Abstract
Use of an apical plug in management of cases with open apices has gained popularity in recent years. Biodentine, a new calcium silicate-based material has recently been introduced as a dentine substitute, whenever original dentine is damaged. This case report describes single visit apexification in a maxillary central incisor with necrotic pulp and open apex using Biodentine as an apical barrier, and a synthetic collagen material as an internal matrix. Following canal cleaning and shaping, calcium hydroxide was placed as an intracanal medicament for 1 mon. This was followed by placement of small piece of absorbable collagen membrane beyond the root apex to serve as matrix. An apical plug of Biodentine of 5 mm thickness was placed against the matrix using pre-fitted hand pluggers. The remainder of canal was back-filled with thermoplasticized gutta-percha and access cavity was restored with composite resin followed by all-ceramic crown. One year follow-up revealed restored aesthetics and function, absence of clinical signs and symptoms, resolution of periapical rarefaction, and a thin layer of calcific tissue formed apical to the Biodentine barrier. The positive clinical outcome in this case is encouraging for the use of Biodentine as an apical plug in single visit apexification procedures.
The completion of root development and closure of the apex occurs up to 3 years following eruption of the tooth.1 When teeth with incomplete root formation undergo pulp necrosis due to trauma, caries or other pulpal pathosis, dentin formation is interrupted and root development ceases. Consequently, the root canal is wide, with thin and fragile walls, and the apex remains open. These features impair root canal instrumentation and prevent the achievement of an adequate apical stop. In order to allow condensation of the filling material and to promote apical sealing in such cases, it is imperative to create an artificial apical barrier or induce closure of the apical foramen with calcified tissue. Apexification is defined as 'a method to induce a calcified barrier in a root with an open apex or the continued apical development of an incomplete root in teeth with necrotic pulp'.2
Whilst several procedures utilizing different materials have been proposed to induce root end barrier formation, calcium hydroxide has gained the widest acceptance. Although this technique is efficient with predictable outcomes, it has several disadvantages.3 The disadvantages are the unpredictable time needed to form an apical barrier, the need for multiple visits, patient compliance, re-infection due to loss of temporary restoration, and also predisposition of the tooth to fracture.4,5,6 Another disadvantage of this technique is the nature of the barrier, which although apparently calcified, is actually porous and is sometimes even found to contain small amounts of soft tissue.7
Considering the various drawbacks associated with calcium hydroxide apexification, the use of apical plug method seems to be a suitable alternate treatment plan for such cases. In this method, a compact barrier is placed in the open area of the root-end to induce the formation of a calcified barricade in the periapical region. After setting of this barrier the remainder part of the canal is immediately obturated with gutta-percha. Advantages of this technique include shorter treatment time, and development of a good apical seal. A number of materials have been proposed for this purpose including tricalcium phosphate, freeze dried bone, freeze-dried dentin, collagen calcium phosphate, proplast (a polytetrafluor-ethylene and carbon felt-like porous material), and mineral trioxide aggregate (MTA).8,9,10,11,12,13
One of the technical problems associated with the placement of these materials is their extrusion into the periodontal tissue. The use of an artificial barrier or a matrix is advisable because its placement in the area of bone destruction provides a base on which the sealing material can be placed and packed. Several materials have been recommended to create a matrix, including calcium hydroxide, hydroxyapatite, absorbable collagen, calcium sulphate, and autologus platelet rich fibrin membrane.14,15,16,17
Of all the materials available, MTA has been widely used for one-visit apexification. It has attracted considerable attention owing to their superior sealing ability, biocompatibility, regenerative capabilities, and antibacterial properties.18,19 Nevertheless, MTA remains subject to some concerns, such as its long setting time, poor handling characteristics, low resistance to compression, low flow capacity, limited resistance to washout before setting, possibility of staining of tooth structure, presence and release of arsenic, and high cost.20,21 These disadvantages necessitate more ideal restorative materials, with adequate biological and mechanical properties. Recently, a new calcium silicate-based material, Biodentine (Septodont, Saint-Maur-des-Fossés, France), has been introduced with the intention of preserving the properties and clinical applications of MTA without its negative characteristics.
The aim of the present article is to report the successful closure of root apex in a pulpless permanent maxillary central incisor with wide open apex using Biodentine in combination with a synthetic collagen material as matrix.
