Abstract
Traditionally, apexification has been used to treat immature permanent teeth that have lost pulp vitality. This technique promotes the formation of an apical barrier to close the open apex so that the filling materials can be confined to the root canal. Because tissue regeneration cannot be achieved with apexification, a new technique called regenerative endodontic treatment was presented recently to treat immature permanent teeth. Regenerative endodontic treatment is a treatment procedure designed to replace damaged pulp tissue with viable tissue which restores the normal function of the pulp-dentin structure. After regenerative endodontic treatment, continued root development and hard tissue deposition on the dentinal wall can occur under ideal circumstances. However, it is difficult to predict the result of regenerative endodontic treatment. Therefore, the purpose of this study was to summarize multiple factors effects on the result of regenerative endodontic treatment in order to achieve more predictable results. In this study, we investigated the features of regenerative endodontic treatment in comparison with those of other pulp treatment procedures and analyzed the factors that have an effect on regenerative endodontic treatment.
The purpose of pulp treatment is to maintain the tooth structure intact in order to preserve optimal function. Maintaining the vitality of teeth damaged due to dental caries or trauma is also one of the purposes of pulp treatment. Especially, in case of immature permanent teeth, maintaining the pulp vitality is essential for continuous root development and apical closure. If the pulp of immature permanent teeth is infected, apexification that includes removal of the infected pulp and application of calcium hydroxide has been performed traditionally.1 Calcium hydroxide is the material of choice for closing the apical foramen. However, while apexification can induce apical closure, it cannot maintain pulp vitality.2 Recently, regenerative endodontic treatment procedure has been suggested in order to replace the damaged pulp tissue with the viable tissue. Especially when the tooth is damaged by trauma, pulp regenerative endodontic treatment is performed because the pulp tissue is uninfected. On the other hand, when apical periodontitis is associated with tooth infection, regenerative endodontic treatment procedure is not considered. But recently, a case report demonstrated continuous root develoment and apical closure with the application of antibiotics.3 Procedures used in this case reports are based on the concept that stem cells have self-regenerating capacity and are multipotent. Stem cells are used to induce pulp regeneration so as to treat immature permanent teeth in a conservative way.4
In apexification, calcium hydroxide is used as an intracanal medication, which should be replaced every 3 months, and a long-term follow-up is necessary. Long-term application of the intra-canal medication increases the possibility of root fracture and developing defects in the root walls due to its porous characteristics.12 On the other hand, regenerative endodontic treatment can result in complete root development after a short-term treatment procedure. Thus, regenerative endodontic treatment causes an increase in root length and thickness.356789
Regenerative endodontic treatment is a procedure that involves disinfection of the root canal with the use of antibiotics. Multiple aerobic and anaerobic bacteria cause infection of the root canals, and hence it is difficult to disinfect the canals effectively with just one type of antibiotic. Therefore, Hoshino and Sato recommended a combination of three antibiotics including ciprofloxacin, metronidazole, minocycline.1011 In this study, various aspects of regenerative endodontic treatment such as clinical features, biological features, and their effects on regenerative endodontic treatment are discussed.
Since many types of regenerative endodontic treatment procedures have been suggested, it is important to have knowledge of the procedure that is generally used. The American Association of Endodontics (AAE) suggests that regenerative endodontic treatment can be used for teeth of a compliant patient with necrotic pulp, an immature apex, and pulp space not needed for post and core. At the first appointment for regenerative endodontic treatment, risks and potential benefits should be explained to the patient after collecting the clinical information and establishing a pulpal and periradicular diagnosis. The tooth is anesthetized and isolated with rubber dam for creating an access opening. Copious, gentle irrigation with 20 mL sodium hypochlorite (NaOCl) using an irrigation system that minimizes the possibility of extrusion of irrigants into the periapical space and lower concentrations of NaOCl are advised to minimize cytotoxicity to stem cells in the apical tissues. The root canal is then dried with sterile paper points, and the antimicrobial medicament is applied into the canal space. A triple antibiotic paste is applied to disinfect the canal space.12 The triple antibiotic paste has the advantage of being a very effective antibiotic combination against intracanal microorganisms.1011 On the other hand, calcium hydroxide has the advantage of being widely available, but it may be cytotoxic to stem cells.13 After the antimicrobial medicament is applied, the tooth is sealed with a temporary filling, and the patient should be asked to visit for a check-up after 3 to 4 weeks.
