Abstract
Objectives
This study aimed to compare the accuracy of conventional intraoral (CI) radiography, photostimulable phosphor (PSP) radiography, cone beam computed tomography (CBCT) and multidetector computed tomography (MDCT) for detection of strip and root perforations in endodontically treated teeth.
Materials and Methods
Mesial and distal roots of 72 recently extracted molar were endodontically prepared. Perforations were created in 0.2, 0.3, or 0.4 mm diameter around the furcation of 48 roots (strip perforation) and at the external surface of 48 roots (root perforation); 48 roots were not perforated (control group). After root obturation, intraoral radiography, CBCT and MDCT were taken. Discontinuity in the root structure was interpreted as perforation. Two observers examined the images. Data were analyzed using Stata software and Chi-square test.
Results
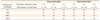
The sensitivity and specificity of CI, PSP, CBCT and MDCT in detection of strip perforations were 81.25% and 93.75%, 85.42% and 91.67%, 97.92% and 85.42%, and 72.92% and 87.50%, respectively. For diagnosis of root perforation, the sensitivity and specificity were 87.50% and 93.75%, 89.58% and 91.67%, 97.92% and 85.42%, and 81.25% and 87.50%, respectively. For detection of strip perforation, the difference between CBCT and all other methods including CI, PSP and MDCT was significant (p < 0.05). For detection of root perforation, only the difference between CBCT and MDCT was significant, and for all the other methods no statistically significant difference was observed.
Root perforation is a mechanical or pathological communication between the root canal system and the supporting tissues of teeth or the oral cavity.1 It is an undesirable and often iatrogenic accident that can occur at any stage of root canal preparation. Root perforation, which comprises about 10% of all endodontic failures, may compromise the health of periradicular tissues and disrupts the integrity of the root.1,2 The location of the perforation, size and time of detection can help select the proper treatment, minimize bone loss and predict the outcome; thus, significantly affect the prognosis of root perforations.3
Root perforation may be caused by creating a ledge in the canal wall during initial instrumentation, perforating through the side of the root at the point of canal obstruction or root curvature, using an instrument too long or too large, and perforating directly through the apical foramen or creating a hole in the lateral surface of the root.3,4 Strip perforation is a longitudinal perforation caused by improper instrumentation through a thin wall (danger zone) in the root. In the danger zone there is less tooth structure compared to the more peripheral portion (safety zone) of the root dentin (Figure 1).5,6
Various instruments and techniques such as electronic apex locators, operative microscopes, endoscopes and optical coherence tomography scan have been suggested for detection of perforations; but none of these can help in diagnosis of perforation in endodontically treated roots.7 Radiographic examination is an essential component of the management of endodontic complications. Intraoral radiographs (either film-based or digital) are still the most accepted and widely used imaging modalities in endodontics. However, such images have inherent limitations that arise primarily from two-dimensional (2D) projection of three-dimensional (3D) structures, which lead to geometric distortion, and restrict the information regarding the size, extension, and location of root/periapical lesions.8,9
Computed tomography (CT) is one of the important imaging modalities that enables 3D assessment of craniofacial structures and allows accurate assessment of both hard and soft tissues with wide ranges of contrast and latitude.10 The introduction of multidetector computed tomography (MDCT) presented a great evolutionary step in the development of CT. MDCT scans can provide thin, multiple and overlapping slices that can be rapidly reconstructed resulting in high-quality images.11 However, excessive radiation exposure, increased cost and limited availability impede the routine use of this technology for dental application.10 Cone beam computed tomography (CBCT) is a radiographic imaging system developed specifically for dentistry. This three-dimensional imaging system has a great potential for application in the field of endodontics.8 Various CBCT systems have differences in resolution and type of detectors that can in turn affect the quality of imaging and diagnostic outcomes.12
Nonspecific clinical symptoms and limited capacity of periapical radiographs sometimes make the correct diagnosis of root perforations challenging.13 Correct and early diagnosis of root perforation and determining the exact location and size of the perforation are necessary to plan an appropriate treatment.3 This in vitro study was conducted to evaluate and compare the diagnostic ability of different radiographic systems including conventional intraoral radiography, photostimulable phosphor (PSP) radiography, CBCT and MDCT in detecting simulated strip and root perforations with different clinical perforation sizes.
