Abstract
Tooth related factors such as palatoradicular groove can be one of the causes for localized periodontal destruction. Such pathological process may result in apicomarginal defect along with inflammation of pulp. This creates challenging situation which clinician must be capable of performing advanced periodontal regenerative procedures for the successful management. This case report discusses clinical management of apicomarginal defect associated with extensive periradicular destruction in a maxillary lateral incisor, along with histopathologic aspect of the lesion.
A close relationship exists between periodontal tissues and pulpal tissue. Periodontitis is an inflammatory condition of periodontium caused primarily due to bacterial biofilm and host response.1 Among the various factors, local factors such as developmental anomalies of tooth may predispose to enhancement of bacterial adhesion to tooth surface. This offers favorable niche for allowing subgingival growth of bacterial plaque.23 Palatoradicular or cinguloradicular groove (PRG) are common development anomalies encountered by clinician. However, it has not been frequently reported in the literature, yet. PRG is a potential area of plaque accumulation that provides straightforward pathway to deeper structure of periodontium.2 This results in localized periodontal attachment loss, causing localized pocket along the extension of groove.23 Although exact etiology is not understood, infolding of enamel organ and hertwig's epithelial root sheath, incomplete attempt of tooth to form another root, or genetic alteration were suggested as possible mechanism for occurrence of the groove, similar to that of dens invaginatus.3456 PRG occurs commonly on distolingual aspect with the prevalence of 2.6% to 8.5% in maxillary incisors.6 Studies related to PRG extension over radicular surface concluded that only 10% extend more than 10 mm over the root surface.6 Depth of PRG and its extent along the root surface may have deleterious effect on the health of periodontium as well as pulpal tissue.7
Along the length of PRG, a direct communication between pulp and periodontal ligament has been described in the literature, which is a rare occurance.8 Depending on the extent of PRG, localized bony defect may extend along the entire root length to involve peri-radicular area with/without loss of marginal bone, which are described as apicomarginal defect.9 Association of apicomarginal defect along with PRG affects the treatment outcome and also plays a key role in selection of treatment modality.9 Apicomarginal defect represents significant challenge for treatment as post-therapy long junctional epithelium formation occurs over the dehisced root surface.10 The present case report describes the management of apicomarginal defect associated with maxillary right lateral incisor caused as a result of PRG that extended to the apex.
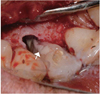
A 21 year systemically healthy nonsmoker male reported to Department of Periodontology, Sinhgad Dental College and Hospital who complained of bleeding gums, mild pain, and purulent discharge in relation to upper right front tooth region for 6 months. On intraoral examination, attached gingiva on the labial aspect of maxillary right lateral incisor showed the presence of draining sinus tract and grade I mobility (Figure 1). Patient reported no history of trauma to the tooth. Periodontal status of dentition was stable and clinically healthy, but tooth 12 presented localized deep probing depth of 15 mm along the distolingual aspect associated with PRG (Figure 2). Tooth was non-vital as it demonstrated no response to electric pulp test (Kerr Electric Pulp Tester, SybronEndo, Orange, CA, USA) as well as to cold test. Intraoral periapical radiograph (IOPA) of involved tooth showed presence of indentation in the distocervical region of crown with linear radiolucency running parallel to the root canal over the entire length of the root (Figure 3). Absence of periodontal ligament space and discontinuous lamina dura was evident on radiograph. There was an ill-defined radiolucency surrounding the middle and apical 1/3 of the root. Root appeared to be a dilacerated with angular bone loss along the distal aspect, extending till middle third of the root (Figure 3).
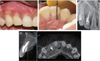
According to clinico-radiographic features and criteria's by Abbott and Sulgado, a diagnosis of concurrent endodontic and periodontal disease was made.11 Patient was explained about the treatment plan and required investigations (radiographic and histological), for which he consented. Authorization from the institutional ethical board was also obtained (SDCH/IEC/2012-13/43A). The patient was subjected to cone beam computed tomography (CBCT, CS 9300, Kodak-Carestream, Rochester, NY, USA) evaluation, which revealed the presence of localized periapical bone loss (10.61 mm × 11.09 mm) with loss of facial cortical plate and marginal alveolar bone along the labial and distolingual aspects of tooth 12 (Figure 4). Tooth also showed the presence of nonembeded pulp stone (green arrow, Figure 4). Based on CBCT findings, a diagnosis of apicomarginal bone defect was made. Estrela et al., proposed the new periapical index (CBCTPAI, cone beam computed tomography periapical apical index) based on diameter of periapical radiolucency and expansion/destruction of periapical cortical bone as seen on the CBCT images.12 Thus the bony defect associated with the tooth 12 was scored as 5+D (Figure 4).