A 20-year old male patient reported to the Department of Conservative Dentistry and Endodontics with a chief complaint of fractured and discoloured upper left front tooth. He gave a history of trauma 10 years back. The patient did not give any history of swelling or pus discharge. No other significant dental or medical history was found and no known drug allergies were noted. Intraoral examination revealed generalized dental fluorosis with Elli's Class IV fracture and discolouration in relation to tooth #21 (Figure 1a). Palpation and percussion test of the involved tooth did not reveal any tenderness. The tooth was not mobile and periodontal probing around the tooth was within physiological limits. Electric pulp testing (Parkell Electronics Division, Farmingdale, NY, USA) of the involved tooth gave no response, whereas response was obtained on adjacent teeth. The radiographic examination of the tooth revealed a wide canal with an open apex and a marked radiolucency periapically (Figure 2a). Clinical and radiographic examination indicated pulp necrosis with chronic apical periodontitis. The available treatment options were discussed with the patient and root canal therapy with calcium hydroxide dressing, followed by apexification with Biodentine using a matrix with synthetic collagen material was selected.
Following rubber dam isolation, a conventional endodontic access cavity was established. A dental operating microscope (Roslane Meditech, Haryana, India) was used to facilitate all endodontic procedures for this tooth. As the apex locator (Raypex5, VDW, Munich, Germany) produced inconsistent canal length readings, the working length was established radiographically 1 mm short of the radiographic apex with a #110 H-file (MANI, INC., Utsunomiya Tochigi, Japan) and was recorded for reference (Figure 2b). The canal was gently instrumented to #140 H-files using a circumferential filing motion with copious irrigation with 3% sodium hypochlorite solution (Cmident, Cmident, New Delhi, India). The canal was dried with sterile paper points, and calcium hydroxide paste (Metapex, Meta Biomed Co. Ltd., Chungwon, Korea) was placed as an intracanal medicament and the access cavity was temporized with a cotton pellet and Cavit G (3M ESPE Dental Products, St. Paul, MN, USA) (Figure 2c).
After 1 month, the tooth was again isolated under rubber dam and the calcium hydroxide was removed mechanically using hand H-files to the working length, while rinsing with alternating solutions of 3% sodium hypochlorite solution and 17% ethylenediaminetetraacetic acid (Prevest Denpro Ltd., Jammu, India). A final rinse with sterile saline was performed. After drying the canal with paper points, small piece of absorbable collagen membrane (CollaPlug, Zimmer Dental Inc., Carlsbad, CA, USA) was cut to fit the width of the canal. The membrane was introduced thorough the root canal and gently compacted using pre-fitted hand pluggers slightly beyond the apex into the bony space formed due to the periapical lesion in order to achieve a matrix.
Biodentine was mixed according to the manufacturer's instructions. It was carried into the canal with the help of an amalgam carrier and was condensed against the collagen matrix using pre-fitted hand pluggers. Several increments were required to form an apical plug of 5 mm thickness, which was confirmed radiographically (Figure 2d). Following the placement of Biodentine over the barrier, butt-end of a paper point was used to clear out any excess material from the walls. After 12 minutes, the hardness of the Biodentine was examined using a plugger to confirm its set. The canal was back-filled with injection-moulded thermoplasticized gutta-percha (Calamus Dual, Dentsply Maillefer, Bellaiguise, Switzerland) and AH Plus resin sealer (Dentsply DeTrey, Konstanz, Germany). The access cavity was then restored with composite resin (Ceram-X Duo, Dentsply DeTrey) (Figure 2e). In the subsequent visit, the teeth were bleached with a combination of in-office and at-home whitening protocols. Following bleaching, tooth #21 was restored with all-ceramic crown (Figure 1b).
One year postoperative follow-up revealed restored aesthetics and function, absence of any clinical signs or symptoms of periradicular pathosis, resolution of periapical rarefaction, and a thin layer of calcific tissue formed apical to the Biodentine barrier (Figure 2f).
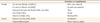
Biodentine has been developed as a permanent dentine substitute material whenever original dentine is damaged. The material with dentin-like mechanical properties can be used on both crowns and roots. Its clinical indications are summarised in Table 1.22,23 Biodentine consists of a powder in a capsule and liquid in a pipette. The highly purified powder is manufactured in a laboratory using the sol-gel method. The powder mainly consists of tricalcium silicate and dicalcium silicate- the principal component of Portland cement and MTA. In addition, the powder also contains calcium carbonate, calcium oxide, iron oxide, and zirconium oxide. The liquid for mixing with the cement powder consists of calcium chloride and a water-soluble polymer. Tricalcium silicate and dicalcium silicate are the main component of the powder and they regulate the setting reaction. Calcium carbonate and calcium oxide are incorporated for both biocompatibility and calcium content.24 They act as fillers, improving the mechanical properties of the cement.22 In addition, as an active agent, calcium carbonate is implicated in the process of hydration.24 Iron oxide is added to impart shade to the cement. While as, zirconium dioxide serves as a radiopacifier. Calcium chloride present in the liquid accelerates the setting reaction and improves the physicochemical properties of the set cement. The hydrosoluble polymer is based on polycarboxylate and it reduces the amount of water required by the mix, while maintaining the consistency of the mixture (Table 2).22
