Abstract
A tooth with primary endodontic disease that demonstrates a periodontal defect might be extracted because of misdiagnosis as severe periodontal disease or a vertical root fracture. The aim of this case report was to demonstrate the long-term survival of endodontically treated teeth, which had been initially considered unsavable. With meticulous evaluation including the patient's dental history, clinical and radiographic examinations, teeth with primary endodontic lesions could be differentiated and saved after proper root canal treatment. Pain history, vitality test, and radiographic examinations, as well as a general periodontal condition check with periodontal probing on an affected tooth, might be the key methods to differentiate endodontic pathosis from that of periodontal disease.
Diagnosis and treatment of teeth with endodontic and periodontal lesions could be challenging for clinicians.1-3 The endodontic-periodontal interrelationships are classified into 5 categories including primary endodontic lesions, primary endodontic lesions with secondary periodontic involvement, primary periodontic lesions, primary periodontic lesions with secondary endodontic involvement, and true combined lesions.1 Even though endodontic-periodontal relationships are well defined and categorized, it may still be confusing for clinicians to make a clear and proper diagnosis when inflammation exists in both the pulp and periodontal tissue. The pulp and periodontium closely communicate through the apical foramen, dentinal tubules, and accessory canals. Pulpal irritants can spread through those communications and affect the integrity of the periodontal structure.3-5
Root canal therapy on a tooth with a primary endodontic lesion is known to result in a good prognosis as long as proper endodontic treatment is completed.1,2 The quality of a root canal treatment on a molar can affect the periodontal condition thereafter.6 Primary endodontic lesions are often misdiagnosed as severe periodontal lesions or vertical root fractures, as the pattern of radiographic bone destruction is confusing. In addition, periodontal treatment such as curettage or a flap operation might be detrimental to the periodontal reattachment of a tooth with a primary endodontic lesion without periodontal involvement.2,7,8
Herein, endodontically treated cases are presented that had favorable outcomes but were initially planned to have extractions because of suspected severe periodontal bone loss or vertical root fracture.
A 67-year-old male patient visited our clinic for evaluation and further treatment of the left mandibular first molar (#36). His chief complaint was "my lower gum has been swollen." The patient's medical history was unremarkable. The patient had received a class II gold inlay restoration on that tooth several years ago. For the past month, he had felt a slight discomfort while chewing. A clinical examination revealed slight sensitivity to percussion and bite, 2 degrees of mobility, no response to cold, and a positive response to the electric pulp test. Gingival swelling, which was confined to the distal aspect of #36, was observed, and periodontal probing was within normal limits, except for the buccal and distal surfaces of the distal root. A periapical radiograph showed apical radiolucencies on both roots, and there was no alveolar bony support around the distal root (Figure 1a). The initial diagnosis of the tooth was partial or total necrosis of the pulp with an acute apical abscess. The possibility of root fracture was considered because of vertical bone loss, the large metallic restoration, and prior bite discomfort history. Endodontic treatment was considered as the first choice.
After an inferior alveolar nerve block, anesthesia was achieved using 2% lidocaine containing 1 : 100,000 epinephrine, and the gold inlay was removed. The tooth was isolated with a rubber dam, 4 orifices were located, and the working lengths were determined with an electronic apex locator (RootZX, Morita, Tokyo, Japan). Upon access opening, two mesial canals were vital, however, two distal canals were necrotic. No crack lines were detected in the access cavity. The canals were instrumented using Gates Glidden Drills, stainless steel hand K-files, ProTaper, and ProFile rotary files (Dentsply Maillefer, Ballaigues, Switzerland). All canals were enlarged to the size of a #35 file and continuously irrigated using 2.5% sodium hypochlorite (NaOCl). The canals were dried, and calcium hydroxide was applied as a medicament. No antibiotics were prescribed as the swelling was localized and there were no signs of fever. A week later, at the second visit, the patient was asymptomatic, and the gingival swelling had subsided. The canals were irrigated using 2.5% NaOCl. At the third visit, 2 weeks after the procedure, the patient was asymptomatic. Master gutta percha cones were placed, and periapical radiographs were taken to confirm the working lengths. The canals were obturated with the continuous wave technique using System B and Obtura II (Figure 1b). The patient was sent to a prosthodontist for further tooth restoration. During an 8-year follow up, the patient remained asymptomatic, and the periapical radiolucency disappeared (Figures 1c - 1f).
