Abstract
Objectives
The aim of this study was to compare the push-out bond strength and dentinal tubule penetration of root canal sealers used with coated core materials and conventional gutta-percha.
Materials and Methods
A total of 72 single-rooted human mandibular incisors were instrumented with NiTi rotary files with irrigation of 2.5% NaOCl. The smear layer was removed with 17% ethylenediaminetetraacetic acid (EDTA). Specimens were assigned into four groups according to the obturation system: Group 1, EndoRez (Ultradent Product Inc.); Group 2, Activ GP (Brasseler); Group 3, SmartSeal (DFRP Ltd. Villa Farm); Group 4, AH 26 (Dentsply de Trey)/gutta-percha (GP). For push-out bond strength measurement, two horizontal slices were obtained from each specimen (n = 20). To compare dentinal tubule penetration, remaining 32 roots assigned to 4 groups as above were obturated with 0.1% Rhodamine B labeled sealers. One horizontal slice was obtained from the middle third of each specimen (n = 8) and scanned under confocal laser scanning electron microscope. Tubule penetration area, depth, and percentage were measured. Kruskall-Wallis test was used for statistical analysis.
Results
EndoRez showed significantly lower push-out bond strength than the others (p < 0.05). No significant difference was found amongst the groups in terms of percentage of sealer penetration. SmartSeal showed the least penetration than the others (p < 0.05).
Conclusions
The bond strength and sealer penetration of resin-and glass ionomer-based sealers used with coated core was not superior to resin-based sealer used with conventional GP. Dentinal tubule penetration has limited effect on bond strength. The use of conventional GP with sealer seems to be sufficient in terms of push-out bond strength.
Although the reduction or elimination of microorganisms responsible for endodontic diseases and failure is the primary goal of endodontic treatment, it is not possible to create a microorganism-free medium inside a root canal system despite current root canal disinfection agents and techniques.12 A corono-apical seal inside the root canal system is essential to prevent the proliferation of residual microorganisms that cause reinfection.
Adhesive applications in restorative dentistry have resulted in the monoblock concept, consisting of a continuous bond among the root dentin, core material, and root canal sealer that is believed to enhance the sealing ability and reinforce the residual root structure against vertical root fracture.34 As gutta-percha (GP) does not bond to dentin, it is crucial to use it with a root canal sealer to adhere to dentin.5 It has previously been shown that an endodontic sealer should adhere both to the GP cone and dentin walls.6 However, sealers can adhere to the root canal wall, but none are able to bond to GP, leaving a gap through which bacteria may pass.7 Thus, obturation systems using coated core materials allowing the adhesion between the sealer and core, such as EndoRez (Ultradent Product Inc., South Jordan, UT, USA), Activ GP (Brasseler, Savannah, GA, USA) and SmartSeal (DFRP Ltd. Villa Farm, Stamford, UK) have been produced.
Adhe s ion to dentin is mostly based on the micromechanical retention obtained from the collagen matrix in the intertubular dentin exposed during the hybridization process,89 and minimally based on the effect of dentinal tubules10 and chemical interaction between the dentin and adhesive systems.11 Dentinal tubule penetration of the sealer creates a micromechanical lock and enhances the retention and resistance to dislocation of the sealer.12 In addition, it allows the sealer to carry its antimicrobial effect into dentinal tubules and increases the contact surface between the sealer and dentin, thus enhancing sealing ability.13
Tay and Pashley defined monoblock units according to the number of gaps between the core material and dentin.3 Filling of root canals with only a filling material such as mineral trioxide aggregate (MTA) creates a gap between the dentin and MTA and therefore is defined as a primary monoblock. Usage of a sealer and a core material creates two gaps, in which one is between dentin and the sealer and the other is between the sealer and core material, and is defined as a secondary monoblock. Usage of a sealer and a coated core material creates an extra third gap between the coating layer and the core material and is defined as a tertiary monoblock.
