Abstract
Objectives
To determine and compare the fracture resistance of endodontically treated maxillary central incisors restored with different posts and cores.
Materials and Methods
Forty-eight upper central incisors were randomly divided into four groups: cast post and core (group 1), fiber-reinforced composite (FRC) post and composite core (group 2), composite post and core (group 3), and controls (group 4). Mesio-distal and bucco-lingual dimensions at 7 and 14 mm from the apex were compared to ensure standardization among the groups. Twelve teeth were prepared for crown restoration (group 4). Teeth in other groups were endodontically treated, decoronated at 14 mm from the apex, and prepared for posts and cores. Resin-based materials were used for cementation in groups 1 and 2. In group 3, composite was used directly to fill the post space and for core build-up. All samples were restored by standard metal crowns using glass ionomer cement, mounted at 135° vertical angle, subjected to thermomechanical aging, and then fractured using a universal testing machine. Kruskal-Wallis and Mann-Whitney U tests were used to analyze the data.
Results
Fracture resistance of the groups was as follows: Control (group 4) > cast post and core (group 1) > fiber post and composite core (group 2) > composite post and core (group 3). All samples in groups 2 and 3 fractured in restorable patterns, whereas most (58%) in group 1 were non-restorable.
Endodontically treated teeth (ETT) are potentially weaker than vital teeth against chewing forces and may fracture more easily.1 For many years, post and core systems have been used as foundational materials for the final restoration of ETT that have lost most of their coronal tooth structure.2 Posts and cores can be custom-made or prefabricated.34
A successful post and core restoration requires a material with physical properties similar to that of tooth dentin.5 Duret et al. introduced fiber-reinforced composites (FRCs) more than 20 years ago.67 FRCs, particularly glass-fiber-reinforced posts, have been recommended as an alternative to cast or prefabricated metal posts because of recent advances in adhesive technologies.89 Their current popularity in restorative dentistry is associated with their rigidity and modulus of elasticity, which is similar to those of dentin, in addition to their superior esthetic properties, lower dentinal removal and ability to be bonded to dentin with adhesive luting resins.10 In addition, FRC posts do not result in metal corrosion or allergic reactions, and can be easily removed from root canals in cases of endodontic failure.1112
Many authors have studied different fiber-reinforced post materials, luting agents, post designs and ferrule effects to evaluate their fracture resistance.13141516 However, conflicting results have been reported. Although some studies have reported lower fracture resistance in ETT with FRC posts, others reported that fracture resistance was equal to or greater than that of ETT restored with metal posts.1718 Some authors have found that ETT with minimal structural loss do not necessarily require posts. It is also unclear whether FRC posts strengthen ETT during clinical service.1920
Some clinical studies have confirmed the long-term clinical performance of FRC posts with composite buildup over an observation period of more than 5 years.21 Only 3 - 10% of all tooth build-up failures were post and core failures from root fractures.22 An intra-radicular restorative system with a modulus of elasticity similar to that of dentin is recommended.23 A post that has been bonded to the dentin may reduce stresses in the remaining root and distribute masticatory loads more homogeneously over the entire bonded interface.24 The use of FRC posts has been suggested to reduce stress concentration and to prevent root fractures.25 Thus, the aim of this in vitro study was to compare fracture resistance in maxillary central incisors restored with different posts and cores.
Prior to conducting the study, the research protocol was approved by the Institutional Ethics Committee (Ref. No. 2447). Forty-eight human maxillary central incisors that had been extracted for periodontal reasons were stored in 0.5% chloramine in water at 4℃ and used within 6 months after extraction. Teeth were collected weekly and transferred from chloramine into distilled water. Each tooth was observed under a stereomicroscope at 20× magnification to verify the absence of carious lesions, cracks and micro-fractures. To standardize the experimental procedures, the mesio-distal and bucco-lingual widths at 7 and 14 mm from the apex were measured using a digital calliper (Guilin Guanglu Measuring Instrument Co., Guangxi Zhuang, China). The teeth were randomly divided into four groups. ANOVA showed no significant difference in mesiodistal widths at 7 and 14 mm between the four groups (Table 1).26 Specimens were stored in distilled water at 37℃ and kept moist during the experiment.
