Abstract
Orthodontic extrusion is usually performed by means of a fixed orthodontic appliance that utilizes arch wire attached to adjacent teeth and transfers the desired force by elastic from the wire to the root. However, clinicians often encounter cases where the bonding required for tooth traction is not possible because the adjacent teeth have been restored with ceramic or veneer. The purpose of this case report is to describe a modified orthodontic extrusion appliance that is useful when conventional orthodontic treatment is not possible. The modified appliance was fabricated using an artificial tooth, clear plastic sheeting, and a braided fiber-reinforced composite strip that covered adjacent teeth without bonding. It satisfied the esthetic and functional needs of the patient and established the optimal biologic width.
When an anterior tooth is fractured at the level of the osseous crest due to severe dental caries or trauma, a clinician can be confronted with a dilemma in choosing the best treatment among the various options with respect to prognosis and esthetics.1,2 In such cases, surgical extraction followed by an implant restoration or fixed prostheses can be considered. On the other hand, the advantages of saving the fractured tooth include a simpler procedure, a conservative approach, achievement of the desired esthetic outcome by preservation of the alveolar bone, and a reduction in time-related cost.3
The ferrule effect over sound dentin for the fractured tooth can be achieved in several ways, including surgical extrusion, crown lengthening, and orthodontic extrusion. Among these treatment options, orthodontic extrusion is the most common treatment because of its simplicity, non-invasiveness, low incidence of relapse, better prognosis, and good esthetic outcome.4
Conventional orthodontic extrusion, first introduced by Heithersay, uses the adjacent teeth as the anchor for the traction force that occurs after attachment of the orthodontic device.5 However, a clinician can encounter a situation where such bonding is not available because the adjacent teeth have been restored with ceramics or veneers. Bonding to ceramics is possible, but the ceramic prostheses may chip or fracture and the bonding strength may not be sufficient to resist the force of traction.6
The purpose of this report is to describe a modified appliance for orthodontic extrusion of a fractured tooth in cases where a conventional orthodontic extrusion appliance application is not possible due to ceramic restorations of the adjacent teeth. This modified design should be developed so that it does not interrupt oral function and so that it concurrently satisfies the esthetic desires during the forced eruption period.
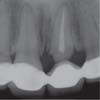
A 20-year-old woman presented to the Department of Advanced General Dentistry, Yonsei University, with chronic gingival swelling and bleeding on the left central incisor. A periapical radiograph of the left central incisor showed the level of tooth structure was approximately equal to the osseous crest and so was insufficient for restoration without invasion of the biologic width (Figure 1). Orthodontic forced eruption followed by single ceramic restoration treatment was determined on the basis of esthetic and economic considerations.
After careful bridge cutting and removal of the crown on the left central incisor (Figure 2), periodontal treatment was performed. A temporary crown with a post was set after the condition of the previous root canal treatment was evaluated by an endodontist. However, considering the adjacent ceramic crowns, conventional methods of forced eruption had an increased risk of ceramic damage. A modified appliance needed to be fabricated.
In the laboratory, an artificial tooth was set on the left central incisor area on the model and a clear appliance was fabricated using a plastic sheet (Bioplast, Scheu-Dental GmbH, Iserlohn, Germany) in the anterior teeth area. The artificial tooth was removed from the clear appliance and trimmed to leave only the labial shell. The labial shell of the artificial tooth was attached inside the clear appliance for esthetic maintenance. A window was formed on the palatal side of the left central incisor area of the clear appliance. A braided fiber-reinforced composite strip of 2 mm in diameter (Fiber Force, Synca, Le Gardeur, QC, Canada) was bonded to the inner surface of the window as a scaffold to increase the strength of the anchor (Figure 3). An elastic thread was engaged to the loop wire in the root and the horizontal bar of the clear appliance, and activated with a 50 g force after a piece of wire (0.032 inch in diameter) ending in a loop was affixed to the prepared root using glass ionomer cement (Figure 4). The occlusal interference due to the appliance was controlled by cutting the plastic sheet on the contact area of the centric stops. To avoid food impaction or foreign body entrapping, the window was covered with temporary filling material leaving the tooth space empty (Figures 5 and 6).
The amount of tooth movement was 1 mm after 1 week, and 2.5 mm after 2 weeks, and the necessary movement of the tooth (approximately 3.5 mm) to achieve the biologic width had been attained after 3 weeks (Figure 7). A two-month retaining period and gingivectomy was planned along with careful periodontal hygiene control, and a new ceramic crown was fabricated on the tooth in concern (Figure 8). The functionality and periodontal support of the restoration have been maintained in good condition for 2 years (Figure 9).
Orthodontic extrusion is one of the best conservative treatment options for compromised biologic width cases. This approach typically uses wires and orthodontic devices attached to the adjacent teeth.7 In the present case, a conventional orthodontic device could not be bonded because of the adjacent zirconia-ceramic prostheses, which were at risk of chipping and fracture, and which had low bonding strength to sustain traction force.8
Modifications of the extrusion appliance for compromised teeth with inadequate biologic width include removable appliances, such as the flipper type and the partial anterior occlusal splint using elastic threads for drawing the cast metal post and core with two supporting retentive rods, and fixed appliances including the clasp and rest types.9,10,11 These appliances do not need bonding to adjacent teeth, but may cause damage to adjacent teeth in the form of chipping or fracture, and do not satisfy esthetic needs. Another method is the use of a fiber-reinforced composite with bonding.12 This method is simple, esthetically pleasing and time-saving. But it needs adjacent natural teeth for bonding. Each of these reported modifications had limitations in its application to the present case with respect to esthetics, technique and cost.
In this case, a clear appliance over the adjacent teeth was used to establish an anchor of sufficient strength. The strength was reinforced by scaffolding using the fiber-reinforced composite. To improve the esthetics during the traction or retaining period, the labial shell of the artificial tooth was attached to the inner labial side of the clear appliance. A beam made in the fiber-reinforced composite, crossing over the space of the root rest between the two adjacent teeth, acted as the main anchor to draw the fractured tooth. The clear appliance could not be delivered without occlusal interference, which was controlled by removal of the area of centric stops by making a hollow in the plastic sheet. This appliance and technique incorporated some modifications and provided adequate esthetics, function, and stability.
When forced eruption is considered for a tooth that is structurally compromised due to trauma, the treatment option that is chosen depends on the conditions of periodontal support and of the adjacent teeth, the material of restoration, and so on. Therefore, a modified approach has been developed.
Figures and Tables
Figure 3
Palatal view of the braided fiber-reinforced composite strip bonded inside the clear appliance.

