusp-replacing posterior restorations is limited by the low flexural strength of the material.7
Fibre reinforcement in dentistry is gradually gaining momentum and is being used for various purposes such as FRC bridges, periodontal splints, orthodontic retainers, FRC resins, and posts. The incorporation of silanated E-glass fibres in the composite resin matrix results in an FRC material that provides fracture toughness greater than dentin and almost double that of conventional composites.8 The mechanical advantages provided by FRCs are their flexural strength, fatigue strength, elastic modulus, and bond strength.9 Two of the mechanisms by which fibres exert high strain to failure on a brittle composite matrix are by acting as a stress-bearing component and by arresting crack propagation or by crack deflection. Thus, the fracture pattern under load is changed resulting in a favourable mode of failure that is easily restorable, and the teeth concerned may be maintained in clinical service without any additional treatment.310 Although extensive research on FRCs has been carried out in vitro, limited research has assessed the clinical use and longevity of FRCs for restorative purpose.56911 Visser et al. concluded that the inclusion of fibres, whether placed as a substructure or embedded in the composite resin itself, significantly increased the fracture strength values of the restorative material.12
In the case described above, the use of FRC was very advantageous. It not only eliminated the need for a conventional crown, which would have required the removal of additional tooth structure, but also served as a coronal reinforcement. Furthermore, the resistance to fracture of endodontically treated teeth is directly proportional to the amount of remaining dentin structure. Zogheib et al. evaluated the fracture resistance of weakened roots (1 mm of remaining dentin thickness) restored with glass fibre posts, composite resin cores, and complete metal crowns, and concluded that in severely weakened roots, the use of a glass fibre post did not reinforce the roots to the same levels of fracture resistance as the non-weakened roots.13 Hence, in this case, the use of a glass fibre post was not suitable due to the compromised root dentin thickness.
The use of Biodentine, as a biomimetic restoration has been well documented. The material demonstrates favourable mechanical properties (elastic modulus, compressive strength, and microhardness) that are very similar to dentin. Biodentine attains a compressive strength of more than 200 MPa at 24 hours, which is more than EverX Posterior FRC (129 MPa). A specific feature of Biodentine is its capacity to continue improving with time over several days, reaching 300 MPa after one month. This value becomes quite stable and is in the range of the compressive strength of natural dentine (297 MPa). Hence, Biodentine has often been referred to as a 'dentin substitute'. Moreover, the material possesses good handling characteristics with favourable setting kinetics (12 minutes) and has the ability to stimulate hard tissue formation. The alkaline environment at the interface of Biodentine and dentin opens a path via which the dentin substitute can enter the tubules. At the entrance of the dentine tubules, some mineral re-crystallisation occurs, creating mineral tags. This induces the micromechanical anchorage of Biodentine, resulting in a bacteria-tight seal. This process continues over time, further improving the seal.1415 The use of Biodentine in this case allowed the compromised dentin around the orifice and the floor of the chamber to be replaced, with the additional aim of achieving hard tissue deposition to reinforce the strength.
In this case, the extensive amount of tooth structure sacrificed to pathology and endodontic treatment supported the use of a minimally invasive FRC restoration instead of a full crown. This technique allowed the conservation of sound dentin and peripheral enamel, thereby influencing the marginal stability.2 This technique can be considered to be an economical, practical, and tooth-saving alternative to the more expensive and invasive process of prosthetic rehabilitation. However, since minimal clinical data exist regarding the use of FRCs, the importance of long-term follow-up cannot be overemphasized.
Figures and Tables
References
1. Stankiewicz NR, Wilson PR. The ferrule effect: a literature review. Int Endod J. 2002; 35:575–581.

2. Rocca GT, Rizcalla N, Krejci I. Fibre-reinforced resin coating for endocrown preparations: a technical report. Oper Dent. 2013; 38:242–248.

3. Shivanna V, Gopeshetti PB. Fracture resistance of endodontically treated teeth restored with composite resin reinforced with polyethylene fibres. Endodontology. 2013; 24:73–79.
4. Yeng T, Messer HH, Parashos P. Treatment planning the endodontic case. Aust Dent J. 2007; 52:Supplement 1. S32–S37.

5. Garoushi S, Tanner J, Vallittu P, Lassila L. Preliminary clinical evaluation of short fibre-reinforced composite resin in posterior teeth: 12-months report. Open Dent J. 2012; 6:41–45.

6. Garoushi S, Mangoush E, Vallittu M, Lassila L. Short fibre reinforced composite: a new alternative for direct onlay restorations. Open Dent J. 2013; 7:181–185.

7. Xia Y, Zhang F, Xie H, Gu N. Nanoparticle-reinforced resin-based dental composites. J Dent. 2008; 36:450–455.

8. GC India: GC EverX Posterior. updated 2015 Dec 12. Available from: http://www.gcindiadental.com/products/compositerestoratives/everx-posterior.
9. Garoushi SK, Shinya A, Shinya A, Vallittu PK. Fibre reinforced onlay composite resin restoration: a case report. J Contemp Dent Pract. 2009; 10:104–110.
10. Garoushi S, Vallittu PK, Lassila LV. Continuous and short fibre reinforced composite in root post-core system of severely damaged incisors. Open Dent J. 2009; 3:36–41.

11. Deliperi S. Direct fibre-reinforced composite restoration in an endodontically-treated molar: a three-year case report. Oper Dent. 2008; 33:209–214.

12. Visser HJ, Brandt PD, de Wet AF. Fracture strength of cusp-replacing fibre-strengthened composite restorations. SADJ. 2014; 69:202.
13. Zogheib LV, Pereira JR, do Valle AL, de Oliveira JA, Pegoraro LF. Fracture resistance of weakened roots restored with composite resin and glass fibre post. Braz Dent J. 2008; 19:329–333.

14. Priyalakshmi S, Ranjan M. Review on Biodentine-a bioactive dentin substitute. IOSR J Dent Med Sci. 2014; 13:13–17.

15. Biodentine-Septodont R&D Department: Biodentine. Active biosilicate technology. Scientific file. updated 2016 Jan 31. Available from: http://www.plandent.no/images/Marketing/Infosenter/Biodentine%20Scientific%20File_web_dokumentasjon.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print













 XML Download
XML Download