Clinical crowns of 36 teeth were cut at 14 mm from the apex using a low-speed saw (TC-3000, Vafaei Industrial Co., Tehran, Iran). Twelve teeth served as the control group, and to standardize their coronal dimensions, they were prepared using diamond burs (Expert Set #4573.314, Komet Brasseler, Lemgo, Germany) for metal crowns (Nickel-Chrome, Damcast NP, Damcast Dentalloy Co., Zhengzhou, China). Similar crown dimensions were used to fabricate crowns for the rest of the experimental samples. The other 36 teeth were divided into three groups. Root canal treatment was performed following a standardized crown-down technique using Protaper Universal (apical, size 30) (Dentsply Maillefer, Ballaigues, Switzerland). After every instrumentation, 2.5% sodium hypochlorite solution was used for irrigation. A final irrigation with 17% EDTA (ACT Aria Dent, Asia Chemi Teb Mfg. Co., Tehran, Iran) was performed to remove the smear layer. The root canals were dried with absorbent paper points (Spident Co. Ltd., Incheon, Korea) and filled with gutta-percha (DiaDent Group International, Cheongju, Korea) via a lateral condensation technique using eugenol-free root canal sealing material (AH 26, Dentsply DeTrey, Konstanz, Germany).
Gutta-percha was removed using a heated hand plugger. The post spaces were prepared using a size 1 drill from the FRC post system (Exacto No. 1, Angelus, Londrina, PR, Brazil), in accordance with the manufacturer's instructions. All roots were uniformly prepared at a depth of 9 mm from the flat coronal surface, to leave at least 5 mm of gutta-percha apically. Samples were weighed to confirm standardization across the groups (Table 1).
A standard post and core were made using fiber-reinforced Exacto No. 1 (Angelus) with a length of 9 mm and 6 mm of composite core build-up (Clearfil Photocore, Kuraray Noritake Dental Inc., Kurashiki, Okayama, Japan). A vinyl plate (0.21 mm, FGM, Joinville, SC, Brazil) was heated and closely adapted to this reference post and core. It was then divided into two parts, i.e., post and core, and used to duplicate cast posts and cores (Damcast NP, Damcast Dentalloy Co.), and composite core build-up with Clearfil Photocore (Kuraray Noritake Dental Inc.) in groups 2 and 3. For fabrication of similar cast post and cores, DuraLay inlay pattern resin (Reliance Dental Mfg. Co., Worth, IL, USA) was injected into the two separated parts of vinyl plate, and then the two parts were attached to each other to form a single pattern resin post and core. Then, the post and core were invested and cast in nickel-chromium alloy (Damcast NP). The procedure was repeated to produce twelve similar cast post and cores.
To build up similar cores in group 2 and 3, the core part of the vinyl plate was filled with hybrid composite (Clearfil Photocore) and placed over the samples, then light cured (Lite Q, Monitex Industrial Co. Ltd, San-Chung, Taiwan) for 40 seconds.
Resin cement (Panavia F2.0, Kuraray Noritake Dental Inc.) was used for posts and cores in group 1, in accordance with the manufacturer's instructions. In group 2, prior to cementation, posts were coated with silane (Silano, Angelus) using a disposable applicator, left for 1 minute, then gently air-dried. They were then cemented using Panavia F2.0 (Kuraray Noritake Dental Inc.). In group 3, teeth were etched with 37% phosphoric acid (Morca Etch, Morvanbon Trading Co., Tehran, Iran) for 15 seconds, then dried with absorbent paper points (Spident Co. Ltd.). Dentin was conditioned with Ambar dentin bonding (Ambar, FGM) in accordance with the manufacturer's instructions. Clearfil Photocore (Kuraray Noritake Dental Inc.) was condensed into the post space in 2 mm increments, followed by core build-up using a reference core in accordance with the manufacturer's instructions.
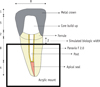
Specimens were prepared for the crown using diamond burs (Expert set #4573, Komet-Brasseler, Lemgo, Germany) in a high-speed handpiece. For ferrule effect, 2 mm of sound dentin was included in the crown preparation and, using a silicon stent, central incisor crowns of identical dimensions were carved with wax, the margins were adjusted, and they were cast in a non-precious alloy (Damcast NP, Figure 1). Glass ionomer cement (GC Gold Label 1, GC Co., Tokyo, Japan) was used to cement all crowns. During all the procedures, teeth were held by moist gauze to prevent dehydration.