At the second appointment, the patient is evaluated for resolution of signs or symptoms of an acute infection. If there are no symptoms or signs of infection, it is appropriate to proceed with the next step of the regenerative endodontic treatment. Local anesthetic without vasocontrictors is recommended at this appointment to avoid the disturbance of intracanal bleeding. After rubber dam isolation and making a coronal access opening, the tooth is irrigated with 20 mL of ethylenediamine tetraacetic acid, followed by normal saline, and the antimicrobial medicament is carefully removed. After drying the canal with a paper point, a file is placed a few milimeters beyond the apical foramen and bleeding is induced up to 3 mm from the cemento-enamel junction (CEJ). To position the mineral trioxide aggregate (MTA), Colla-Plug, which serves as a resorbable matrix, is placed into the canal. Then about 3 mm of MTA is placed, followed by placement of the final restoration.12 A 12 to 18 month recall is probably the minimal time to judge radiographic evidence of root development and to conduct the clinical examination.13
There are several treatment options for a necrotic or infected immature permanent tooth. Traditionally, the apexification procedure has been recommended for treating an immature tooth with an open apex. Apexification is a procedure that promotes the formation of an apical barrier to prevent the extrusion of filling materials.14 Materials such as calcium hydroxide which are capable of forming a calcified apical barrier are used for apexification. Although calcium hydroxide can be used to form a calcified apical barrier, it has some drawbacks.2 The most critical drawback is the reduction in root strength due to the use of calcium hydroxide, and this increases the possibility of root fracture. Another drawback is the long time span of the entire treatment. At least 6 months are required to create an apical barrier, and mulitple visits are needed to replenish calcium hydroxide.15 Due to these drawbacks, alternative apexification methods have been proposed recently. MTA has been proposed as a material to create an apical barrier that prevents the extrusion of obturation materials. In comparison with calcium hydroxide, MTA is used in the one or two step apexification procedure, and therefore a fewer number of appointments are needed.13 In spite of this advantage, apexification with MTA neither strengthens the root nor induces further root development. As a result, the roots remain thin and fragile, and hence another treatment approach is needed.14 It has been recently suggested that regenerative endodontic treatment can be alternative approach of apexification. Regenerative endodontic treatment has the advantages of further root development and reinforcement of dentinal walls by deposition of hard tissue, thus strengthening the root against fracture.16 The characteristics of three treatment procedures are summarized in Table 1.
Considering these characteristics, regenerative endodontic treatment seems to be the most effective procedure. However, without clinical data of comparison of the outcomes of these three treatment procedures, it is difficult to determine which procedure is the most effective to treat an immature tooth with a necrotic pulp. Jeeruphan conducted a retrospective study about the comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic treatment or apexification. A total of 61 cases were included in this study. The cases included regenerative endodontic treatment (20 cases), apexification with MTA (19 cases), and apexification with calcium hydroxide (22 cases). In this retrospective study, the percentage increase in root width and root length after the treatment procedure was analyzed using radiographic data (Table 2).14
Immature teeth treated with regenerative endodontic treatment showed a significantly higher percentage increase in root width (28.2%) and root length (14.9%) as compared with teeth treated by either apexification with MTA (percentage increase in root width, 0.00% and percentage increase in root length, 6.1%) or apexification with calcium hydroxide (percentage increase in root width, 1.52% and percentage increase in root length, 0.4%).14 The results of this study indicated that regenerative endodontic treatment has the advantage of promoting further root development and thickening of dentinal walls by hard tissue deposition.
Regenerative endodontic treatment can occur in infected immature permanent teeth because of mesenchymal stem cells which exist in the apical papilla of immature teeth. These stem cells from the apical papilla (SCAP) are capable of differentiating into odontoblast-like cells forming root dentin.417 Another type of mesenchymal cells, which are called dental pulp stem cells (DPSCs) were discovered and isolated earlier, and DPSCs have the ability to differentiate into odontoblast-like cells and form dentin/pulp-like complex when implanted into subcutaneous spaces of immunocompromised mice.18 Both SCAP and DPSCs are as potent in osteo/dentinogenic differentiation as mesenchymal cells from bone marrows, whereas they are weaker in adipogenic potential.17 SCAP and DPSCs show similar features, but they have some differences. In order to examine the differences between SCAP and DPSCs, both cells were isolated from the same tooth and cultured under the same conditions.4 It was found that SCAP showed a significantly greater bromodeoxyuridine uptake rate (an indication of cell proliferation), number of population doublings, and tissue regeneration capacity than DPSCs (Table 3). These evidences suggest that SCAP derived from a developing tissue may be a superior cell source for tissue regeneration.19