According to the Tay and Pashley classification, the EndoRez, Activ GP, and SmartSeal create a tertiary monoblock unit in the root canal.3 The EndoRez includes the use of a resin-coated conventional GP cone with a hydrophilic urethane dimethacrylate-based dual-cured bondable resin sealer that does not require an additional dentin adhesive. Activ GP is a similar system that includes the usage of a glass ionomer-coated conventional GP with a glass ionomer-based root canal sealer. SmartSeal is a recent filling system that uses a synthetic core material called Smartpoint that includes zirconium oxide and polyamide, and an epoxy-amine resin-based root canal sealer called Smartpaste.14 The push-out bond strength and dentinal tubule penetrations of these materials that create tertiary monoblock units have not yet been evaluated.
The aim of this study was to compare the push-out bond strength and dentinal tubule penetration of these tertiary monoblock units consisting of resin- and glass ionomer-based sealers used with coated GP, to a secondary monoblock unit consisting of a resin-based sealer used with conventional GP. The null hypothesis was that there is no difference in the bond strength and dentinal tubule penetration among the test groups.
This study was approved by the Hacettepe University Ethics Board and Commissions (number 09/01). Forty freshly extracted, mature, and single-rooted intact mandibular incisors of visually similar size were used in push-out bond tests. The teeth with two canals were eliminated during the access cavity preparation and the ones with single canal were selected for the experiment. The same operator performed all experimental procedures. Teeth were decoronated to obtain 15 mm length roots, and the working length was established as 14 mm. Root canals were instrumented with RaCe nickel titanium (NiTi) Rotary files (FKG Dentaire SA, La Chaux-de-Fonds, Switzerland) up to a size 40/0.04 in the presence of RC-Prep (Premier Dental Products, Tulsa, OK, USA) as a lubricant. Root canals were irrigated with 2 mL of 2.5% sodium hypochlorite (NaOCl) between each file. After the instrumentation, 2.5% NaOCl was inserted into the root canal and ultrasonically activated for 1 minute. Then, the smear layer was removed using 17% ethylenediaminetetraacetic acid (EDTA) for 1 minute. The EDTA was freshly prepared at Hacettepe University Faculty of Pharmacy before the experiment. After drying root canals with paper points, 40 specimens were randomly assigned into 4 groups (n = 10) and obturated by single cone technique as follows:
Group 1, EndoRez sealer and a size 40/0.04 EndoRez point;
Group 2, Activ GP sealer and a size 40/0.04 Activ GP point;
Group 3, Smartpaste sealer and a size 40/0.04 Smartpoint point;
Group 4, AH 26 sealer (Dentsply de Trey, Konstanz, Germany) and a size 40/0.04 GP point. All root canal sealers were prepared according to the manufacturers' instructions and placed in the canal with a lentulo spiral. After the obturation process, specimens were coronally sealed with Coltosol F (Coltene/Whaledent Gmbh, Langenau, Germany) and stored in 100% humidity for 1 week to allow complete setting of the sealer.
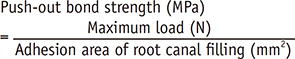
Coronal seal was removed and specimens were molded into cylindrical epoxy resin blocks. Two horizontal slices approximately 1 mm in thickness were obtained from the most coronal third of the roots in the corono-apical direction of each specimen by using a 0.3 mm low-speed water-cooled precision saw (IsoMet 5000, Buehler, Lake Bluff, IL, USA). By this method, 20 specimens were obtained for each test group (n = 20). After measuring the thickness of the slices with a digital caliper, the filling material was loaded with a 0.76 mm diameter stainless steel cylindrical plunger. The tip of the plunger was positioned and sized to contact only the core material. The push-out force was applied from apical to coronal direction because of the convergence of the root canal. Loading was performed on a universal testing machine, (Lloyd LRX, Lloyd Instruments Ltd., Fareham, UK) at a constant crosshead speed of 1 mm/minute until bond failure occurred. Maximum load was recorded in Newton (N) by using Nexygen data analysis software (Lloyd Instruments Ltd.), and push-out bond strength was calculated in megapascals (MPa), according to the formula below:15
where 'r' is the radius of root canal filling and 'h' is the thickness of the slice. Coronal and apical radius of the filling material was assumed to be the same (1 mm). 'π' is accepted as 3.14.
Thirty-two freshly extracted, mature, and single-rooted intact mandibular incisors were selected, decoronated, chemo-mechanically prepared, and randomly assigned into four groups for obturation (n = 8) as described above. Before the obturation procedure, root canal sealers were mixed with 0.1% Rhodamine B dye (Sigma Aldrich Co., St Louis, MO, USA) for fluorescence under a confocal laser scanning microscope (CLSM) and placed in the canal with a lentulo spiral.16 After the obturation, specimens were stored at 37℃ and 100% humidity for 1 week to allow complete setting of the sealers.