Teeth were placed in cylindrical auto-polymerising acrylic (Acropars, Marlic Co., Tehran, Iran) at a 135° vertical angle. To simulate biological width, the margin 2 mm apical to the crown was not covered with acrylic (Figure 1). A specialized mold designed for use with a chewing simulator (CS-4.2, SD Mechatronik GmbH, Feldkirchen-Westerham, Germany) was utilized to mount the specimens. All samples were subjected to 250,000 cycles of 5 kg of force (CS-4.2, SD Mechatronik GmbH). Samples were also subjected to 500 thermal cycles (Delta Tpo2, Nemo, Mashhad, Iran) alternating between 5℃ and 55℃, with a dwell time of 60 seconds.
After thermo-mechanical aging, samples were subjected to a compressive load in a universal testing machine (K - 21046, Walter+bai, Löhningen, Switzerland) at a crosshead speed of 1 mm/min. Load at failure was recorded. Kruskal-Wallis and Mann-Whitney U tests with a significance threshold of p < 0.05 were used to analyze the differences between groups via IBM SPSS 20.0 (IBM, Chicago, IL, USA). Failure modes were classified as restorable or non-restorable; teeth with a fracture line extending above the simulated bone level were considered restorable in this study.
In the process of mechanical fatigue, two samples in group 2 and three samples in group 3 failed before the completion of cyclic loading. These samples were replaced with new samples following the same experimental methodology previously described. The mean loads at fracture of the four groups are presented in Table 2. All of the groups differed significantly from each other. The ranking of the groups was as follows: Control (group 4) > cast post and core (group 1) > fiber post and composite core (group 2) > composite post and core (group 3). Visual inspection (×2.5 binocular loupe, Orascoptic, Kerr Co., Middleton, WI, USA) showed that all samples in the control group fractured in non-restorable patterns. All samples in groups 2 and 3 failed in restorable patterns. Seven samples in group 1 (58%) were non-restorable. Pearson Chi-Square test showed significant difference in fracture pattern among groups (p < 0.001, Table 2).
The present study investigated the restoration of structurally compromised endodontically treated upper central incisors using different posts and cores. The teeth in the control group were most resistant to fractures, followed by those restored with cast posts and cores. All of the fractures in the control group were non-restorable. Seven samples in the cast post and core group (58%) were non-restorable, whereas others had restorable fracture patterns. Teeth with a fracture line extending above the simulated bone level were considered restorable in this study. All samples in the FRC group and the composite group fractured in restorable patterns.
Ferrario et al. assessed the bite force of individual teeth in 52 healthy young adult males and females.27 The incisors exhibited the lowest bite force values in both sexes (93 - 146 N). Although all groups in this study exhibited similar or higher fracture resistance than the mean bite force of the central incisors, it should be noted that two samples in group 2 and three samples in group 3 failed during mechanical loading under 50 N load. Significant differences were observed among all pairs of groups in this study, and the composite group showed the lowest resistance to fracture. Given esthetic considerations, FRCs seem to be favorable choice in such cases. A modulus of elasticity similar to that of dentin and restorable modes of fracture are other advantages of restoration of ETT with FRCs.
Numerous studies have investigated different post and core systems to identify a superior material for use in such situations; however, the results of these studies are not consistent. Bolay et al. compared two FRC posts and cores, and the corresponding composite cores built up without a post.28 There were no significant differences among the four groups. For this reason, Bolay et al. suggested that composites alone can perform as well as FRCs.28 Other studies evaluated the restoration of flared canals, either with custom-cast base metal (Ni-Cr) or different types of FRCs, and concluded that tooth strength was higher when restored with cast posts than any type of fiber-reinforced resin post. However, all of the fiber-reinforced resin posts showed similar behaviour with regard to protecting the remaining tooth structure.29 FRC has yielded similar results to gold alloy posts and cores.30 Other studies have shown higher values with FRC than with zirconia and titanium posts.3132 The variation in the reported results may have resulted from differences in experimental methodology, the physical properties of the materials used, and differences between tooth compositions.33 For instance, significantly lower fracture resistance has been reported for FRC under cyclic versus static loading.34