Seventy-two recently extracted human mandibular molar teeth with mature apices were selected and stored in purified filtered water. Surfaces of the roots were examined to ensure absence of any defects visually and with a magnifying glass. Teeth with fractures, cracks, external or internal root resorption, open apices, endodontically treated roots or non-accessible root canals due to calcification were excluded. After standard access cavity preparation and coronal pulp excavation, the patency was established with a size 10 K File (Mani Inc., Utsunomiya Tochigi, Japan). The root canals were cleaned and shaped using the step back technique with K files of sizes 15 to 30 and preparation was completed using a F3 ProTaper file (Dentsply Maillefer, Ballaigues, Switzerland) according to the manufacturer's protocol. The canals were repeatedly irrigated with a freshly prepared 2% solution of sodium hypochlorite (NaOCl) using a 5cc syringe and a 27 gauge needle. After completion of the procedure, canals were rinsed with 2 mL of distilled water.
One hundred forty-four mesial and distal roots of 72 teeth were divided into three groups (n = 48 in each group). One of the groups was not perforated (control group). In strip perforation and root perforation groups, mesiolingual canal of the mesial root and distal or distolingual canal of the distal root were perforated in 0.2 mm, 0.3 mm and 0.4 mm sizes. According to Shemesh et al.'s study, perforation in the coronal third or furcal area of the root is known as a strip perforation while a perforation in other sites of the root is known as a root perforation.7 To create root perforations, a ledge was created on the root curvature with Gates Glidden drills No. 1 to 3 (Mani inc.) and it was continued until a thin layer of dentin remained on the lateral side of the root wall. After that, depending on perforation diameter, a size 20, 30 or 40 K file was forced against the thin wall until the root wall was perforated. All root perforations were created on the mesial or distal side of the middle or apical part of the root.12 Strip perforations 1 to 3 mm below the furcation were created by over instrumentation of the danger zone using a No. 2 or 3 Gates Glidden drill until it seemed that the root was almost perforated and dentin chips extruded through the lateral surface of the root. Then, depending on perforation diameter, a size 20, 30 or 40 K file was forced against the thin wall until the root wall was perforated. The perforation was widened so that the file could pass through the perforation easily.3,5
The teeth were dried using No. 35 and 30 paper points (Ariadent, Tehran, Iran). AH26 sealer (Dentsply DeTrey, Konstanz, Germany) was mixed according to the instructions of the manufacturer and placed into the canal. Size 35 gutta-percha (Gapadent, Tianjin, China) was coated with the sealer and placed into the root canal. Roots were filled by the lateral compaction technique using a size 30 spreader (Mani Inc.) and size 25 gutta-percha cones. Finally, gutta-percha was condensed in the orifices of canals to remove the voids. The teeth were placed in premade sockets in dry human mandibles bilaterally in the posterior region. Impression material was used to fix the teeth in the mandibular sockets. The mandibular bones were coated with dental wax of 1.5 mm thickness, which had similar attenuation properties to human soft tissues.
Intraoral conventional and digital radiography were done using E Speed dental films (Kodak, Rochester, NY, USA) and Digora Optime (Soredex, Tuusula, Finland) size 2 PSP receptor (85 - 167 microns pixel size and 6 - 8 LP/mm resolution) with Minray intraoral x-ray unit (Soredex). To hold the image receptors in a fixed and repeatable position, a film holder was made with putty paste (Asia Chemi Teb Mfg Co., Tehran, Iran). The mandible was placed on a table and mounted on a wooden block to facilitate the movement of the x-ray tube. Two images were taken from each tooth in two different directions including perpendicularly and 10° distal tube shift relative to the long axis of the teeth. Exposure times were 0.2 and 0.12 seconds for conventional and PSP radiography, respectively, with the exposure settings of 7 mA and 60 kVp. Conventional radiographs were processed in an automatic processor (Hope DentalMax X-ray processor, ClassicXray. com, Rolla, MO, USA) and then mounted (Figure 2). Digital receptors were kept inside a black plastic bag to minimize the effect of environmental light and were then scanned using a Digora scanner (Soredex). The images were stored in JPEG format (Figure 3).