According to the treatment protocols of Abbott and Salgado and Oh et al., endodontic therapy with phase I periodontal therapy was initiated.1113 Under rubber dam isolation, access opening was done and canal were cleaned and shaped using crown down technique up to apical size 60 (Colorinox K-file, Dentsply Maillefer, Ballaigues, Switzerland) with 5.25% sodium hypochlorite as irrigant. After thoroughly drying of canals, calcium hydroxide paste was applied and the access cavity was sealed with zinc oxide eugenol restoration. Root planning and curettage was done followed by provisional composite and wire splinting of tooth. Instructions for oral hygiene maintenance were given. After four weeks, intra-canal medication was replaced with new calcium hydroxide medication and periodontal reassessment was done. During this assessment it was found that gingival tissue with respect to the maxillary lateral incisor appeared clinically healthy with no draining sinus tract with persistence of pocket. Patient was recalled after three months for further evaluation, which revealed persistent localized pocket of 14 mm. Hence, surgical periodontal therapy was planned.
The surgical therapy involved guided tissue regeneration using demineralized freeze dried bone allograft (DFDBA, Tissue bank, TATA Memorial Hospital, Mumbai, India) and platelet rich fibrin (PRF). One week prior to surgical therapy root canal were filled with cold lateral compaction of 0.02 taper master gutta-percha cone and accessory cones with AH Plus sealer (Dentsply Maillefer) and warm vertical compaction of 0.06 taper gutta-percha cone using Obtura II (SybronEndo). The access cavity was sealed with glass ionomer cement (Fuji II, GC Co., Tokyo, Japan).
Prior to surgery, PRF was freshly prepared. Ten mL of whole blood was drawn by venipuncture from antecubital area in two 5 mL sterile glass tubes and was centrifuged at 3,000 rpm for 10 minutes. This resulted in three layers of lower red fraction containing red blood cells, upper straw colored cellular plasma, and the middle fraction containing the fibrin clot. PRF was obtained from the upper straw colored layer with middle layer. By using 2% lidocaine hydrochloride with 1:100,000 adrenaline, adequate local anesthesia was obtained which was followed by intracrevicular horizontal incision extending from mesial line angle of tooth 11 to distal line angle of tooth 13 on both buccal and palatal aspect (Figure 5). On buccal aspect vertical releasing incisions were placed at the end of horizontal incision extending beyond mucogingival junction and full thickness mucoperiosteal flap was adequately reflected to expose the bony defect for the access (Figure 5). After complete degranulation of bony defect, radicular groove could be visualized extending along distolingual aspect of the entire root length. Tissue removed from periapical region was sent for histopathological examination after fixation in 10% formalin. Bony defect was seen around the radicular groove on the palatal aspect that extended buccally involving apical and middle third of the root of right lateral incisor with loss of buccal cortical plate along the entire root surface. Intact interdental bone was evident (Figure 6). Dilaceration of apical third of root was noticed with extrusion of approximately 1 mm of gutta-percha from the apex (yellow arrow, Figure 6).
Thorough scaling of root surface was done with ultrasonic instruments (Piezon 250, EMS, Nyon, Switzerland). Saucerization of the PRG was done using appropriate mechanical instruments (Gracey curette, numbers 1,2 and 5,6, Hu-Friedy Manufacturing Co., Chicago, IL, USA) to obtain hard and smooth surface. Apical 3 mm of the root was resected and retropreparation was performed using ultrasonic tips (Diamond Coated Ultrasonic tips, SybronEndo). The root end cavity was filled with mineral trioxide aggregate (ProRoot MTA, Dentsply, York, PA, USA) (Figure 7). With adequate hemostasis and isolation, PRG was conditioned with 10% polyacrilic acid and sealed with light cured glass ionomer cement (Fuji II LC, GC Co.) (Figure 8). Bony defect was overfilled up to the level of interdental bone crest with mixture of DFDBA and PRF (Figure 9). PRF was then used to cover the grafted area in the form of membrane (Figure 10). Flaps were repositioned to achieve primary closure using 4-0 monofilament polyamide black suture (Ethilon, Johnson & Johnson, M.I.D.C., Aurangabad, India) (Figure 11). Postoperative IOPA was made and antibiotics (Amoxicillin 500 mg, 3 times daily) and non-steroidal anti-inflammatory drug (Ibuprofen 500 mg, 3 times daily) were prescribed for 5 days. Patient was advised regarding oral hygiene measures with the use of 0.2% chlorhexidine gluconate mouthwash for 3 weeks. Healing was uneventful and sutures removed after 10 days.
Patient was recalled at 3, 6, 9 and 12 month for evaluation. At 12 month follow up, patient was asymptomatic, sinus tract was closed and probing depth was 2 mm with 1 mm gingival recession along the distopalatal aspect (Figures 12a and 12b). IOPA and CBCT made at 12 month recall showed complete resolution of the periapical radiolucency (Figures 12c and 12d). According to radiographic healing criteria developed by Rud et al., IOPA at 12 month was assessed and found to show complete healing (Figure 12c).14
Hematoxylin and eosin stained section of the granulation tissue showed non-keratinized stratified squamous cystic epithelium lining with arcading type (blue arrow) of proliferation and connective tissue showed infiltration of chronic inflammatory cells, which were the suggestive features of periapical cyst (Figure 13).
