Abstract
When a tooth shows discoloration and does not respond to the cold test or electric pulp test (EPT) after a traumatic injury, its diagnosis can be even more difficult due to the lack of proper diagnostic methods to evaluate its vitality. In these case reports, we hope to demonstrate that ultrasound Doppler might be successfully used to evaluate the vitality of the tooth after trauma, and help reduce unnecessary endodontic treatments. In all three of the present cases, the teeth were discolored after traumatic injuries and showed negative responses to the cold test and EPT. However, they showed distinctive vital reactions in the ultrasound Doppler test during the whole observation period. In the first case, the tooth color returned to normal, and the tooth showed a positive response to the cold test and EPT at 10 wk after the injury. In the second case, the tooth color had returned to its normal shade at 10 wk after the traumatic injury but remained insensitive to the cold test and EPT. In the third case, the discoloration was successfully treated with vital tooth bleaching.
Tooth vitality is determined using the cold test, electric pulp test (EPT), radiographic examination, or clinical signs such as tooth discoloration. However, tooth vitality could be more properly evaluated by the blood supply in the pulp rather than these other tests, such as the cold test and EPT, which actually evaluate the sensitivity of the nerves.1 When the tooth experience a traumatic injury, the evaluation of tooth vitality is difficult because they occasionally do not respond to the cold test or EPT due to the reduced conduction ability of the sensory nerves or nerve endings.2 This lack of response seems to be caused by the damage, inflammation, compression or tension state of the apical nerve fibers, which require approximately eight weeks or more to return to normal functioning.3
Tooth discoloration may follow a traumatic injury.4,5 When the tooth shows discoloration and also does not respond to the cold test or EPT after a traumatic injury, its diagnosis can be even more difficult due to the lack of proper diagnostic methods to evaluate its vitality. The discolored tooth may return to its original shade and translucency completely or incompletely when the tooth vitality is preserved.4,5 Malgren and Hubel reported that the discoloration disappeared within 4 weeks to 6 months in eight out of nine permanent teeth that had been root fractured and showed tooth discoloration after the trauma.6 They reported that all of the teeth had regained their normal sensibility when the discoloration disappeared. Transient color changes were also described in connection with transient apical breakdown (TAB) after luxation injuries in permanent teeth.7,8 The discoloration and loss of electrometric sensibility returned to normal when there was radiographic evidence of the resolution of the TAB. However, this resolution usually takes a long time to be confirmed.
Ultrasound Doppler imaging has been used in many medical fields as a non-invasive and radiation-free technique to assess the blood flow in micro-vascular systems. Ultrasound has also recently been applied to dentistry. Some studies have shown that ultrasound Doppler imaging provides sufficient information on micro-vascularity for dental treatment.9-11
Recently, Yoon et al. reported that ultrasound Doppler could be effectively used to evaluate the pulp blood flow in the pulp spaces.1,12 They reported that it can measure the reduced blood stream speed after a local anesthetic injection containing 1 : 80,000 epinephrine. They also indicated the possibility that this Doppler system could be used effectively in the diagnosis of traumatic injury.12
In this paper, three cases are presented that were seen in the Department of Conservative Dentistry, Yonsei University Dental Hospital, Seoul, Korea, during the past two years. In the beginning, all three teeth were discolored after a traumatic injury and showed negative responses to the thermal test and EPT but also showed a distinctive vital reaction in the ultrasound Doppler test unit (MM-D-K, Minimax, Moscow, Russia). In the first and second cases, the tooth discolorations returned to normal at 10 weeks after the injuries. In the third case, the tooth discoloration was successfully treated by vital bleaching. In this case series, we hope to demonstrate that ultrasound Doppler might be successfully used to evaluate the vitality of teeth after trauma and help reduce unnecessary endodontic treatments.
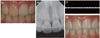
A 47-year-old female patient visited our department due to traumatic injury to her upper right lateral incisor (tooth #12). She sustained the injury 3 days before she visited our clinic by a fist blow injury to her face. Tooth #12 was subluxated, and showed a positive response to a percussion test. It did not show any response to a cold test or EPT. The tooth was diagnosed with subluxation, and we decided to wait and observe its course. There was no discomfort during the 2 weeks after the injury, but there was no response to the thermal test or EPT, and a reddish discoloration was observed (Figure 1a).