CBCT images were obtained using Cranex 3D (Soredex) in an upright position. The mandibles were fixed in a chin rest similar to the location of the patient's jaw. Radiation was emitted at high-resolution mode with 90 kVp, 4 mA, 12.6 seconds, voxel size of 0.2 × 0.2 × 0.2 mm, field of view of 6 × 8 cm and 0.2 mm slice thickness. The images were reconstructed at 0.2 mm intervals and stored in Digital Imaging and Communications in Medicine (DICOM) format (Figure 4). MDCT images were obtained using a Somatom Emotion 16 (Siemens, München, Germany) operated at 130 kVp and 80 mAs. The specimens were stabilized on the gantry, and axial scan images were adjusted parallel to the occlusal plane of the teeth. Images were obtained at a slice thickness of 0.75 mm and were reconstructed to 0.2 mm intervals and finally stored in DICOM format (Figure 5).
Any discontinuity in the peripheral portion of the root that is seen either at the furcation area (strip perforation) or at the external area (root perforation), either filled with a radiopaque filling material (i.e. gutta-percha or cement or both) or appeared like a radiolucent defect was diagnosed as a perforation.7 Two observers including two dentomaxillofacial radiologists (with 5 and 18 years of experience) who were not involved in any stages of the study were instructed to separately and randomly view the images while grading their observations as perforation, no perforation or probable perforation when it could not be clearly detected (questionable). CBCT Cranex 3D and MDCT images were reviewed in three reconstruction planes (axial, coronal and sagittal). A 15-inch liquid crystal display monitor (Toshiba satellite L40, Tokyo, Japan) with 1367 × 768 pixels resolution was used for interpretation of the images in a dimly lit room without time restrictions. The observers were allowed to adjust brightness, contrast and magnification of the images to obtain the best visual result.
To estimate the sensitivity and specificity of the imaging techniques, the number of truly detected perforated roots ('questionable' and 'perforation') and the number of truly detected sound roots were divided by the total number of perforated roots and the total number of non-perforated roots, respectively. These values were reported as a percentage using known simulated complications as the gold standard. The chi-square test was used to assess the correlation between two qualitative variations. To compare the variables such as image modalities, perforation locations and sizes, χ2 test was used. All statistical analyses were performed at a 95% confidence interval using statistical software (Stata version 11.2, Stata Corp, College Station, TX, USA). Inter-observer and intra-observer agreement for each radiographic technique were calculated using Cohen's kappa values. A kappa value below 0.40 was indicative of poor agreement, a kappa value of 0.40 to 0.75 indicated intermediate to good agreement and a kappa value greater than 0.75 was indicative of excellent agreement beyond chance.
The overall sensitivity, specificity and accuracy of imaging techniques in diagnosis of perforations are shown in Table 1. Overall, CBCT was superior to CI, PSP and MDCT and the differences in this respect were statistically significant (p < 0.05). Although PSP was more accurate than CI, the difference was not significant (p = 0.637). MDCT had the lowest accuracy but no significant difference with CI or PSP (p > 0.05).
The sensitivity, specificity and accuracy of the imaging techniques based on the perforation site are listed in Table 2. According to Table 2, CBCT was significantly superior to CI and PSP in detecting strip perforations (p < 0.05), while there was no difference in detecting root perforations (p = 0.60 and p = 0.92, respectively). CI was more accurate in detecting root perforation than strip perforation while the ability of PSP in detection of strip perforation was better than CI, though not statistically significant (p = 0.74 and p = 0.58, respectively). MDCT was the most inaccurate imaging modality for diagnosis of both strip and root perforations.
As the diameter of perforation increased, the diagnostic ability of all radiographic techniques increased as well. However, the perforation size did not influence the diagnostic capability of the radiographic techniques except that a 0.2 mm defect was more difficult to detect than a 0.4 mm defect in both strip and root perforations using MDCT (p = 0.03, Table 3). The inter-observer Cohen's kappa coefficients were 0.62, 0.67, 0.85 and 0.56 for CI, PSP, CBCT and MDCT, respectively. Intra-observer agreements were excellent and varied between 0.86 and 0.94.
This study investigated the diagnostic value of film-based periapical radiography, digital PSP periapical radiography, CBCT and MDCT in detection of root perforations in endodontically treated teeth. The influence of size and location of perforation on the accuracy of these radiographic techniques were also assessed. The roots were perforated on the mesial or distal sides because according to the morphology of mandibular molar roots, it is more probable that perforations occur at these sides.14