A 43-year-old female patient visited our clinic because of intermittent discomfort of her right mandibular teeth. She had visited 2 other dental clinics, and both dentists recommended extraction of her right mandibular first molar because they believed the mesial root might be vertically fractured. Based on her prior dental history, #46 was pulpotomized several years ago and had maintained asymptomatic until 2 months ago. The tooth was sensitive to percussion and bite. There was no mobility, and periodontal probing was within normal limits. Large periapical lesions in both roots and a J-shaped alveolar bone defect in the mesial root were observed in the periapical radiographs (Figures 2a and 2b). A cone-beam computed tomography (CBCT, Pax-Zenith3D, Vatech, Yongin, Korea, 104 kVp, 5.5 mA) was also performed to rule out a vertical root fracture (Figures 3a - 3d). The tooth was diagnosed as a previously initiated tooth with chronic apical periodontitis. The possibility of vertical root fracture was explained to the patient, but we believed a primary endodontic lesion without any fractures was possible, so nonsurgical endodontic therapy was suggested as the first option.
The gold crown and amalgam core were removed. There was no visible crack or fracture line found on the outer and inner access cavity walls. Conventional root canal treatment was performed using a protocol similar to that described in case 1. Three canals were found and enlarged to a 0.04 taper of the #35 Profile (Figure 2c). At the second visit, the patient was asymptomatic, and the canals were clean. The canals were obturated, and a composite resin core was built (Figure 2d). At a 3-month follow up (Figure 2e), the patient was asymptomatic and sent to the department of prosthodontics for a crown restoration. The tooth underwent routine check-ups and was asymptomatic through a 2-year follow up (Figures 2f - 2h).
A 50-year-old female patient was referred from a private dental clinic to our hospital for a proper diagnosis and treatment of the left mandibular second molar. Her chief complaint was gingival swelling around the tooth. A sinus tract was traced to the distal aspect of the distal root (Figures 4a and 4b). In the periapical radiographs, a toothlike fragment was observed where the sinus tract was traced. She had a surgical extraction of #38 6 months ago, and a class II gold restoration on #37 thereafter. Her prior dentist suspected a distal root fracture of #37. There was no response to cold or electric pulp test on #37. The tooth was not sensitive to percussion or bite tests. There was no abnormal mobility, and a periodontal probing test appeared normal except for apical full-depth probing on the distal root. The initial diagnosis of #37 was pulp necrosis with chronic apical abscess, and the existence of tooth remnants of #38 was also considered as a contributing factor. We decided on a nonsurgical endodontic treatment for the necrotized second molar. The patient was informed that the lesion would not respond to root canal therapy, so a surgical approach should be considered to remove the tooth fragment.
After removal of the gold onlay on #37, root canal treatment was initiated according to the above-mentioned protocol. Even after 3 canal preparations were completed up to #35 and copious 2.5% NaOCl irrigation was performed, the sinus tract on the distal side remained (Figures 4c and 4d). Surgical removal of the #38 fragment was decided. Computed tomography (CT, Somtom Sensation 64, Siemens, Erlangen, Germany, 120 kVp, 90 mA) was performed to evaluate the location of the fragments, which were observed on the distal proximity of #37 (Figures 4g and 4h). An oral surgeon expected that removal of tooth remnants might be difficult without excising a large amount of cortical bone. Therefore, an intentional replantation of #37 was planned, while the tooth fragments of #38 were retrieved from the extraction socket.
One week before surgery, an orthodontic elastic separating ring was inserted into the interdental space between #36 and #37 to increase the mobility of #37. The surgical procedure was performed as planned without any complications. The extracted #37 was retro-prepped and retro-filled with mineral trioxide aggregate (white ProRoot MTA, Dentsply Tulsa dental, Tulsa, OK, USA). While an endodontist worked with the extracted #37, an oral surgeon removed the tooth fragment from the extraction socket of #37 (Figures 4i and 4j). After placing the tooth back into the socket, there was no mobility, and no additional splinting was needed thereafter. Total tooth fragment removal was confirmed with periapical radiographs (Figure 4k). One week after surgery, the tooth was slightly mobile and sensitive to percussion. The patient was instructed to have a temporary resin crown for protection. However, when the patient visited our clinic for a 3-month follow up, the tooth remained asymptomatic, and the periapical radiolucency had decreased. The results of a periodontal pocket probing were within normal limits. The 1- and 2-year follow-up radiographs revealed a gradual decrease in radiolucency (Figures 4l - 4n).
There are several key factors known to be critical to diagnose an endodontic lesion.1,3,8,9 First, possible existence of endodontic irritants should be observed or at least, strongly suspected.1-3 Deep caries, secondary decay, old restoration, pulp necrosis, and prior or incomplete endodontic treatment can be clues for clinicians to consider the possibility of an endodontic origin. Second, the general periodontal condition of the other teeth should be checked. If there is no generalized periodontitis, the involved tooth might have endodontic pathosis, rather than a periodontal problem.1,3 The other considerations are mobility and pain characteristics. Other than during the acute abscess stage, teeth with an endodontic lesion tend to have normal mobility. Also, pain caused from endodontic lesions has been known to be more acute and severe.3 Moreover, meticulous periodontal probing to check the physical contours of attachment is suggested as a useful tool in differential diagnosis, a tooth with endodontic pathosis tends to have a narrow, deep pocket probing.7,8 In addition, teeth with primary periodontal pathosis tend to respond positively to vitality tests such as cold thermal test and electric pulp testing (EPT).1,2