Specimens were molded into cylindrical epoxy resin blocks. One horizontal slice 1 mm in thickness was obtained from the middle third of the specimen using the same 0.3 mm low-speed water-cooled precision saw (IsoMet, Buehler). The specimens were mounted onto a cover glass and scanned under a CLSM (LSM Pascal, Carl Zeiss, Jena, Germany) by using the 543 nm wavelength of helium laser under ×2.5 magnification (Numerical apperture, NA 0.12). The pinhole was kept at 78 µm in all of the recordings. The first optical image section, which began at the surface of the specimen, was discarded. The next optical section, which was focused about 100 µm deeper, was acquired.
Images were evaluated by using LSM Image Examiner Software (Carl Zeiss). The circumference of the root canal and the circumference of sealer penetration areas were outlined and measured. The ratio of these two measurements was calculated as the percentage of sealer covering the canal wall. To measure the depth of penetration, the deepest point of penetration was measured from the canal wall to the point of maximum sealer penetration. The whole penetration area of the sealer was also calculated. The area of the canal and whole area that the sealer penetrated were measured, and the difference was calculated as the penetration area of the sealer. Figures 1 and 2 show the measurement of dentin tubule penetration parameters.
There was a significant difference amongst bond strength values of the test groups (p < 0.05). Pairwise comparisons with Dunn's test showed that EndoRez was significantly different from the other groups (p < 0.05), while no difference was observed amongst the others. Table 1 shows the statistical result of push-out bond strength of the test groups.
No significant difference was found amongst the percentage of sealer penetration of the groups. SmartSeal showed the least area and depth of tubule penetration (p < 0.05), while no difference was found amongst the others. Table 2 shows the statistical result of area, depth, and percentage of dentinal tubule penetration of the test groups.
All groups in this study showed measurable adhesive properties and dentinal tubule penetrations. The null hypothesis that there is no difference among the groups tested was rejected. EndoRez showed the lowest push-out bond strength, while there were no significant differences among the other groups. No difference was found among the groups in terms of the percentage of dentinal tubule penetration, but SmartSeal showed significantly lower area and depth of dentinal tubule penetration while no significant difference was found among the others.
The push-out test has been used to evaluate the dentin bond strength of root canal filling materials.1417 This method allows the standardization of the specimens and evaluation of very low bond strength values.18 Although it allows the assessment of bond strength at different root levels, we obtained specimens from the coronal third of the roots to prevent the plunger (0.76 mm tip size) from being larger than the core diameter and touching the dentin walls. It has also previously been shown that the location of the slice did not have a significant effect on bond strength.141719
CLSM was used for the evaluation of dentinal tubule penetrations instead of scanning electron microscope (SEM) because it allows standard and reproducible three-dimensional imaging of the samples without damaging them.162021 At the same time, it allows evaluation of tubule penetration and adaptation of sealer quickly and objectively in panoramic images obtained at lower magnifications via the fluorescent effect of Rhodamine B.22 It has previously been shown that Rhodamine B is a safe dye that has no effect on the setting of the sealers.1623
EndoRez is the first-generation methacrylate resin-based root canal sealer using nonacidic hydrophilic resin monomers.24 Its hydrophilic character also allows the material to flow into moist accessory canals and dentinal tubules to create resin tags for retention and seal after the removal of the smear layer.2425 There is a lack of chemical union between the polyisoprene content of GP and methacrylate resin-based sealers. Therefore, EndoRez sealer is used with polybutadiene-diisocyanate methacylate resin-coated GP to allow the chemical bonding between GP and the sealer.25 Meanwhile, coatings of the core structure might be damaged during the lateral compaction procedure. Therefore, the single cone obturation technique has been used for the obturation of root canals.26 In this study, EndoRez showed the lowest bond strength to coronal radicular dentin (0.14 MPa), approximately ten times lower than that of AH 26 (1.41 MPa), which is a classic epoxy resin-based root canal sealer generally accepted as the gold standard. These findings are very similar to the findings of a study that compared the regional bond strength of resin-based sealers after the use of EDTA as a final irrigant.17 It has also been shown that EndoRez had the lowest bond strength values amongst five different type of sealers including Activ GP and AH Plus.19