The ability of calcium silicate to interact with water leads to the setting and hardening of the cement.22,25 The powder is mixed with 5 drops of liquid in a capsule and triturated for 30 seconds.22 Tricalcium silicate mixes with the water component and leads to the formation of a hydrated calcium silicate gel and calcium hydroxide. This dissolution process occurs at the surface of each grain of calcium silicate. The hydrated calcium silicate gel and the excess of calcium hydroxide tend to precipitate at the surface of the particles and in the pores of the powder.22,25 Nucleation and growth of the gel structure gradually fills the spaces in between the tricalcium silicate grains.26 Crystallisation of the calcium silicate gel structure occurs through continuous hydration with unreacted tricalcium silicate grains surrounded by layers of hydrated calcium silicate gel and crystals of calcium carbonate filling the spaces between the grains of cement. This process of crystallisation makes the structure relatively impermeable to water and slows down the effects of further reactions.22,25
The mix has a putty-like consistency which reminds that of phosphate cement. Biodentine has a shorter setting time of 12 minutes as compared to that of MTA which is 2 hours 45 minutes.18,22 This reduction in setting time is reported to have been achieved by higher specific surface size of particles, addition of calcium chloride accelerator to liquid phase, and decrease in the liquid content.22 In case of apexification, quicker setting time eliminates the need for two step obturation as with MTA, and reduces the risk of bacterial contamination.27
The marginal sealing ability of calcium silicate-based materials is attributed to its ability to produce surface apatite crystals when in contact with the phosphates available in tissue fluids. The crystalline precipitates are formed through interaction of calcium and hydroxyl ions released from set material with phosphates.28 The apatite crystals formed have been identified as calcium-deficient B-type carbonated apatite precipitates produced via an amorphous calcium phosphate phase.29 Biodentine shows apatite formation after immersion in phosphate solution, indicative of its bioactivity.30 Dentine may uptake several elements released from bioactive materials, and such a phenomenon may cause chemical and structural modification in dentine. Han and Okiji compared calcium and silicon uptake by adjacent root canal dentine in the presence of phosphate buffered saline using Biodentine and ProRoot MTA. The results showed that both materials formed a tag-like structure composed of the material itself or calcium- or phosphate rich crystalline deposits. The thickness of the calcium and silicon -rich layers increased over time, and the thickness of the calcium and silicon -rich layer was significantly larger in Biodentine compared to MTA after 30 and 90 days, concluding that the dentine element uptake was greater for Biodentine than for MTA. These findings lead to the notion that apatite formation contributes to leakage reduction not only by filling the gap along the interface but also via dentine interactions such as intrafibrillar apatite deposition.31
Placement of Biodentine as apical plug is technique-sensitive. Restricting the material to the confines of the root apex is crucial. Sealing material extruded periapically may set before it disintegrates and gets resorbed. This might result in the persistence of the inflammatory process, which may complicate or even prevent repair of the tissue.32 To overcome such problems, Lemon in 1992 introduced the 'internal matrix concept' for treatment of root perforations. He recommended the use of amalgam for sealing the perforation, which would be condensed against an external matrix of hydroxyapatite, carefully pushed through the perforation thus serving as an external barrier or matrix.14 Alternate use of a sterile absorbable collagen membrane as an external matrix has been advocated to reconstruct the outer shape of root and facilitate the adaptation of the sealing material. This material absorbs moisture and expands and also has a haemostatic effect.15 The collagen membrane fully absorbs within 10 to 14 days allowing new bone to gradually fill the defect.
Deliberate overinstrumentation of the periapical area to produce a blood clot that will induce apical closure has also been described as an alternative treatment in some cases of incomplete root formation.33 Although pulp revascularization remains a good treatment option for such cases, the patient was not agreeable due to the time constraint. So, one step apexification with Biodentine was selected for this case.
Biodentine represents a great improvement compared to the other calcium silicate dental materials. In contrast with MTA, the mechanical properties of Biodentine are similar to those of natural dentine. The compressive strength, elasticity modulus and microhardness are comparable with that of natural dentine. The material is stable, less soluble, non-resorbable, hydrophilic, easy to prepare and place, needs much less time for setting, produces a tighter seal and has greater radiopacity.22,26 Due to its improved material properties, Biodentine has a distinct advantage over its closest alternatives in treatment of teeth with open apex.
Figures and Tables
Figure 1
(a) Preoperative photograph showing Elli's Class IV fracture and discolouration in relation to 21; (b) Postoperative photograph showing tooth restored with an all-ceramic crown.