At 6 weeks after the injury, the patient did not show any discomfort, but the discoloration lasted, and the tooth did not respond to cold or EPT. We decided to use the ultrasound Doppler unit to evaluate the vitality of the pulp, and the result was shown in Figure 1b. Tooth #12 produced a typical pulsated image, which represents normal vital pulp (Figure 1b). We explained the results and implications of the test to the patient. We decided to continue to wait and observe the tooth because the patient had no discomfort, did not mind the discoloration at that time, and was willing to wait to determine whether the tooth could recover to normal without any treatment. At 10 weeks after the injury, the tooth had returned to a normal shade and regained its normal responses to the cold test and EPT (Figure 1c).
A 30-year-old female patient visited our clinic for further treatment of traumatized anterior teeth. She had sustained an injury from a fall 2 weeks ago, and had visited a local clinic immediately after the trauma. The subluxated tooth #21 was splinted with composite resin and wire from tooth #13 to tooth #23, and then the local dentist referred her to our clinic. In the periapical radiographic view, the root and periapical area were normal (Figure 2a). Tooth #21 showed negative responses to the thermal test and EPT, a positive response to the percussion test, and pinkish discoloration (Figure 2b). The other teeth showed normal responses to all of the tests. In the ultrasound Doppler test, tooth #21 produced a normal pulsated response like those of the other teeth, and we were also able to hear the beat of the pulsation from the speaker (Figure 2c). At 4 weeks after the injury, tooth #21 showed normal response to percussion, again. In the other tests, the results were also the same as in the previous visit. At 6 weeks after the injury, tooth #21 still showed pinkish discoloration and negative responses to the thermal test and EPT. At 10 weeks after the injury, the shade of tooth #21 returned to normal (Figure 2d). At 12, 16, 20, and 24 weeks after the injury, the patient did not feel any discomfort at all. In the ultrasound Doppler test, tooth #21 showed a vital response, but it did not respond to the cold test or EPT. In the periapical view, the root and periapical area were within the normal range. The negative response continued throughout the follow-up period for 9 months. At that time, she was pregnant and wanted to delay her next visit until after her delivery.
A 22-year-old female patient visited our department to have her teeth bleached. She thought her teeth were generally yellowish, and she was especially unsatisfied with the shade of tooth #11, which showed yellowish brown discoloration (Figure 3a). She reported experiencing trauma to her anterior teeth when she was in primary school, and she had finished orthodontic treatment approximately 7 years before presentation. However, she did not know exactly when tooth #11 started to become discolored. In the radiograph, the coronal pulp space was obliterated, whereas the pulp space was present in the root area. There was no radiolucency in the periapical region, but the root apex was slightly shortened (Figure 3b). In the cold test, tooth #11 did not show any response, although she occasionally displayed a delayed response. The tooth did not respond to the EPT. In the ultrasound Doppler test, tooth #11 showed an image and sound typical of a vital tooth (Figure 3c). We decided to perform vital tooth bleaching first and then re-evaluate the color to decide whether restorative treatment was needed. Home bleaching was started using 15% carbamide peroxide gel (Opalescence, Ultradent, South Jordan, UT, USA). Additional home bleaching was continued only for tooth #11 after she was satisfied with the shade of her other teeth. After approximately 2 months of bleaching, she was satisfied with the shade of tooth #11 and did not want any further treatment (Figure 3d).
Pink discoloration, which may occur within 2 - 3 days after a traumatic injury, is caused by the rupture of capillaries and the release of red blood cells into the pulp chamber. Hemolysis leads to the diffusion of hemoglobin into the dentinal tubules, which shift the tooth color from pinkish to grayish-blue. Some fading of the grey-blue tint can occur when the blood supply to the pulp is maintained and the pulp survives.6
In the first case, the ultrasound Doppler showed a typical pulsated image when the tooth did not respond to the cold test and EPT in the early phase after a traumatic injury. Then, in ongoing follow-up, the Doppler test continued to show vital image, but the tooth still did not respond to the other two tests. The tooth regained its shade by 10 weeks after the traumatic injury, and its response to the cold test and EPT returned to normal. This finding is consistent with previous reports that indicated that the discoloration returned to normal when the teeth regained their vitality and demonstrating that ultrasound Doppler can be successfully used to determine the vitality of teeth during the period when they do not respond to the cold test and EPT after a traumatic injury.4-8 Ultrasound Doppler may help decrease unnecessary endodontic treatments, which could be performed due to a lack of the proper diagnostic methods after a traumatic injury.