Removal of the smear layer before root canal filling is generally advised to allow the sealer to penetrate into dentinal tubules and to contact root dentin.12 In this study, the smear layer was removed with EDTA and NaOCl, as has been reported to be the most effective method.27 The manufacturer of EndoRez recommends EDTA as the final irrigation solution rather than NaOCl. NaOCl is an oxidizing agent and inhibits the polymerization of resins, thus reducing resin bond strength.28 AH 26 and Smartpaste are both epoxy-amine resin-based root canal sealers. The low shrinkage during setting and dimensional stability of epoxy-amine-based sealers have been previously shown.2930 In this study, their bond strength was found to be significantly higher than EndoRez. This finding may reveal that methacrylate-based sealers are more affected by NaOCl oxidization than epoxy-amine-based ones. EndoRez is a methacrylate-based root canal sealer that creates long resin tags into dentinal tubules as a result of its hydrophilic character.242531 Similar to a previous study,19 long resin tags of EndoRez were shown in this study. Despite long resin tag formation, the extremely high cavity-configuration factor (C-Factor) of the root canal system32 and the polymerization shrinkage of the methacrylate-based sealer33 might be the reasons for the very low bond strengths of this sealer.
SmartSeal is a filling system comprised of a Smartpoint and a Smartpaste. Smartpoint is a radiopaque polymeric synthetic core material consisting of a zirconium oxide/polyamide blend and is coated with a radiolucent hydrophilic polymer sheet of acrylonitrile/vinyl pyrrolidone. It absorbs water from the tooth tissue and expands laterally to adapt to the shape of the root canal. Smartpaste is a radiopaque epoxy-amine resin-based root canal sealer that includes an active polymer that undergoes hydrophilic swelling when in contact with moisture in root canals to allow the sufficient filling of dentinal tubules. A superior adhesion to root canal walls might be expected because of the swelling of both Smartpoint and Smartpaste. However, no significant difference in bond strength was found between Smartpoint/Smartpaste filling and AH 26/GP filling. This finding is similar to another study14 that found no difference in the bond strength of these systems when used with single cone or cold lateral compaction technique. Moreover, they showed that bond failure was mainly adhesive to dentin for all groups. Although no difference was found amongst the groups in terms of percentage of sealer penetration, Smartpaste showed the least penetration area and depth. The high viscosity of Smartpaste might be the reason for this low penetration ability. Moreover, it seems that the swelling potential of Smartpaste and Smartpoint did not enhance the penetration ability of the material. Despite the low penetration ability of Smartseal, it showed similar bond strength to AH 26. This result is not surprising when considering that it has previously been shown that dentinal tubule penetration has minimal effect on adhesion ability.10
Glass ionomer sealers, including polyacrylic acid, have been shown to have a chelating reaction with the calcium content of dentin matrix.34 In this study, the push-out bond strength of Activ GP was lower than SmartSeal and AH 26, but no significant difference was found amongst them. Also, the bond strength of sealer to GP might be enhanced with the glass-ionomer coating of the core material. Fisher et al.19 compared the push-out bond strength of EndoRez and Activ GP obturation systems to Resilon/Epiphany system, GP with AH Plus, and GP with KerrEWT. They found that epoxy resin-based AH Plus has the highest bond strength to dentin, and Activ GP and Kerr EWT were superior to EndoRez and Resion/Epiphany systems, which is similar to our results.
Within the limitations of this study, it can be concluded that the use of coated core materials with resin- and glass ionomer- based sealers did not enhance the bond strength of the root canal obturation material. Dentinal tubule penetration has limited effect on push-out bond strength of the root canal sealers.
Figures and Tables
 | Figure 2Measurement of percentage and maximum depth of sealer penetration using LSM Image Examiner Software (Carl Zeiss). |
Table 1
Push-out bond strength of the test groups (MPa)
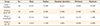
Table 2
Dentinal tubule penetration area (mm2), depth (mm), and percentage (%) of the test groups