Figure 2
(a) Preoperative radiograph showing tooth 21 with open apices and periapical radiolucency; (b) Working length radiograph; (c) Calcium hydroxide as intracanal medicament; (d) Radiograph confirming the placement of Biodentine apical plug compacted against the barrier material; (e) Backfill performed using thermoplasticized gutta-percha; (f) One year follow-up radiograph showing resolution of periapical rarefaction and a thin layer of calcific tissue formed apical to the Biodentine barrier.

References
1. Bhasker SN. Orban's oral histology and embryology. 11th ed. St. Louis: Mosby-Year Book;1991. p. 382.
2. American Association of Endodontists: Glossary of endodontic terms. updated 2013 Nov 6. Available from: http://www.aae.org/glossary.
3. Sheehy EC, Roberts GJ. Use of calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: a review. Br Dent J. 1997; 183:241–246.

4. Felippe MC, Felippe WT, Marques MM, Antoniazzi JH. The effect of renewal of calcium hydroxide paste on the apexification and periapical healing of teeth with incomplete root formation. Int Endod J. 2005; 38:436–442.

5. Metzger Z, Solomonov M, Mass E. Calcium hydroxide retention in wide root canals with flaring apices. Dent Traumatol. 2001; 17:86–92.

6. Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002; 18:134–137.

7. Binnie WH, Rowe AH. A histological study of periapical tissues of incompletely formed pulpless teeth filled with calcium hydroxide. J Dent Res. 1973; 52:1110–1116.

8. Roberts SC Jr, Brilliant JD. Tricalcium phosphate as an adjunct to apical closure in pulpless permanent teeth. J Endod. 1975; 1:263–269.

9. Rossmeisl R, Reader A, Melfi R, Marquard J. A study of freeze-dried (lyophilized) cortical bone used as an apical barrier in adult monkey teeth. J Endod. 1982; 8:219–226.

10. Rossmeisl R, Reader A, Melfi R, Marquard J. A study of freeze-dried (lyophilized) dentin used as an apical barrier in adult monkey teeth. Oral Surg Oral Med Oral Pathol. 1982; 53:303–310.