There are some factors that affect the results of regenerative endodontic treatment. To achieve successful results of the treatment procedure, a thorough understanding of these factors is very important. The first factor is the disinfection of the canal. During the early stage of research, the regenerative endodontic treatment of pulp tissue in an infected tooth was thought to be impossible. The first attempt at regenerative endodontic treatment of an avulsed immature tooth with necrotic non-infected pulp was successful.3 Therefore, researchers suggested that regenerative endodontic treatment will occur if it was possible to create an environment similar to the avulsed tooth. In other words, if the canals were effectively disinfected and the coronal access was effectively sealed, regenerative endodontic treatment should occur as in an avulsed tooth. To disinfect the canal, many types of medications are used nowadays.3
The second factor is the apex diameter. A tooth with an open apex allows the migration of mesenchymal stem cells into the root canal space, and this could allow host cell homing to form new tissue in the root canal space.2021 An apical opening of 1.1 mm in diameter or larger is beneficial, with natural regenerative endodontic treatment occurring in approximately 18% to 34% of teeth with immature roots.22
The third factor is the patient age. Several case reports of regenerative endodontic treatment procedures have generally been limited to patients who are reaching adolescence, mostly aged from 8 - 16 years.362223 Based on these case reports, it would not be advisable to perform regenerative endodontic treatment procedures in children younger than 8 years or older than 16 years. Also, regenerative endodontic treatment procedure should not be performed on deciduous teeth, because of the possible risk of impairing the eruption pattern of permanent teeth.22 The three factors that affect the results of regenerative endodontic treatment are summarized in Table 4.
Banchs and Trope reported successful multiple visit regenerative endodontic treatment of the lower right second premolar in an 11 year-old boy.3 During the first visit, access opening, canal irrigation and application of tri-antibiotic paste were performed. The patient returned 26 days later for the second visit, and after this a two year follow-up was performed. During this period, the radiograph showed closure of the apex and thickening of the dentinal walls.3 Chueh and Huang also suggested multiple visit regenerative endodontic treatment to achieve successful results.23 Regenerative endodontic treatment of an immature tooth was performed in a 10 year-old girl. During the first visit, an access cavity was made, followed by canal irrigation and application of tri-antibiotic paste. Thirty-five months after the initial treatment, the radiographs showed a reduction of the root canal space and maturation of the root apex.23 In contrast, Shin et al. performed single visit regenerative endodontic treatment of the lower right second premolar in a 12 year-old girl.6 An access cavity was made, and the coronal portion of the canal was irrigated with 10 mL of 6% NaOCl. After rinsing the canal with sterile saline solution, the canal was irrigated with 10 mL of 2% chlorhexidine gluconate and it was allowed to remain in the canal for 5 minutes. The canal was dried with paper points and MTA was placed into the canal. Finally, the access cavity was filled with resin-bonded composite restoration. At the 13 and 19 month follow-up, the radiographs showed evidence of complete periradicular bone healing and root maturation. In this case, a single visit regenerative endodontic treatment protocol was successful, because the tooth exhibited partial pulpal necrosis. If the tooth had complete pulpal necrosis, this protocol would not have been successful. Therefore, it seems that a multiple visit protocol using a tri-antibiotic paste may be better treatment option for teeth with complete pulpal necrosis. Hence, case selection is critical when deciding which regenerative endodontic treatment protocol is ideal for a particular pulpal condition.6 The above three cases of regenerative endodontic treatment are summarized in Table 5.
In 1996, Hoshino et al. recommended a tri-antibiotic paste, which was composed of ciprofloxacin, metronidazole, and minocycline, to disinfect the canal, and this medicament can be used effectively in regenerative endodontic treatment.10 On the other hand, Chueh et al. reported that complete disinfection of the canal and regeneration can be achieved by using calcium hydroxide alone.24 In 2009, Bose et al. analyzed cases of regenerative endodontic treatment performed all over the world.13 Regenerative endodontic treatment with the triple antibiotic paste, calcium hydroxide, and formocresol produced significantly greater increases in root length and width compared with that in the control group. There were no significant differences in root length among the three groups of medicaments. In terms of changes in root width, the triple antibiotic paste produced significantly greater increases in dentin wall thickness compared with the other two medicament groups.1213 Although application of the triple antibiotic paste can be effective, drawbacks of the triple antibiotic paste have been reported recently. Ding et al. reported that two patients suffered from pain after the application of the triple antibiotic paste, and they were excluded from the research.25 Jung et al. reported the development of a persistent sinus tract after using triple antibiotic paste.26 They replaced this intracanal medicament with calcium hydroxide, after which the symptoms of the patient settled down.26