Acknowledgement
This study has been supported by the Scientific Research Projects Coordination Unit of Hacettepe University (09 D01 201 003 (4752)).
References
1. Rôças IN, Neves MA, Provenzano JC, Siqueira JF Jr. Susceptibility of as-yet-uncultivated and difficult-toculture bacteria to chemomechanical procedures. J Endod. 2014; 40:33–37.

2. Siqueira JF Jr, Lima KC, Magalhães FA, Lopes HP, de Uzeda M. Mechanical reduction of the bacterial population in the root canal by three instrumentation techniques. J Endod. 1999; 25:332–335.

3. Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangible goal. J Endod. 2007; 33:391–398.

4. Kim YK, Grandini S, Ames JM, Gu LS, Kim SK, Pashley DH, Gutmann JL, Tay FR. Critical review on methacrylate resin-based root canal sealers. J Endod. 2010; 36:383–399.

5. Hammad M, Qualtrough A, Silikas N. Evaluation of root canal obturation: a three-dimensional in vitro study. J Endod. 2009; 35:541–544.

6. Caicedo R, von Fraunhofer JA. The properties of endodontic sealer cements. J Endod. 1988; 14:527–534.

7. Teixeira FB, Teixeira EC, Thompson JY, Trope M. Fracture resistance of roots endodontically treated with a new resin filling material. J Am Dent Assoc. 2004; 135:646–652.

8. Tao L, Pashley DH. Shear bond strengths to dentin: effects of surface treatments, depth and position. Dent Mater. 1988; 4:371–378.

9. Tagami J, Tao L, Pashley DH. Correlation among dentin depth, permeability, and bond-strength of adhesive resins. Dent Mater. 1990; 6:45–50.

10. Schwartz RS. Adhesive dentistry and endodontics. Part 2: bonding in the root canal system-the promise and the problems: a review. J Endod. 2006; 32:1125–1134.

11. Yoshida Y, Nagakane K, Fukuda R, Nakayama Y, Okazaki M, Shintani H, Inoue S, Tagawa Y, Suzuki K, De Munck J, Van Meerbeek B. Comparative study on adhesive performance of functional monomers. J Dent Res. 2004; 83:454–458.

12. White RR, Goldman M, Lin PS. The influence of the smeared layer upon dentinal tubule penetration by plastic filling materials. J Endod. 1984; 10:558–562.

13. Sen BH, Pişkin B, Baran N. The effect of tubular penetration of root canal sealers on dye microleakage. Int Endod J. 1996; 29:23–28.

14. Economides N, Gogos C, Kodonas K, Beltes C, Kolokouris I. An ex vivo comparison of the push-out bond-strength of a new endodontic filling system (Smartseal) and various gutta-percha filling techniques. Odontology. 2012; 100:187–191.