Case presented here is of a young patient with extensive apicomarginal bony defect caused due to PRG involving entire root of maxillary right lateral incisor. Improvement of patient oral health was achieved by treatment objectives, including elimination of endodontic infection, removal of PRG to prevent accumulation and pathway for bacterial plaque and regeneration of lost periodontal structures.
According to Kogon, PRG affects about 5.6% of lateral incisors with only 10% extends to more than 10 mm from cingulum towards apex.6 In the present case, PRG extended to the apex, which is a rare finding, and it resulted in concurrent endodontic and periodontal disease with apicomarginal bony defect. Schultz et al. and Sekhar et al. have advocated splinting of mobile teeth before any regenerative procedure to improve periodontal attachment level.1516 In the present case, tooth was also associated with grade I mobility hence temporary splinting was done to aid in reduction of tooth mobility similar to the case reports of Oh et al. and Ballal et al. who showed successful outcome.1317 But removal of splint depends on individual situation.1322 In our case splint was removed at 9 month follow up visit and we observed absence of mobility.
Limited cases are published with respect to maxillary incisor associated along with periapical lesion and concomitant marginal loss.1318 The prognosis of periaradicular surgery (varying between 25% and 90%) depends on the amount and location of bone adjacent to root surfaces.1920 Destruction of marginal bone found in apicomarginal defect reduces the success of treatment to 27% and 37%.21 Loss of buccal cortical bone along with periapical bone as seen in this case created significant challenge for successful treatment outcome.
Literature reports numerous biomaterials for guided tissue regeneration which includes, resorbable/non-resorable membranes, periosteal grafts, various bone grafts.37101518222324 All of these have shown successful results, but certain disadvantages of the membranes, such as high cost, possibility of contamination on exposure to oral cavity, need for second surgery (non-resorable membranes only) and greater risk of mechanical trauma from gingival sulcus (during loss of marginal bone) should be overcome.26 Hence in present case mixture of PRF and DFDBA graft was used. PRF was also used as membrane to cover the grafted site. Shivshankar et al. reported the use of PRF with hydroxyapatite for management of large periapical lesion and its successful treatment outcome after 2 years.24 PRF contains various growth factors which has potent positive effects on cellular differentiation.24,25 PRF membrane also acts like a competition barrier, and accelerates wound closure and mucosal healing due to fibrin bandage and growth factor release.26
Glass ionomer cement (GIC) is biocompatible and has adhesive property to dentin.27 Clinical reports demonstrate that behavior of GIC in subgingival area is characterized by less inflammation, greater bone repair, gain of clinical attachment and reduced pocket depth.27 GIC used in the present case showed similar results with Forero-López et al., who reported the new technique sensitive procedure which involved sealing PRG with GIC, replantation with intentional horizontal 180 degree rotation of tooth and aesthetic veneer for restoring tooth morphology.28 But Naik et al. and Zucchelli et al. have used biodentine and flowable composite, respectively.2930 Zucchelli et al. also have demonstrated successful results by using papilla amplification flap and Emdogain (Institut Straumann, Waldenburg, Switzerland) which is unique of this case.30
Various reports published in the literature have used IOPA to evaluate bony changes associated with the involved tooth except Rachana et al. who have used CT, while Rajput et al. have used CBCT for initial evaluation.3132 But in the present case along with IOPA, CBCT have been used not only for initial evaluation but also for postoperative follow up. Scoring of lesion using CBCTPAI was done, which is unique of this report. To best of our knowledge this report is first to report use of CBCT and CBCTPAI for evaluation of treatment outcomes. At 12th month radiographic assessment criteria was used to access pre- and post-operative IOPA that satisfied the criteria of complete healing. To our knowledge our case report is also unique in presenting histological aspect of obtained periapical lesion to confirm the lesion.
The present report has described successful management of apicomarginal defect by applying principles of GTR with use of DFDBA and PRF. With the help of CBCT along with clinical findings, satisfactory results were demonstrated but further long-term follow up is required to validate obtained results.
Figures and Tables
 | Figure 1Labial view with draining sinus tract (yellow arrow) associated with maxillary right lateral incisor. |
 | Figure 4Preoperative cone beam computed tomography images. Green arrow indicates nonembeded pulp stone. |
 | Figure 6After complete removal of granulation tissue. Yellow arrow indicates extrusion of approximately 1 mm of gutta-percha from the apex. |
 | Figure 8Glass ionomer cement restoration in the palatoradicular groove. White arrow indicates glass ionomer restoration. |
 | Figure 9Bone defect filled with mixture of demineralized freeze-dried bone allograft and platelet rich fibrin. |
Acknowledgement
We would like to thank staff of Department of Oral Pathology, Sinhgad Dental College and Hospital, Maharashtra, India, for helping us in histopathological investigation.
References
1. Darby I, Curtis M. Microbiology of periodontal disease in children and young adults. Periodontol 2000. 2001; 26:33–53.