Especially, when the triple antibiotic paste is placed in contact with the anterior teeth, discoloration can occur. According to Kim et al., minocycline, which is one of the components of the triple antibiotic paste is the main cause of tooth discoloration. Minocycline can penetrate the tooth through dentinal tubules, and it can integrate with the crystal structure of the tooth.27 Administration of minocycline is contraindicated in pregnant women who are in the 3rd trimester or in children who are under 8 years of age, due to the induction of tooth discoloration, reduction of bone growth, and amelogenesis imperfecta.28 Reynolds reported the methods to prevent tooth discoloration. One method is sealing the coronal dentin wall with flowable resin before application of the triple antibiotic paste, and the other method is retrograde filling of antibiotics with 20 gauge needle to minimize the contact with the coronal part of teeth.27 There are case reports suggesting that cefaclor, amoxicillin should be used instead of minocycline. But amoxicillin has side effects such as an allergic reaction.29
Another material that is used in the regenerative endodontic treatment procedure is MTA. The coronal space is usually filled with MTA after inducing bleeding with a file. The reason why MTA is used in regenerative endodontic treatment is that MTA has a remarkable biocompatibility and sealing ability. MTA is also able to set in a moist environment such as the bleeding area of the tooth.30
In conclusion, there are no guidelines regarding which medicament should be used for regenerative endodontic treatment for specific situations, and the results of regenerative endodontic treatment are at odds with the medicaments that are used for treatment. Therefore, disinfection of canals and preservation of the tissue vitality are more important than selection of the medicament. If these factors can be controlled, successful results of the regenerative endodontic treatment procedure can be obtained.
Regenerative endodontic treatment is based on the concept that multipotent stem cells from the apical area are able to induce pulp regeneration in immature permanent teeth. As a result of this concept, the treatment becomes more conservative.24 SCAP are known to have a greater differentiation capacity than other stem cells and they are loosely attached to the root apical area. The root apical area contains an abundant number of stem cells which are responsible for root development. Even when the pulp becomes necrotic, SCAP are able to maintain their vitality through collateral circulation.31 The size of the apical foramen is an important factor that needs to be considered for successful regenerative endodontic treatment. Regenerative endodontic treatment of avulsed teeth was more successful when the diameter of the apical foramen was greater than 1.1 mm. This is because a bigger size of apical foramen allows more blood to be supplied.22 In terms of the frequency of application of antibiotics for treatment of infected root canal, it was found that repeated application of antibiotics increases their antibacterial efficacy.10 A combination of three antibiotics is very effective in disinfecting dentin in the root. This triple antibiotic paste is composed of ciprofloxacin, metronidazole, and minocycline in a 1 : 1 : 1 ratio.1011 The drawbacks of the triple antibiotic paste such as discoloration of the crown, increase in bacterial resistance and allergic reactions have been reported.32 MTA is being used as the final canal filling material when the tooth is treated by the regenerative endodontic treatment procedure.325 MTA allows cell proliferation and cell attachment because it has less cytotoxicity and good biocompatibility.31 These characteristics enhance the tissue healing process and prevent the weakening of the dentin structure which was caused by long-term administration of calcium hydroxide.33 The regenerative endodontic treatment procedure is based on the conservative concept that recommends treatment by induction of pulp regeneration; however, if the procedure fails, conventional root canal therapy should be performed. Therefore, dentists should explain to the patients that there is a possibility that conventional root canal therapy may be performed before the initiation of regenerative endodontic treatment procedure. Especially for the treatment of molars, the regenerative endodontic treatment procedure has many disadvantages such as discoloration of root canal and access cavity, limited access due to canal calcification, and difficulty in MTA removal. Therefore, prudent case selection is important and when applying MTA, local application of MTA over the canal orifice is recommended. After filling the canals with MTA, a periodic check-up is necessary.
Recently many cases of regenerative endodontic treatment of teeth with infected canals have been reported. But these cases do not provide clinical results such as the long-term success rate of regenerative endodontic treatment. Therefore, to achieve successful results of the regenerative endodontic treatment procedure, prudent case selection and a long-term follow-up are considered to be very important.
Figures and Tables
Figure 1
The current considerations for regenerative endodontic treatment procedures (Courtesy of the American Association of Endodontics). NaOCl, sodium hypochlorite; EDTA, ethylenediaminetetraacetic acid; MTA, mineral trioxide aggregate.