Most previous studies emphasized that the main function of the post is retaining core build-up, rather than strengthening the tooth. It has previously been shown that composite cores alone can have similar results to posts and cores.28 But, this study showed inferior results for composite-alone compared to cast and FRC post and core restorations for teeth with extensive structural loss. Our study also confirms the clinical validity of FRC restoration. Providing a ferrule length of 1.5 - 2.0 mm is highly recommended, as it may contribute to a more favorable fracture pattern.35 Most fractures in this study were at the junction of posts and cores, or in part of the dentin in the ferrule length, thus providing additional opportunities to restore the teeth. The method of ferrule preparation can also affect the fracture patterns. The ferrule in this study was prepared as conservatively as possible (Figure 1), which may have contributed to the restorable fracture patterns observed in some cast posts and cores (42%). The effect of thermo-mechanical aging is important, and may have resulted in a different outcome than has been reported in other studies.28 Silication followed by silanation of posts and cores has yielded promising results and should be further evaluated in future studies.36
The upper central incisors were chosen for this study because of their importance in facial esthetics and their need for restoration. Because of limitations of time and the availability of upper central incisors, in the present study the teeth in the control group were standardized by preparation for crown restoration with similar dimensions. The highest fracture resistance was observed in the control group, with most of the fractures occurring with a similar pattern and limited to the middle third of the tooth, confirming a similar distribution of applied force. Seven samples (58%) in the cast post and core group had vertical root fractures that were categorized as non-restorable. Considering the emphasis in the literature that the main function of the post is to act as a core retainer, rather than strengthening the tooth, the clinical use of FRC is favorable because of its associated fracture pattern. FRC appears to dissipate forces along the root canal, reducing stresses on the root.37 When the forces exceed tolerance, FRC absorbs the stresses and fractures at the coronal portion, without root fracture.10
A limitation of this study was that the biochemical properties of the extracted teeth such as dentin sclerosis in relation to age and race were not known, even though such factors can affect root resistance to fracture.38 Although samples were subjected to thermo-mechanical aging, longer periods of artificial aging such as simulation of 5 - 10 years of clinical function would have given a better clinical prediction of restoration survival. The periodontal ligament was not simulated in this study, even though its simulation has been recommended.39 However, simulation of the periodontal ligament may have compromised the study results because of artifacts arising from the actual study materials, and in addition it can increase the risk of tooth dislodgement during mechanical cycles. For these reasons, the authors decided not to simulate the periodontal ligament.40 Another limitation was that only one type of FRC was tested. Despite these considerations and limitations, the present study attempted to imitate the natural clinical situation to the greatest extent possible, and provides insight into the stress performance and reliability of different post and core restorations for upper central incisors.
Within the limitations of this in vitro study, cast posts and cores exhibited higher fracture resistance, with most of the fractures having non-restorable patterns. FRC posts proved to be the most clinically suitable restoration with regard to esthetic and restorable fracture patterns. Composite exhibited the lowest fracture resistance for the reconstruction of upper central incisors with extensive structural loss.
Figures and Tables
Table 1
Dimensions of samples in millimetres and weight after post space and ferrule preparation (n = 12)