2. Kovács V, Tihanyi D, Gera I. The incidence of local plaque retentive factors in chronic periodontitis. Fogorv Sz. 2007; 100:295–300.
3. Simon JH, Glick DH, Frank AL. Predictable endodontic and periodontic failures as a result of radicular anomalies. Oral Surg Oral Med Oral Pathol. 1971; 31:823–826.

4. Ennes JP, Lara VS. Comparative morphological analysis of the root developmental groove with the palato-gingival groove. Oral Dis. 2004; 10:378–382.

5. Peikoff MD, Perry JB, Chapnick LA. Endodontic failure attributable to a complex radicular lingual groove. J Endod. 1985; 11:573–577.

6. Kogon SL. The prevalence, location and conformation of palato-radicular grooves in maxillary incisors. J Periodontol. 1986; 57:231–234.

7. Assaf ME, Roller N. The cingulo-radicular groove: its significance and management-two cases reports. Compendium. 1992; 13:94. 96. 98 passim.
8. Lara VS, Consolaro A, Bruce RS. Macroscopic and Microscopic analysis of the palato-gingival groove. J Endod. 2000; 26:345–350.

9. Dietrich T, Zunker P, Dietrich D, Bernimoulin JP. Apicomarginal defects in periradicular surgery: classification and diagnostic aspects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:233–239.