Table 1
The characteristics of three treatment procedures for immature root formation

Table 2
The percentage increase in root width and root length after the treatment procedure
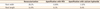
| Revascularization | Apexification with MTA | Apexification with calcium hydroxide | |
|---|---|---|---|
| Root width | 28.2% | 0.00% | 1.52% |
| Root length | 14.9% | 6.1% | 0.4% |
Table 3
Comparison between stem cells from the apical papilla (SCAP) and dental pulp stem cells (DPSCs)

Table 4
Factors that affect the results of revascularization

Table 5
Case reports of multiple visit & single visit revascularization

Acknowledgement
This study was supported by the National Research Foundation of Korea grant funded by the Korea government (MSIP) (no. 2011-0030121) and Chonnam National University, 2013.
References
3. Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004; 30:196–200.

4. Huang GT, Sonoyama W, Liu Y, Liu H, Wang S, Shi S. The hidden treasure in apical papilla: the potential role in pulp/dentin regeneration and bioroot engineering. J Endod. 2008; 34:645–651.

5. Shah N, Logani A, Bhaskar U, Aggarwal V. Efficacy of revascularization to induce apexification/apexogensis in infected, nonvital, immature teeth: a pilot clinical study. J Endod. 2008; 34:919–925.

6. Shin SY, Albert JS, Mortman RE. One step pulp revascularization treatment of an immature permanent tooth with chronic apical abscess: a case report. Int Endod J. 2009; 42:1118–1126.

7. Forghani M, Parisay I, Maghsoudlou A. Apexogenesis and revascularization treatment procedures for two traumatized immature permanent maxillary incisors: a case report. Restor Dent Endod. 2013; 38:178–181.

8. Hotwani K, Sharma K. Platelet rich fibrin - a novel acumen into regenerative endodontic therapy. Restor Dent Endod. 2014; 39:1–6.