In the first and second cases, 10 weeks were needed to regain the tooth's color and responses to the cold test and EPT. This result is consistent with a previous study in which the discoloration disappeared within 4 weeks to 6 months after root fracture resulting in tooth discoloration after trauma.6 The second case was interesting in that the discoloration returned to normal by 10 weeks after injury, but the tooth did not respond to the cold test and EPT even at 9 months after the traumatic injury, although it showed a consistent vital image in the Doppler test from the beginning. False positive responses in the ultrasound Doppler test have not yet been studied. In the present study, a 20-MHz ultrasound Doppler probe was used. The frequency of ultrasound is very important because it determines the penetration depth of the ultrasound wave. Although a 20-MHz frequency was reported to efficiently penetrate the enamel and dentin, and detect the blood flow in the pulp spaces, it might be possible to detect the blood flow outside of the pulp spaces if the thickness of the hard tissue is very thin.1,12 The potential for false positive responses with the ultrasound Doppler probe requires further investigation. In the second case, long-term follow-up is necessary to verify whether the vitality was actually maintained, which could be confirmed by a positive response to the cold test and EPT. However, in this case, the tooth returned to its normal shade by 10 weeks after the traumatic injury, which suggests that the blood supply to the pulp was maintained and the pulp survived.6 More time might be needed for the nerve fiber to heal. Further follow-up is required to determine whether the test results are true or false positive.
In the third case, the patient did not respond to the cold test and EPT, although she occasionally showed an obscure positive delayed response to the cold test. The cold test depends on the hydrodynamic movement of fluid within the dentinal tubules, which excites the A-fibers.13 Teeth with calcified pulp spaces might have normal and healthy pulps, but cold stimuli might not be able to excite the nerve endings due to the insulating effect of the thicker layer of dentin, which is the result of secondary and reactionary dentin formation.14 Ehrmann reported that EPT is particularly effective in older patients and in teeth that have limited fluid movement through the dentinal tubules as a result of dentine sclerosis and calcification of the pulp space because thermal pulp tests are usually inadequate in these situations.14 Klein reported that a patient was unlikely to respond to a cold test but may respond to an EPT if the pulp space had been significantly calcified.15 In their case, more electric pulp current was often needed to elicit a response because there was an increased dentin layer and a diminished pulp cavity or a fibrotic pulp. In the third case, tooth #11 was diagnosed as a vital tooth based on the results of the ultrasound Doppler test because it displayed a consistent positive sign throughout the observation period. In this case, the coronal pulp space was obliterated, whereas the pulp space was present in the root area. Because the ultrasound Doppler probe tip was positioned apically, there was a possibility of detecting the blood flow of the root canal. Furthermore, the patient showed a response to the cold test, although the response was delayed and inconsistent. For further research, we need more cases and studies related to ultrasound Doppler.
Other methods for evaluating the vascularity of pulp are laser Doppler and pulse oximetry.16-20 Laser Doppler applies a laser to transmit light into the pulp blood vessels through the tooth structure, and a red and infrared LED light beam is used in pulse oximetry for the same purpose. However, the discoloration of the tooth caused by the deposition of blood pigments in the traumatized tooth may hinder the penetration of light in both laser Doppler and pulse oximetry.18,20,21 The ultrasound wave used in the ultrasound Doppler unit can detect blood flow regardless of coronal discoloration, so it can be more useful for discolored teeth.
Tooth discoloration after a traumatic injury was corrected when the ultrasound Doppler produced a typical pulsated image, which represents normal vital pulp. Ultrasound Doppler might be an effective tool to evaluate tooth vitality when the cold test and EPT do not give proper information, especially after a traumatic injury. However, the use of ultrasound Doppler requires further research on the potential for false positive and negative responses to increase its clinical reliability.
Figures and Tables
Figure 1
(a) In case 1, discoloration of tooth #12 was observed at 2 weeks after the injury; (b) The result of an ultrasound Doppler test at 6 weeks after the injury. It shows a typical pulsated image, which represents normal vital pulp; (c) At 10 weeks after the injury, the tooth had returned to a normal shade.