10. Goyal B, Tewari S, Duhan J, Sehgal PK. Comparative evaluation of platelet-rich plasma and guided tissue regeneration membrane in the healing of apicomarginal defects: a clinical study. J Endod. 2011; 37:773–780.

11. Abbott PV, Salgado JC. Strategies for the endodontic management of concurrent endodontic and periodontal diseases. Aust Dent J. 2009; 54:S70–S85.

12. Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod. 2008; 34:1325–1331.

13. Oh SL, Fouad AF, Park SH. Treatment strategy for guided tissue regeneration in combined endodontic-periodontal lesions: case report and review. J Endod. 2009; 35:1331–1336.

14. Rud J, Andreasen JO, Jensen JE. Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg. 1972; 1:195–214.

15. Schulz A, Hilgers RD, Niedermeier W. The effect of splinting of teeth in combination with reconstructive periodontal surgery in humans. Clin Oral Investig. 2000; 4:98–105.

16. Sekhar LC, Koganti VP, Shankar BR, Gopinath A. A comparative study of temporary splints: bonded polyethylene fiber reinforcement ribbon and stainless steel wire + composite resin splint in the treatment of chronic periodontitis. J Contemp Dent Pract. 2011; 12:343–349.

17. Ballal NV, Jothi V, Bhat KS, Bhat KM. Salvaging a tooth with a deep palatogingival groove: an endo-perio treatment - a case report. Int Endod J. 2007; 40:808–817.

18. Kishan KV, Hegde V, Ponnappa KC, Girish TN, Ponappa MC. Management of palato-radicular groove in a maxillary lateral incisor. J Nat Sci Biol Med. 2014; 5:178–181.
19. Skoglund A, Persson G. A follow-up study of apicoectomized teeth with total loss of the buccal bone plate. Oral Surg Oral Med Oral Pathol. 1985; 59:78–81.

20. Abramowitz PN, Rankow H, Trope M. Multidisciplinary approach to apical surgery in conjunction with the loss of buccal cortical plate. Oral Surg Oral Med Oral Pathol. 1994; 77:502–506.

21. Gutmann JL, Harrison JW. Surgical Endodontics. 1st ed. Chennai: All India Publishers and Distributors;1999. p. 338.
22. Taschieri S, Rosano G, Weinstein T, Bortolin M, Del Fabbro M. Treatment of through-and-through bone lesion using autologous growth factors and xenogeneic bone graft: a case report. Oral Maxillofac Surg. 2012; 16:57–64.

23. Attam K, Tiwary R, Talwar S, Lamba AK. Palatogingival groove: endodontic-periodontal management-case report. J Endod. 2010; 36:1717–1720.

24. Shivashankar VY, Johns DA, Vidyanath S, Sam G. Combination of platelet rich fibrin, hydroxyapatite and PRF membrane in the management of large inflammatory periapical lesion. J Conserv Dent. 2013; 16:261–264.

25. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Anthony J, Dohan J, Mouhyi J, Dohan DM. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV. clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:e56–e60.

26. Pecora G, Baek SH, Rethnam S, Kim S. Barrier membrane techniques in endodontic microsurgery. Dent Clin North Am. 1997; 41:585–602.
27. Gomes SC, Miranda LA, Soares I, Oppermann RV. Clinical and Histologic Evaluation of the Periodontal Response to Restorative Procedures in the Dog. Int J Periodontics Restorative Dent. 2005; 25:39–47.
28. Forero-López J, Gamboa-Martínez L, Pico-Porras L, Niño-Barrera JL. Surgical management with intentional replantation on a tooth with palato-radicular groove. Restor Dent Endod. 2015; 40:166–171.

29. Naik M, de Ataide Ide N, Fernandes M, Lambor R. Treatment of combined endodontic: periodontic lesion by sealing of palato-radicular groove using biodentine. J Conserv Dent. 2014; 17:594–597.

30. Zucchelli G, Mele M, Checchi L. The papilla amplification flap for the treatment of a localized periodontal defect associated with a palatal groove. J Periodontol. 2006; 77:1788–1796.





 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download