9. Goyal L. Clinical effectiveness of combining platelet rich fibrin with alloplastic bone substitute for the management of combined endodontic periodontal lesion. Restor Dent Endod. 2014; 39:51–55.

10. Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K, Iwaku M. In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J. 1996; 29:125–130.

11. Sato I, Ando-Kurihara N, Kota K, Iwaku M, Hoshino E. Sterilization of infected root-canal dentine by topical application of a mixture of ciprofloxacin, metronidazole and minocycline in situ. Int Endod J. 1996; 29:118–124.

12. Hargreaves KM, Law AS. Regenerative Endodontics. In : Hargreaves KM, Cohen S, editors. Pathways of the Pulp. 10th ed. St Louis, MO: Mosby Elsevier;2011. p. 602–619.
13. Bose R, Nummikoski P, Hargreaves K. A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. J Endod. 2009; 35:1343–1349.

14. Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod. 2012; 38:1330–1336.

15. Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002; 18:134–137.

16. Witherspoon DE, Small JC, Regan JD, Nunn M. Retrospective analysis of open apex teeth obturated with mineral trioxide aggregate. J Endod. 2008; 34:1171–1176.

17. Sonoyama W, Liu Y, Yamaza T, Tuan RS, Wang S, Shi S, Huang GT. Characterization of the apical papilla and its residing stem cells from human immature permanent teeth: a pilot study. J Endod. 2008; 34:166–171.

18. Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A. 2000; 97:13625–13630.
19. Sonoyama W, Liu Y, Fang D, Yamaza T, Seo BM, Zhang C, Liu H, Gronthos S, Wang CY, Wang S, Shi S. Mesenchymal stem cell-mediated functional tooth regeneration in swine. PLoS One. 2006; 1:e79.

20. Lovelace TW, Henry MA, Hargreaves KM, Diogenes A. Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. J Endod. 2011; 37:133–138.

21. Kim JY, Xin X, Moioli EK, Chung J, Lee CH, Chen M, Fu SY, Koch PD, Mao JJ. Regeneration of dental-pulp-like tissue by chemotaxis-induced cell homing. Tissue Eng Part A. 2010; 16:3023–3031.

22. Garcia-Godoy F, Murray PE. Recommendations for using regenerative endodontic procedures in permanent immature traumatized teeth. Dent Traumatol. 2012; 28:33–41.

23. Chueh LH, Huang GT. Immature teeth with periradicular periodontitis or abscess undergoing apexogenesis: a paradigm shift. J Endod. 2006; 32:1205–1213.

24. Chueh LH, Ho YC, Kuo TC, Lai WH, Chen YH, Chiang CP. Regenerative endodontic treatment for necrotic immature permanent teeth. J Endod. 2009; 35:160–164.

25. Ding RY, Cheung GS, Chen J, Yin XZ, Wang QQ, Zhang CF. Pulp revascularization of immature teeth with apical periodontitis: a clinical study. J Endod. 2009; 35:745–749.

26. Jung IY, Lee SJ, Hargreaves KM. Biologically based treatment of immature permanent teeth with pulpal necrosis: a case series. J Endod. 2008; 34:876–887.

27. Kim JH, Kim Y, Shin SJ, Park JW, Jung IY. Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod. 2010; 36:1086–1091.

28. Dummett CO, Thikkurissy S. Anomalies of the developing dentition. In : Casamassimo PS, Fields HW, McTigue DJ, Nowak A, editors. Pediatric dentistry. Infancy through adolescence. 5th ed. Philadelphia: WB Saunders Co.;2013. p. 54–80.
29. Thomson A, Kahler B. Regenerative endodontics-biologically-based treatment for immature permanent teeth: a case report and review of the literature. Aust Dent J. 2010; 55:446–452.

30. D'Arcangelo C, D'Amario M. Use of MTA for orthograde obturation of nonvital teeth with open apices: report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:e98–e101.
31. Huang GT. A paradigm shift in endodontic management of immature teeth: conservation of stem cells for regeneration. J Dent. 2008; 36:379–386.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download