11. Nevins A, Finkelstein F, Laporta R, Borden BG. Induction of hard tissue into pulpless open-apex teeth using collagen-calcium phosphate gel. J Endod. 1978; 4:76–81.

12. Eleazer PD, McDonald TW, Sinai IH, Fantasia JE, Michelich RJ, Yagiela JA. Proplast as an apical barrier in root canal therapy. J Endod. 1984; 10:487–490.

13. Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999; 25:197–205.

14. Lemon RR. Nonsurgical repair of perforation defects. Internal matrix concept. Dent Clin North Am. 1992; 36:439–457.
15. Bargholz C. Perforation repair with mineral trioxide aggregate: a modified matrix concept. Int Endod J. 2005; 38:59–69.

16. Mesimeris V, Sade E, Baer PN. Calcium sulfate as a biodegradable barrier membrane: a preliminary report on the "Surgiplast" technique. Periodontal Clin Investig. 1995; 17:13–16.
17. Rudagi KB, Rudagi B. One-step apexification in immature tooth using grey mineral trioxide aggregate as an apical barrier and autologus platelet rich fibrin membrane as an internal matrix. J Conserv Dent. 2012; 15:196–199.

18. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review - Part I: chemical, physical, and antibacterial properties. J Endod. 2010; 36:16–27.

19. Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review - Part II: leakage and biocompatibility investigations. J Endod. 2010; 36:190–202.

20. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review - Part III: clinical applications, drawbacks, and mechanism of action. J Endod. 2010; 36:400–413.

21. Chang SW. Chemical characteristics of mineral trioxide aggregate and its hydration reaction. Restor Dent Endod. 2012; 37:188–193.

22. Septodont. Biodentine - Active Biosilicate Technology, scientific file. Saint-Maur-des-Fossés Cedex, France: R&D Department, Septodont;2010.
23. Villat C, Grosgogeat B, Seux D, Farge P. Conservative approach of a symptomatic carious immature permanent tooth using a tricalcium silicate cement (Biodentine): a case report. Restor Dent Endod. 2013; 38:258–262.

24. Garrault S, Behr T, Nonat A. Formation of the C-S-H Layer during early hydration of tricalcium silicate grains with different sizes. J phys chem B. 2006; 110:270–275.

25. Pradelle-Plasse N, Tran XV, Colon P. VI-2-1. Physico chemical properties. In : Goldberg M, editor. Biocompatibility or cytotoxic effects of dental composites. Oxford: Coxmoor Publishing Co.;2009. p. 184–194.
26. Bachoo IK, Seymour D, Brunton P. A biocompatible and bioactive replacement for dentine: is this a reality? The properties and uses of a novel calcium-based cement. Br Dent J. 2013; 214:E5.

27. Bachoo IK, Seymour D, Brunton P. Clinical case reports using a novel calcium-based cement. Br Dent J. 2013; 214:61–64.

28. Camilleri J. Characterization of hydration products of mineral trioxide aggregate. Int Endod J. 2008; 41:408–417.

29. Tay FR, Pashley DH, Rueggeberg FA, Loushine RJ, Weller RN. Calcium phosphate phase transformation produced by the interaction of the portland cement component of white mineral trioxide aggregate with a phosphatecontaining fluid. J Endod. 2007; 33:1347–1351.

30. Goldberg M. Chapter VI. Emerging trends in (bio)material researches. Biocompatibility or cytotoxic effects of dental composites. Oxford: Coxmoor Publishing Co.;2009. p. 181–203.
31. Han L, Okiji T. Uptake of calcium and silicon released from calcium silicate-based endodontic materials into root canal dentine. Int Endod J. 2011; 44:1081–1087.

32. Benenati FW, Roane JB, Biggs JT, Simon JH. Recall evaluation of iatrogenic root perforations repaired with amalgam and gutta-percha. J Endod. 1986; 12:161–166.

33. Thibodeau B, Trope M. Pulp revascularization of a necrotic infected immature permanent tooth: case report and review of the literature. Pediatr Dent. 2007; 29:47–50.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download