Our first and second cases' conditions turned out to be primary endodontic lesions, without periodontal involvement. Preoperative periapical radiographs in both cases made the dentists suspect a vertical root fracture. In addition, periodontal full-pocket probing depths on the affected roots were also considered signs of root fractures. With the aid of a dental operative microscope, the access cavities were carefully examined, and the possibility of cracks originating from the coronal portion was eliminated. However, vertical root fractures frequently initiate from the apical portion. Therefore, the possibility of a vertical root fracture was in consideration. The initial suspicion of root fractures was eliminated after the initiation of root canal therapy because the previous symptoms including swelling disappeared after the initiation of root canal therapy, and cleanliness of the root canal system was maintained.
For case 2, CBCT was performed to diagnose a vertical root fracture, but no fracture lines were detected in the CBCT views. However, it was not possible to clearly rule out a vertical root fracture based on the radiographs.10,11 The use of CBCT might be beneficial if there is a deviation because of an existing long-term vertical root fracture. CBCT is considered a useful tool for the diagnosis of a vertical root fracture, but a hair-like crack may not be detected with CBCT.10 As for case 3, CT was utilized, instead of CBCT, because CBCT was not available in our institution at that time. CBCT might have been beneficial in this case because of the cost and radiation dose.
For cases 1 and 2, no periodontal treatment was performed during the endodontic procedure. A primary endodontic lesion does not need additional periodontal treatment such as curettage.7,8 Interestingly, both cases had rapid healing, confirmed by periapical radiographs. According to the 3-month follow-up radiographs, the prior radiolucency obviously decreased. Case 3 demonstrated a more complicated situation. On the basis of the past dental history, it was inferred that the tooth fragment of the third molar was not completely removed during extraction and that the fragment was connected to the apical lesion, which originated from the second molar. We postulated that the sinus tract might be persistent after root canal therapy because of the infected tooth remnants.
For case 3, an oral surgeon expected that it might be difficult to locate the tooth remnants because almost 6 months had passed, and the extraction socket was filled with bone. Instead of performing an osteotomy on the distal side of the second molar, a more conservative approach to extract the second molar was considered in order to remove the tooth fragment of the third molar through an extraction socket. However, the decision to perform an intentional replantation of the second molar had disadvantages because of the possible complications during extraction, such as possible tooth fracture during extraction and ankylosis. There was no initial mobility of the second molar, and an orthodontic elastic separation ring was inserted to increase tooth mobility to minimize harmful extraction forces on the tooth.12,13 When the second molar was extracted, calculus was observed on the furcation area of distal root, which was removed using a curette. During a preoperative examination, a sinus tract traced to the furcation area was noticed that might have been a coincidence, along the area of calculus deposition. Based on that finding, the tooth may have had a combined endodontic and periodontal problem. We inferred that the second molar had a pulp necrosis, which created a loss of periodontal attachment, and calculus deposited thereafter. Nevertheless, this hypothesis was not proven, as we did not review the patient's prior dental records.
A proper and meticulous diagnosis depends on discriminating a primary endodontic lesion from that of periodontal disease, a vertical root fracture, or both. For both teeth in cases 2 and 3, their dentists initially suggested an extraction because of severe periodontal defects, as well as possibilities of vertical root fractures. A comprehensive examination and careful interpretation of all possible information such as patient dental history, pain history, vitality test, mobility test, bite test, periodontal probing, and radiographic findings should be performed to save a tooth with a primary endodontic lesion.
Figures and Tables
Figure 1
A series of periapical radiographs of the mandibular left first molar of case 1. (a) A preoperative radiograph showed radiolucency around both the mesial and distal roots and a gutta percha cone traced to the apex of distal root; (b) A postoperative radiograph after obturation of 4 canals; (c) A periapical radiograph at a 1-year routine check-up; (d) A periapical radiograph at a 3-year routine check-up; (e) and (f) Periapical radiographs at an 8-year routine check-up.
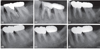
Figure 2
Periapical radiographs of case 2. (a) A preoperative periapical radiograph showed a J-shaped radiolucency on the mesial root of mandibular right first molar; (b) A preoperative radiograph with a different horizontal angle. The distal root also had a J-shaped lesion, which could be suspected of being a vertical root fracture; (c) A periapical radiograph for the working length determination; (d) A postoperative radiograph after canal filling; (e) A periapical radiograph at a 3-month routine check-up; (f) A periapical radiograph at a 6-month routine check-up; (g) A periapical radiograph at a 1-year routine check-up; (h) A periapical radiograph at a 2-year routine check-up.