15. Nagas E, Cehreli ZC, Durmaz V, Vallittu PK, Lassila LV. Regional push-out bond-strength and coronal microleakage of Resilon after different light-curing methods. J Endod. 2007; 33:1464–1468.

16. Gharib SR, Tordik PA, Imamura GM, Baginski TA, Goodell GG. A confocal laser scanning microscope investigation of the epiphany obturation system. J Endod. 2007; 33:957–961.

17. Patil SA, Dodwad PK, Patil AA. An in vitro comparison of bond-strengths of Gutta-percha/AH Plus, Resilon/ Epiphany self-etch and EndoREZ obturation system to intraradicular dentin using a push-out test design. J Conserv Dent. 2013; 16:238–242.

18. Onay EO, Ungor M, Ari H, Belli S, Ogus E. Push-out bond-strength and SEM evaluation of new polymeric root canal fillings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:879–885.

19. Fisher MA, Berzins DW, Bahcall JK. An in vitro comparison of bond-strength of various obturation materials to root canal dentin using a push-out test design. J Endod. 2007; 33:856–858.

20. Ordinola-Zapata R, Bramante CM, Graeff MS, del Carpio Perochena A, Vivan RR, Camargo EJ, Garcia RB, Bernardineli N, Gutmann JL, de Moraes IG. Depth and percentage of penetration of endodontic sealers into dentinal tubules after root canal obturation using a lateral compaction technique: a confocal laser scanning microscopy study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:450–457.

21. Vadhana S, Latha J, Velmurugan N. Evaluation of penetration depth of 2% chlorhexidine digluconate into root dentinal tubules using confocal laser scanning microscope. Restor Dent Endod. 2015; 40:149–154.

22. D'Alpino PH, Pereira JC, Svizero NR, Rueggeberg FA, Pashley DH. Use of fluorescent compounds in assessing bonded resin-based restorations: a literature review. J Dent. 2006; 34:623–634.
23. Patel DV, Sherriff M, Ford TR, Watson TF, Mannocci F. The penetration of RealSeal primer and Tubliseal into root canal dentinal tubules: a confocal microscopic study. Int Endod J. 2007; 40:67–71.

24. Zmener O, Pameijer CH, Serrano SA, Vidueira M, Macchi RL. Significance of moist root canal dentin with the use of methacrylate-based endodontic sealers: an in vitro coronal dye leakage study. J Endod. 2008; 34:76–79.

25. Tay FR, Loushine RJ, Monticelli F, Weller RN, Breschi L, Ferrari M, Pashley DH. Effectiveness of resin-coated gutta-percha cones and a dual-cured, hydrophilic methacrylate resin-based sealer in obturating root canals. J Endod. 2005; 31:659–664.

26. Gillespie WT, Loushine RJ, Weller RN, Mazzoni A, Doyle MD, Waller JL, Pashley DH, Tay FR. Improving the performance of EndoREZ root canal sealer with a dual-cured two-step self-etch adhesive. II. Apical and coronal seal. J Endod. 2006; 32:771–775.

27. Goldman LB, Goldman M, Kronman JH, Lin PS. The efficacy of several irrigating solutions for endodontics: a scanning electron microscopic study. Oral Surg Oral Med Oral Pathol. 1981; 52:197–204.

28. Ari H, Yaşar E, Belli S. Effects of NaOCl on bondstrengths of resin cements to root canal dentin. J Endod. 2003; 29:248–251.

29. McMichen FR, Pearson G, Rahbaran S, Gulabivala K. A comparative study of selected physical properties of five root-canal sealers. Int Endod J. 2003; 36:629–635.

30. Schäfer E, Zandbiglari T. Solubility of root-canal sealersin water and artificial saliva. Int Endod J. 2003; 36:660–660.
31. Sevimay S, Kalayci A. Evaluation of apical sealing ability and adaptation to dentine of two resin-based sealers. J Oral Rehabil. 2005; 32:105–110.

32. Tay FR, Loushine RJ, Lambrechts P, Weller RN, Pashley DH. Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod. 2005; 31:584–589.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download