Table 2
Loads at fracture and their fracture modes

Acknowledgment
The authors would like to thank the Dental Material Research Center Faculty of Dentistry, Babol University of Medical Sciences, Babol, Iran for partially funding this study. The authors also express their gratitude to Ms Shams and Professor Torabinejad of the Dental Material Research Center, for their assistance with this study. Partial funding by Dental Material Research Center, Faculty of Dentistry, Babol University of Medical Sciences, Babol, Iran.
References
1. Hansen EK, Asmussen E, Christiansen NC. In vivo fractures of endodontically treated posterior teeth restored with amalgam. Endod Dent Traumatol. 1990; 6:49–55.

2. Qing H, Zhu Z, Chao Y, Zhang W. In vitro evaluation of the fracture resistance of anterior endodontically treated teeth restored with glass fiber and zircon posts. J Prosthet Dent. 2007; 97:93–98.

3. Sahafi A, Peutzfeldt A, Asmussen E, Gotfredsen K. Retention and failure morphology of prefabricated posts. Int J Prosthodont. 2004; 17:307–312.
4. Nergiz I, Schmage P, Ozcan M, Platzer U. Effect of length and diameter of tapered posts on the retention. J Oral Rehabil. 2002; 29:28–34.

5. Fernandes AS, Shetty S, Coutinho I. Factors determining post selection: a literature review. J Prosthet Dent. 2003; 90:556–562.

6. Duret B, Reynaud M, Duret F. New concept of corono-radicular reconstruction: the Composipost (1). Chir Dent Fr. 1990; 60:131–141.
7. Duret B, Reynaud M, Duret F. A new concept of coronoradicular reconstruction, the Composipost (2). Chir Dent Fr. 1990; 60:69–77.
8. Fredriksson M, Astbäck J, Pamenius M, Arvidson K. A retrospective study of 236 patients with teeth restored by carbon fiber-reinforced epoxy resin posts. J Prosthet Dent. 1998; 80:151–157.

9. Ferrari M, Vichi A, Mannocci F, Mason PN. Retrospective study of the clinical performance of fiber posts. Am J Dent. 2000; 13:9B–13B.
10. Strassler HE, Cloutier PC. A new fiber post for esthetic dentistry. Compend Contin Educ Dent. 2003; 24:742–748.
11. Fovet Y, Pourreyron L, Gal JY. Corrosion by galvanic coupling between carbon fiber posts and different alloys. Dent Mater. 2000; 16:364–373.

12. Lidén C, Norberg K. Nickel on the Swedish market. Follow-up after implementation of the Nickel Directive. Contact Dermatitis. 2005; 52:29–35.

13. Vichi A, Vano M, Ferrari M. The effect of different storage conditions and duration on the fracture strength of three types of translucent fiber posts. Dent Mater. 2008; 24:832–838.

14. Monticelli F, Ferrari M, Toledano M. Cement system and surface treatment selection for fiber post luting. Med Oral Patol Oral Cir Bucal. 2008; 13:E214–E221.
15. Varvara G, Perinetti G, Di Iorio D, Murmura G, Caputi S. In vitro evaluation of fracture resistance and failure mode of internally restored endodontically treated maxillary incisors with differing heights of residual dentin. J Prosthet Dent. 2007; 98:365–372.

16. Naumann M, Preuss A, Rosentritt M. Effect of incomplete crown ferrules on load capacity of endodontically treated maxillary incisors restored with fiber posts, composite build-ups, and all-ceramic crowns: an in vitro evaluation after chewing simulation. Acta Odontol Scand. 2006; 64:31–36.

17. Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence of vertical root fracture of pulpless teeth restored with six post-and-coresystems. J Prosthet Dent. 1999; 81:262–269.

18. Zhang XH, Tong D, Wang XZ. The measurement and comparison of shear fracture strength and shear bond strength between carbon fiber post and some other posts. Zhonghua Kou Qiang Yi Xue Za Zhi. 2003; 38:339–341.
19. Heydecke G, Butz F, Strub JR. Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: an in-vitro study. J Dent. 2001; 29:427–433.