Periapical radiographs (PRs) including the conventional intraoral and digital intraoral radiographs are the most common imaging modalities in endodontic clinical practice for assessing the progression and outcome of treatment.9,15 Both CI and PSP radiography are used to assess root perforations.16,17 We found that PSP radiography was superior to CI in diagnosis of perforations although the difference was not statistically significant. The ability of radiographs for distinguishing the fine details in an image is related to spatial resolution (SR). The SR of CI (> 20 LP/mm) is higher than that of PSP (6 - 8 LP/mm).Therefore, it should result in better detection of small perforations by CI.16,17 The high sensitivity of PSP radiography in diagnosing perforations could be explained by its enhanced contrast resolution (CR). CR is the ability to distinguish different densities on radiographs.17 Previous studies have shown that higher-SR images do not improve the detection of proximal caries in a PSP system.18 Increasing the CR allows for better capturing the shades of gray that are recorded in an image and ensures that the gray-levels are available for processing when certain signals of known characteristics need to be displayed.19 As a result, subtle changes in root integrity such as root perforation could be diagnosed.
CBCT has the highest accuracy among different imaging modalities in detecting perforations. The difference between the sensitivity of CBCT devices in current and previous studies may be due to the inherent metal artifacts in CBCT, which differ by the type of detector and spatial resolution of different systems.12,20 Some CBCT scanners such as Cranex 3D provide the user with a choice between the high and low resolution modes while scanning a patient. We used high resolution mode since it has a lower voxel size and higher exposure rate resulting in higher spatial resolution for scanning and detecting small root perforations.21 On the other hand, the higher spatial resolution of acquired images renders higher patient radiation dose. Therefore, it was stated that this may provide the same diagnostic result as lower resolution images.22 Haiter-Neto et al. indicated that the resolution did not have an impact on the detection of proximal and occlusal caries.23 There is no report in the literature on the impact of resolution mode on the detection of root perforations in filled roots using CBCT. However, it is generally thought that clinical applications of high resolution mode will depend on the clinical needs and the propriety from the point of radiation doses.22
Metal artifacts related to radiopaque materials inside the canal decrease the accuracy of CBCT in detecting endodontic complications.12,24 According to Hassan et al., streak artifacts associated with root canal filling could mimic fracture and reduce the specificity of CBCT scans in diagnosis.25 The same artifact could increase the risk of perforation misdiagnosis. Bueno et al. suggested that sequential axial slices of 0.2 mm/0.2 mm of each root from coronal to apical (or from apical to coronal) could reduce the beam hardening effect associated with endodontic material by decreasing the amount of filling near the perforation location.26 This procedure provides precious information regarding the location of communication between the root canals and the periodontal space, hence suggesting root perforations. This strategy was used to allow better detection of perforations by CBCT.
CT scans of the jaws are primarily used for the temporomandibular joints and then for the three-dimensional reconstruction of the jaws before major maxillofacial operations, bone evaluation for implant placement, and detection of vertical root fractures.27,28,29,30 The authors did not find any reports on the diagnosis of root perforation with CT in the literature. MDCT had the lowest sensitivity in detecting perforations possibly due to the difference in spatial resolution.31 Spatial resolution of CI, PSP and CBCT were superior to that of MDCT (> 20 LP/mm, 6 - 8 LP/mm, and 3.1 LP/mm versus 2 LP/mm, respectively).16,17,31 However, superimposition of the neighboring structures reduces the sensitivity of PRs while the 3D nature of CBCT and MDCT allows visualization of the peroration in various sections and angulations.23 In our study, a slice thickness of 0.2 mm for CBCT and 0.75 mm for MDCT affected the spatial resolution of the reconstructed axial images of CBCT and MDCT.31,32 Several studies stated that for detailed evaluation of the mandible, it is essential to obtain CT scans with narrow cuts at bone windows, when the diameter of lesion is comparable to or less than the CT slice thickness, identification of the lesions is inaccurate.31,33 As a result, it is difficult to diagnose such small perforations with MDCT.
In our study, the diagnostic value of periapical radiographs in diagnosing strip and root perforations was high mainly because these perforations were made on mesial or distal sides of the roots and radiopaque materials were placed in canals. Although the diameter of perforations were small and similar to the diameter of endodontic instruments, the results obtained in the current study showed that the diameter of perforation did not influence the accuracy of periapical radiographs which is similar to a previous study.7 Changing the horizontal angulation of the radiation source increases the diagnostic ability of PRs especially for diagnosis of strip perforations where the location of perforation could be masked by the concavity of the root (Figures 2 and 3).7,34 Consequently, it was possible to highly diagnose strip and root perforations.