Figure 2
(a) In case 2, tooth #21 was splinted at a local clinic after a subluxation injury that had occurred 2 weeks before the patient visited our clinic. It showed a negative response to the thermal test and EPT, and a positive response to the percussion test; (b) Tooth #21 showed pinkish discoloration; (c) In the ultrasound Doppler test, tooth #21 showed a normal pulsated response like that of the other teeth; (d) At 10 weeks after the injury, the shade of tooth #21 had returned to normal.

Figure 3
(a) In case 3, tooth #11 showed yellowish brown discoloration; (b) The coronal pulp space was obliterated, whereas the pulp space was present in the root area. There was no radiolucency in the periapical area, but the root apex was slightly shortened; (c) In the ultrasound Doppler test, tooth #11 showed an image typical of a vital tooth; (d) The patient was satisfied with the shade of tooth #11 after vital bleaching treatment.
Acknowledgement
This case report is a part of the research that was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2011-0021235).
References
1. Yoon MJ, Kim E, Lee SJ, Bae YM, Kim S, Park SH. Pulpal blood flow measurement with ultrasound Doppler imaging. J Endod. 2010; 36:419–422.

2. Abd-Elmeguid A, Yu DC. Dental pulp neurophysiology: part 2. Current diagnostic tests to assess pulp vitality. J Can Dent Assoc. 2009; 75:139–143.
3. Ozçelik B, Kuraner T, Kendir B, Aşan E. Histopathological evaluation of the dental pulps in crown-fractured teeth. J Endod. 2000; 26:271–273.

4. Aguiló L, Gandía JL. Transient red discoloration: report of case. ASDC J Dent Child. 1998; 65:346–348. 356
5. Andreasen FM. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endod Dent Traumatol. 1989; 5:111–131.

6. Malmgren B, Hübel S. Transient discoloration of the coronal fragment in intra-alveolar root fractures. Dent Traumatol. 2012; 28:200–204.

7. Andreasen FM. Transient apical breakdown and its relation to color and sensibility changes after luxation injuries to teeth. Endod Dent Traumatol. 1986; 2:9–19.

8. Cohenca N, Karni S, Rotstein I. Transient apical breakdown following tooth luxation. Dent Traumatol. 2003; 19:289–291.

9. Cotti E, Campisi G, Ambu R, Dettori C. Ultrasound real-time imaging in the differential diagnosis of periapical lesions. Int Endod J. 2003; 36:556–563.

10. Rajendran N, Sundaresan B. Efficacy of ultrasound and color power Doppler as a monitoring tool in the healing of endodontic periapical lesions. J Endod. 2007; 33:181–186.

11. Lustig JP, London D, Dor BL, Yanko R. Ultrasound identification and quantitative measurement of blood supply to the anterior part of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 96:625–629.

12. Yoon MJ, Lee SJ, Kim E, Park SH. Doppler ultrasound to detect pulpal blood flow changes during local anaesthesia. Int Endod J. 2012; 45:83–87.

13. Cohen S, Hargreaves KM. Pathways of the pulp. 9th ed. Louis: Mosby;2006. p. 504–508.
14. Ehrmann EH. Pulp testers and pulp testing with particular reference to the use of dry ice. Aust Dent J. 1977; 22:272–279.

15. Klein H. Pulp responses to an electric pulp stimulator in the developing permanent anterior dentition. ASDC J Dent Child. 1978; 45:199–202.
16. Olgart L, Gazelius B, Lindh-Strömberg U. Laser Doppler flowmetry in assessing vitality in luxated permanent teeth. Int Endod J. 1988; 21:300–306.

17. Sasano T, Onodera D, Hashimoto K, Iikubo M, Satoh-Kuriwada S, Shoji N, Miyahara T. Possible application of transmitted laser light for the assessment of human pulp vitality. Part 2. Increased laser power for enhanced detection of pulpal blood flow. Dent Traumatol. 2005; 21:37–41.

18. Gopikrishna V, Tinagupta K, Kandaswamy D. Comparison of electrical, thermal, and pulse oximetry methods for assessing pulp vitality in recently traumatized teeth. J Endod. 2007; 33:531–535.

19. Gopikrishna V, Tinagupta K, Kandaswamy D. Evaluation of efficacy of a new custom-made pulse oximeter dental probe in comparison with the electrical and thermal tests for assessing pulp vitality. J Endod. 2007; 33:411–414.

20. Jafarzadeh H, Rosenberg PA. Pulse oximetry: review of a potential aid in endodontic diagnosis. J Endod. 2009; 35:329–333.

21. Heithersay GS, Hirsch RS. Tooth discoloration and resolution following a luxation injury: significance of blood pigment in dentin to laser Doppler flowmetry readings. Quintessence Int. 1993; 24:669–676.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download