Figure 4
Elastic thread engaged between the loop wire of the root portion and the fiber-reinforced composite strip.

Acknowledgement
This study was supported by a faculty research grant from Yonsei University College of Dentistry for 2012 (No 6-2012-0126).
References
1. Aggarwal V, Logani A, Shah N. Complicated crown fractures - management and treatment options. Int Endod J. 2009; 42:740–753.

2. Garrett GB. Forced eruption in the treatment of transverse root fractures. J Am Dent Assoc. 1985; 111:270–272.

3. Simon JH. Root extrusion. Rationale and techniques. Dent Clin North Am. 1984; 28:909–921.
4. Ingber JS. Forced eruption. I. A method of treating isolated one and two wall infrabony osseous defects-rationale and case report. J Periodontol. 1974; 45:199–206.

5. Heithersay GS. Combined endodontic-orthodontic treatment of transverse root fractures in the region of the alveolar crest. Oral Surg Oral Med Oral Pathol. 1973; 36:404–415.

6. Ribeiro JG, Segalla JC, Perez F, Ribeiro JC, Moyses MR. Effect of ceramic surface treatment on the shear bond strength of a resin cement to different ceramic systems. Gen Dent. 2012; 60:e315–e320.
7. Ziskind D, Schmidt A, Hirschfeld Z. Forced eruption technique: rationale and clinical report. J Prosthet Dent. 1998; 79:246–248.

8. Emerich-Poplatek K, Sawicki L, Bodal M, Adamowicz-Klepalska B. Forced eruption after crown/root fracture with a simple and aesthetic method using the fractured crown. Dent Traumatol. 2005; 21:165–169.

9. Veis R, Salzer A, Christian J. Manual of appliance therapy for adults and children. Los Angeles, CA: Space Maintainers Laboratory;1994.
10. Felippe LA, Monteiro Junior S, Vieira LC, Araujo E. Reestablishing biologic width with forced eruption. Quintessence Int. 2003; 34:733–738.
11. Uddin M, Mosheshvili N, Segelnick SL. A new appliance for forced eruption. N Y State Dent J. 2006; 72:46–50.
12. Oshagh M, Sadeghi AR, Sharafeddin F, Alavi AA, Amid R, Derafshi R. Forced eruption by fiber-reinforced composite. Dent Today. 2009; 28:666870–71.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download