The results of our study showed that CBCT was highly accurate in diagnosis of strip perforations. Venskutonis et al. found that CBCT was more sensitive especially in a small voxel size.35 Presence of radiopaque material in the canal can enhance the accuracy of PRs. It has been proposed that highly radiopaque calcium-hydroxide paste with barium sulfate placed in the root canal can enhance radiographic detection.36 Shemesh et al. found CBCT and PSP radiography to be unreliable techniques for detection of strip perforations.7 Although CBCT was superior to PSP radiography in diagnosing this kind of perforation, there was no difference in detecting root perforations. Eskandarloo et al. found a significant difference between PSP radiography and CBCT in detecting small (0.2 mm) mesiodistal perforations.12 The high accuracy of PRs and CBCT in detecting strip perforations in our study can be to some extent explained by the presence of filling material penetrating into the perforation. Previous studies found warm or soft gutta-percha methods to be more effective than lateral compaction in sealing lateral canals.37 In the current study, it is possible that the packing of gutta-percha caused penetration of the filling material, especially sealer, into the cervical perforations and consequently resulting in better detection of strip perforations.
The results of the current study revealed that perforation diameter in the range of 0.2 - 0.4 mm did not influence the diagnostic accuracy of imaging techniques except that a 0.2 mm defect was more difficult to detect than a 0.4 mm perforation by MDCT. In agreement with the results of our study, Venskutonis et al. showed that perforation size did not influence the accuracy of CBCT.35 However, they stated that CI could not detect 0.2 mm, 0.3 mm and 0.4 mm perforation sizes mainly because they perforated the roots on the buccal or lingual sides of unfilled roots. D'Addazio et al. found no significant difference between CI and CBCT in the detection of large (1 mm) mesiodistal perforations.24 It should be noted that occurrence of such large perforations in the clinical setting is not probable and the result of our study on small perforations could not confirm or reject the findings of D'Addazio et al. As previously discussed, the lower sensitivity of MDCT could be related to higher slice thickness of this modality.24
In the clinical setting, additional factors such as performance of the observer, viewing conditions, patient related factors and software specifications of MDCT and CBCT can affect the diagnosis of root perforations.35 In this study, artificially created root perforations, soft tissue simulation and dry human mandible did not provide the same image quality as in the clinical setting. Well-distinguished features of the artificially created defects, lack of patient movement and inherent difference between the artificial and natural conditions may raise the possibility of measurement bias and overestimation. Furthermore, we simulated root perforation only on root portion of the tooth and assessed the diagnostic ability of the imaging modality in mandibular molars. The results may be different in furcal perforations and in the maxillary molar teeth due to different anatomy. The most important drawback of MDCT is the high radiation dose. CBCT produces less radiation than MDCT but more than PRs. We have to keep ALARA and radiation exposure should be taken into consideration.38,39 Consequently, in diagnostic tasks related to the perforation of root where it is not possible to detect the perforation based only on PRs or clinical examination, use of CBCT is favorable and useful. MDCT is not suggested for diagnosing perforations.
Under the conditions of this in vitro study, the overall accuracy of PRs and CBCT scans to diagnose perforations in root-filled teeth was high although CBCT scans showed a significantly higher accuracy than PRs in diagnosing strip perforations. There was no significant difference between the CBCT and PRs in detecting root perforations. Considering the high radiation dose, MDCT was not suggested as a primary or secondary radiographic technique for detecting perforations. Location and diameter of perforations did not influence the accuracy of the radiographic technique except that 0.2 mm defects were more difficult to detect than 0.4 mm defects by MDCT.
Figures and Tables
Figure 2
Periapical radiography taken with conventional intraoral (CI) imaging technique. (a) Standard angulation; (b) Distal angulation. Arrow shows strip perforation.
Figure 3
Periapical radiography taken with digital photostimulable phosphor (PSP) radiographic imaging technique. (a) Standard angulation; (b) Distal angulation. Arrow shows strip perforation.