Figure 3
Preoperative views of #46 of case 2 using cone-beam computed tomography (CBCT). (a) A coronal view of the mesial root and the surrounding bone of #46; (b) A coronal view of the distal root and the surrounding bone of #46; (c) A sagittal view of the mesial root and the surrounding bone of #46; (d) A sagittal view of the distal root and the surrounding bone of #46.

Figure 4
A series of periapical radiographs, computed tomographic (CT) views, and clinical photos of the mandibular left second molar of case 3. (a) A preoperative periapical radiograph of #37; (b) A preoperative radiograph of #37 with a gutta percha cone traced to the furcation area; (c) and (d) Periapical radiographs obtained at a second visit of the endodontic treatment of #37. A sinus tract formed and was traced to the distal surface of the tooth; (e) and (f) Postoperative radiographs of #37 after canal filling; (g) and (h) CT views from sagittal and axial planes demonstrated the tooth fragment of #38; (i) An extracted second molar for intentional replantation. Calculus deposition was noticed on the furcation of the distal root; (j) A tooth fragment of #38 was removed through an extraction socket of #37; (k) A postoperative radiograph after intentional replantation of #37; (l) A periapical radiograph at a 1-year routine check-up; (m) and (n) A periapical radiograph at a 2-year routine check-up.

Acknowledgement
Dr. JH Lim and Dr. JH Lee contributed equally to this case report and share first authorship. This study was supported by a Grant from the Korean Health Care Technology R&D Project, Ministry of Health, Welfare & Family affairs, Republic of Korea (A084458).
References
1. Simon JH, Glick DH, Frank AL. The relationship of endodontic-periodontic lesions. J Endod. 2013; 39:e41–e46.

2. Harrington GW. The perio-endo question: differential diagnosis. Dent Clin North Am. 1979; 23:673–690.
3. Chen SY, Wang HL, Glickman GN. The influence of endodontic treatment upon periodontal wound healing. J Clin Periodontol. 1997; 24:449–456.

4. Bergenholtz G. Interactions between pulpal and periodontal disease conditions: introduction. Endod Topics. 2006; 13:1–2.

5. Rotstein I, Simon JH. The endo-perio lesion: a critical appraisal of the disease condition. Endod Topics. 2006; 13:34–56.

6. Jansson LE, Ehnevid H. The influence of endodontic infection on periodontal status in mandibular molars. J Periodontol. 1998; 69:1392–1396.

7. Guldener PH. The relationship between periodontal and pulpal disease. Int Endod J. 1985; 18:41–54.

8. Harrington GW, Steiner DR, Ammons WF. The periodontal-endodontic controversy. Periodontol 2000. 2002; 30:123–130.

10. Tamse A. Vertical root fractures in endodontically treated teeth: diagnostic signs and clinical management. Endod Topics. 2006; 13:84–94.

11. Pitts DL, Natkin E. Diagnosis and treatment of vertical root fractures. J Endod. 1983; 9:338–346.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download