Abstract
Apical surgery cuts off the apical root and the crown-to-root ratio becomes unfavorable. Crown-to-root ratio has been applied to periodontally compromised teeth. Apical root resection is a different matter from periodontal bone loss. The purpose of this paper is to review the validity of crown-to-root ratio in the apically resected teeth. Most roots have conical shape and the root surface area of coronal part is wider than apical part of the same length. Therefore loss of alveolar bone support from apical resection is much less than its linear length.The maximum stress from mastication concentrates on the cervical area and the minimum stress was found on the apical 1/3 area. Therefore apical root resection is not so harmful as periodontal bone loss. Osteotomy for apical resection reduces longitudinal width of the buccal bone and increases the risk of endo-perio communication which leads to failure. Endodontic microsurgery is able to realize 0 degree or shallow bevel and precise length of root resection, and minimize the longitudinal width of osteotomy. The crown-to-root ratio is not valid in evaluating the prosthodontic prognosis of the apically resected teeth. Accurate execution of endodontic microsurgery to preserve the buccal bone is essential to avoid endo-perio communication.
Abutment evaluation is mandatory before any dental treatments although we are often unaware of its significance on favorable abutment teeth. There are many predictors for abutment longevity such as mobility, alveolar bone support, root configuration, opposing occlusion, pulpal condition and remaining tooth structure.1-5 Assessment of abutment is a comprehensive process which considers these predictors integrally. Among them alveolar bone support is the most important factor to predict prosthodontic prognosis of a tooth and has been properly evaluated by crown-to-root ratio.6-9 Many studies about the prosthodontic impact of the crown-to-root ratio investigated periodontally compromised teeth, because the most common cause of increased crown-to-root ratio was periodontitis.10-13 The crown-to-root ratio has been popularly used to evaluate the teeth with periodontal bone loss as a prosthodontic abutment.14
Apical surgery is a promising procedure to resolve periapical pathosis that are related to a periapical cyst, a complex canal anatomy, extraradicular infection, an inadequate healing after nonsurgical retreatment and its success rate is very high with microsurgical instrument and technique.15,16 One of a few demerits of apical surgery is the fact that it cuts off the apical part of root and shortens the root portion. Therefore, the crown-to-root ratio of the tooth becomes more unfavorable.
For the tooth with periapical pathosis problem only, its crown-to-root ratio is not a matter of concern. But we sometimes encounter teeth where the crown-to-root ratio is expected to be questionable or poor after apical surgery, such as teeth with short roots or teeth that need large resections due to perforations, resorptions and the other problems (Figures 1a - 1d). The teeth in Figures 1a - 1c showed apical root resorption due to trauma and inflammation. The Figure 1d shows the tooth with a shortened root due to root fracture. In this situation we used to consider crown-to-root ratio of the teeth for prosthodontic evaluation and obviously these teeth are going to show very poor crown-to-root ratio after apical surgery. Therefore it is reasonable that we expect poor prognosis of these cases.
Apical root resection is a different matter from periodontal bone loss notwithstanding the fact that both increase crown-to-root ratio. Is it appropriate to evaluate apically resected teeth with the standard of crown-to-root ratio for periodontally compromised teeth? The purpose of this study is to review the validity of the standard of crown-to-root ratio in the apically resected teeth.
Crown-to-root ratio is calculated from only 1-dimensional linear measurements and is not directly proportional to 3-dimensional alveolar bone support. Total supported root surface area is more appropriate parameter to evaluate alveolar bone support.17 Ante's law is calculated based on periodontal membrane area of abutment teeth so very similar to total supported root surface.18 In Leempoel's study, 1451 bridges constructed according to Ante's law showed significantly higher survival rate than 223 bridges that did not meet this law.19 On the contrary, Fayyad and Al-Rafee showed that 57% of bridges did not meet the Ante's law but all bridges had functioned properly for 8 - 11 years.20
Most roots have conical shape and the root surface area of the coronal part is wider than the apical part of the same length. Root surface area of coronal half occupies 61.5% and apical half 38.5% of total root surface area.21 Supposing a tooth with the root of 14 mm length as an example, the root surface area of coronal 3 mm is eight times wider than that of apical 3 mm. Moreover, molars have root trunk portion which shows wider surface area than just conical root portion. Root trunk area averaged 32% of the total root surface area of Maxillary first molar and was greater than the root surface area of palatal root.22 On these teeth loss of apical root is less significant for alveolar bone support.
Loss of alveolar bone support from apical resection is much less compared to the loss of its linear length.