20. Kim JH, Park SH, Park JW, Jung IY. Influence of post types and sizes on fracture resistance in the immature tooth model. J Korean Acad Conserv Dent. 2010; 35:257–266.

21. Ferrari M, Cagidiaco MC, Goracci C, Vichi A, Mason PN, Radovic I, Tay F. Long-term retrospective study of the clinical performance of fiber posts. Am J Dent. 2007; 20:287–291.
22. Jung RE, Kalkstein O, Sailer I, Roos M, Hämmerle CH. A comparison of composite post buildups and cast gold post-and-core buildups for the restoration of nonvital teeth after 5 to 10 years. Int J Prosthodont. 2007; 20:63–69.
23. Dallari A, Rovatti L. Six years of in vitro/in vivo experience with Composipost. Compend Contin Educ Dent Suppl. 1996; S57–S63.
24. Duret B, Duret F, Reynaud M. Long-life physical property preservation and postendodontic rehabilitation with the Composipost. Compend Contin Educ Dent Suppl. 1996; S50–S56.
25. Cormier CJ, Burns DR, Moon P. In vitro comparison of the fracture resistance and failure mode of fiber, ceramic, and conventional post systems at various stages of restoration. J Prosthodont. 2001; 10:26–36.

26. Hayashi M, Takahashi Y, Imazato S, Ebisu S. Fracture resistance of pulpless teeth restored with post-cores and crowns. Dent Mater. 2006; 22:477–485.

27. Ferrario VF, Sforza C, Serrao G, Dellavia C, Tartaglia GM. Single tooth bite forces in healthy young adults. J Oral Rehabil. 2004; 31:18–22.

28. Bolay Ş, Öztürk E, Tuncel B, Ertan A. Fracture resistance of endodontically treated teeth restored with or without post systems. J Dent Sci. 2012; 7:148–153.

29. Maccari PC, Cosme DC, Oshima HM, Burnett LH Jr, Shinkai RS. Fracture strength of endodontically treated teeth with flared root canals and restored with different post systems. J Esthet Restor Dent. 2007; 19:30–36.

30. Rosentritt M, Fürer C, Behr M, Lang R, Handel G. Comparison of in vitro fracture strength of metallic and tooth-coloured posts and cores. J Oral Rehabil. 2000; 27:595–601.

31. Maccari PC, Conceição EN, Nunes MF. Fracture resistance of endodontically treated teeth restored with three different prefabricated esthetic posts. J Esthet Restor Dent. 2003; 15:25–30.

32. Nothdurft FP, Seidel E, Gebhart F, Naumann M, Motter PJ, Pospiech PR. Influence of endodontic posts on the fracture behavior of crowned premolars with class II cavities. J Dent. 2008; 36:287–293.

33. Fernandes AS, Dessai GS. Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont. 2001; 14:355–363.
34. Drummond JL, Bapna MS. Static and cyclic loading of fiber-reinforced dental resin. Dent Mater. 2003; 19:226–231.

35. Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M. Ferrule effect: a literature review. J Endod. 2012; 38:11–19.

36. Keum HJ, Yoo HM. Effect of surface treatments of fiber posts on bond strength to composite resin cores. J Korean Acad Conserv Dent. 2010; 35:173–179.

37. Newman MP, Yaman P, Dennison J, Rafter M, Billy E. Fracture resistance of endodontically treated teeth restored with composite posts. J Prosthet Dent. 2003; 89:360–367.

38. Mireku AS, Romberg E, Fouad AF, Arola D. Vertical fracture of root filled teeth restored with posts: the effects of patient age and dentine thickness. Int Endod J. 2010; 43:218–225.

39. Soares CJ, Pizi EC, Fonseca RB, Martins LR. Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res. 2005; 19:11–16.

40. Libman WJ, Nicholls JI. Load fatigue of teeth restored with cast posts and cores and complete crowns. Int J Prosthodont. 1995; 8:155–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download