Figure 4
Images taken with cone beam computed tomography (CBCT) imaging technique. (a) Root perforation (arrow); (b) Strip perforation (arrow).

Figure 5
Images taken with multidetector computed tomography (MDCT) imaging technique. (a) Root perforation (arrow); (b) Strip perforation (arrow).

Table 1
Overall sensitivity, specificity and accuracy of the imaging techniques in diagnosis of perforations with known simulated perforations as the gold standard

| Imaging technique | Sensitivity(%) | Specificity (%) | Accuracy (%) |
|---|---|---|---|
| CI | 84.38 | 93.75 | 0.74 |
| PSP | 87.50 | 91.67 | 0.76 |
| CBCT | 97.92 | 85.42 | 0.86 |
| MDCT | 77.08 | 87.50 | 0.60 |
Table 2
Specificity, sensitivity, and accuracy of the radiographic techniques in diagnosing perforations at different locations
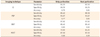
Table 3
Accuracy of imaging modalities in detection numbers of perforations according to the perforation diameter
Acknowledgment
We would like to thank the Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences for approving this study and special thanks to Dr. A. Kavand of the University of Tehran for the English language editing.
References
1. Fuss Z, Trope M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol. 1996; 12:255–264.

2. Ingle JI. A standardized endodontic technique utilizing newly designed instruments and filling materials. Oral Surg Oral Med Oral Pathol. 1961; 14:83–91.

3. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics. 2006; 13:95–107.

4. Alhadainy HA. Root perforations. A review of literature. Oral Surg Oral Med Oral Pathol. 1994; 78:368–374.
5. Bryant ST, Dummer PM, Pitoni C, Bourba M, Moghal S. Shaping ability of .04 and .06 taper ProFile rotary nickel-titanium instruments in stimulated root canals. Int Endod J. 1999; 32:155–164.

6. Berutti E, Fedon G. Thickness of cementum/dentin in mesial roots of mandibular first molars. J Endod. 1992; 18:545–548.

7. Shemesh H, Cristescu RC, Wesselink PR, Wu MK. The use of cone-beam computed tomography and digital periapical radiographs to diagnose root perforations. J Endod. 2011; 37:513–516.

8. Ball RL, Barbizam JV, Cohenca N. Intraoperative endodontic applications of cone-beam computed tomography. J Endod. 2013; 39:548–557.

9. Patel S, Dawood A, Mannocci F, Wilson R, Pitt Ford T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J. 2009; 42:507–515.

10. Chindasombatjaroen J, Kakimoto N, Murakami S, Maeda Y, Furukawa S. Quantitative analysis of metallic artifacts caused by dental metals: comparison of cone-beam and multi-detector row CT scanners. Oral Radiol. 2011; 27:114–120.

11. Gaia BF, Sales MA, Perrella A, Fenyo-Pereira M, Cavalcanti MG. Comparison between cone-beam and multislice computed tomography for identification of simulated bone lesions. Braz Oral Res. 2011; 25:362–368.

12. Eskandarloo A, Mirshekari A, Poorolajal J, Mohammadi Z, Shokri A. Comparison of cone-beam computed tomography with intraoral photostimulable phosphor imaging plate for diagnosis of endodontic complications: a simulation study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:e54–e61.

13. Fuss Z, Assooline LS, Kaufman AY. Determination of location of root perforations by electronic apex locators. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 82:324–329.

14. Skidmore AE, Bjorndal AM. Root canal morphology of the human mandibular first molar. Oral Surg Oral Med Oral Pathol. 1971; 32:778–784.

15. Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: I. 1961. J Endod. 2003; 29:702–706.

16. Farman AG, Farman TT. A comparison of 18 different x-ray detectors currently used in dentistry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 99:485–489.

17. Udupa H, Mah P, Dove SB, McDavid WD. Evaluation of image quality parameters of representative intraoral digital radiographic systems. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:774–783.

18. Li G, Berkhout WE, Sanderink GC, Martins M, van der Stelt PF. Detection of in vitro proximal caries in storage phosphor plate radiographs scanned with different resolutions. Dentomaxillofac Radiol. 2008; 37:325–329.

20. Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e25–e31.

21. Cheng JG, Zhang ZL, Wang XY, Zhang ZY, Ma XC, Li G. Detection accuracy of proximal caries by phosphor plate and cone-beam computerized tomography images scanned with different resolutions. Clin Oral Investig. 2012; 16:1015–1021.

22. Spin-Neto R, Gotfredsen E, Wenzel A. Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: a systematic review. J Digit Imaging. 2013; 26:813–820.

23. Haiter-Neto F, Wenzel A, Gotfredsen E. Diagnostic accuracy of cone beam computed tomography scans compared with intraoral image modalities for detection of caries lesions. Dentomaxillofac Radiol. 2008; 37:18–22.

24. D'Addazio PS, Campos CN, Özcan M, Teixeira HG, Passoni RM, Carvalho AC. A comparative study between cone beam computed tomography and periapical radiographs in diagnosis of simulated endodontic complications. Int Endod J. 2011; 44:218–224.
25. Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod. 2009; 35:719–722.

26. Bueno MR, Estrela C, De Figueiredo JA, Azevedo BC. Map-reading strategy to diagnose root perforations near metallic intracanal posts by using cone beam computed tomography. J Endod. 2011; 37:85–90.

27. Wilkinson T, Maryniuk G. The correlation between sagittal anatomic sections and computerized tomography of the TMJ. J Craniomandibular Pract. 1983; 1:37–45.

28. Solar P, Ulm C, Lill W, Imhof H, Watzek G, Blahout R, Gruber H, Matejka M. Precision of three-dimensional CT-assisted model production in the maxillofacial area. Eur Radiol. 1992; 2:473–477.

29. Casselman JW, Quirynen M, Lemahieu SF, Baert AL, Bonte J. Computed tomography in the determination of anatomical landmarks in the perspective of endosseous oral implant installation. J Head Neck Pathol. 1988; 7:255–264.
30. Youssefzadeh S, Gahleitner A, Dorffner R, Bernhart T, Kainberger FM. Dental Vertical Root Fractures: Value of CT in Detection. Radiology. 1999; 210:545–549.

31. Iikubo M, Kobayashi K, Mishima A, Shimoda S, Daimaruya T, Igarashi C, Imanaka M, Yuasa M, Sakamoto M, Sasano T. Accuracy of intraoral radiography, multidetector helical CT, and limited cone-beam CT for the detection of horizontal tooth root fracture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:e70–e74.

32. Baxter BS, Sorenson JA. Factors affecting the measurement of size and CT number in computed tomography. Invest Radiol. 1981; 16:337–341.

33. Shaha AR. Preoperative evaluation of the mandible in patients with carcinoma of the floor of mouth. Head Neck. 1991; 13:398–402.

34. Fava LR, Dummer PM. Periapical radiographic techniques during endodontic diagnosis and treatment. Int Endod J. 1997; 30:250–261.

35. Venskutonis T, Juodzbalys G, Nackaerts O, Mickevicienė L. Influence of voxel size on the diagnostic ability of cone-beam computed tomography to evaluate simulated root perforations. Oral Radiol. 2013; 29:151–159.

36. Hovland EJ, Dumsha TC. Problems in the management of tooth resorption. Problem solving in endodontics. 3rd ed.St. Louis: CV Mosby;1997. p. 253–276.
37. Carvalho-Sousa B, Almeida-Gomes F, Carvalho PR, Maníglia-Ferreira C, Gurgel-Filho ED, Albuquerque DS. Filling lateral canals: evaluation of different filling techniques. Eur J Dent. 2010; 4:251–256.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download