Masticatory forces are transmitted to the tooth and the degree of the stresses of the tooth varies according the site of the teeth. Dejak et al. analyzed stress distribution of tooth under mastication using finite element analysis.23 He created 2-dimensional tooth model and simulated chewing 4 morsels with different elastic moduli. And values of stresses were calculated during simulation. The result was that the maximum stresses were shown on the cervical area from 18.5 - 87.3 MPa and the minimum stresses were found on the apical 1/3 area below 1/10 of maximum stresses in all the simulations.23 Many studies of dental implant show similar tendency to stress distribution on natural teeth. The stress on coronal thread was the highest and gradually decreased to apical thread.24,25 The dental implants with 3.3 (diameter) × 8.5 (length) and 3.3 (diameter) × 15.0 (length) showed very similar stress curve. That means apical portion of long implant does not contribute to abutment support.24
Cervical bone support is the most important to sustain the stresses from occlusal load. Therefore periodontal bone loss is detrimental to prognosis of abutment tooth. On the contrary, apical root resection is not so harmful as periodontal bone loss because its contribution to bone support was originally low.
Horizontal root fracture is very similar to apical root resection because the apical part of the fractured root does not contribute to support the tooth. Cvek et al. reported the prognosis of teeth with intra-alveolar root fracture.26 He investigated 285 teeth with horizontal root fracture at middle 1/3. Among them 249 teeth survived and 36 teeth failed. The twenty three teeth were extracted within 50 days due to failure of initial stabilization and 13 teeth were extracted due to endodontic failure.26 Interesting point is that no teeth failed due to the loosening of coronal fragment. Considering the quite long-term follow up period of this study (mean = 65 months), coronal root portion is thought to be sufficient to support the tooth (Figure 2).
Apical root resorption occurring during orthodontic treatment results in shortened root similar to apical resection. It is a fearful situation to orthodontists but actually does not seriously jeopardize the longevity of the tooth. One long-term clinical study which observed 100 patients for average 14.1 years found that even severely resorbed teeth were functioning in a reasonable manner with hypermobility observed in only two patients.27 The reason for this result can be explained by Kalkwarf's study using computer-aided calculation of remaining periodontal attachment area of virtually resorbed root, in which approximately 3 mm of loss of apical support had been found to be equivalent to 1 mm of crestal bone loss (Figure 3).28
Osteotomy for apical resection reduces longitudinal width of the buccal bone plate and therefore increases the risk of endo-perio communication which leads to failure (Figure 4). This is a critical point to predict the prognosis of apical surgery. Consequently we should preserve the buccal bone plate as much as possible. Resection of the correct length of apical root with minimum bevel is essential. And it is a more crucial factor in Korean population than in western population because tooth lengths in Koreans are shorter than Caucasians.29 Contemporary endodontic microsurgery is able to realize 0 degree or shallow bevel and precise length of root resection and therefore minimize the longitudinal width of osteotomy and the risk of endo-perio communication due to buccal bone loss.
Apical root resection does not reduce the periodontal bone support as much as the loss of the crown-to-root ratio, and therefore the standard of crown-to-root ratio should be re-visited in evaluating the prosthodontic prognosis of the apically resected teeth (Figure 5). Because loss of total supported root surface due to apical resection is minimal and occlusal stress concentrate on the cervical area, not apical area. But, decreasing the longitudinal distance between alveolar bone margin and resected root end can increase the risk of endo-perio communication. Therefore, the evaluation of the marginal bone and the attached gingiva and accurate execution of endodontic microsurgery are the essentials for the preservation of the buccal bone.
Figures and Tables
Figure 1
Pre-operative radiographs of 4 cases in which crown-to-root ratios were expected to be poor after apical surgery. (a) The patient was referred from a local clinic for apical surgery of tooth #11 due to failure of negotiation in 2008. The tooth had a history of trauma in 2000 and showed 4 to 6 mm apical root resorption; (b) Non-surgical root canal treatment of #21 was incompletely finished due to canal calcification. Two months later sinus tract recurred and the tooth was planned to take apical surgery. The apical root was shortened due to inflammation; (c) The patient was referred from the department of pediatric dentistry for increased apical lesion of tooth #12. The tooth had a history of intrusive luxation in 2000 and received non-surgical root canal treatment in 2001. Apical root resorption with apical lesion was observed and lateral perforation was suspected; (d) The patient was referred from a local clinic for proper treatment of tooth #12 in 2002. Horizontal root fracture was seen and apical surgery with removal of the fractured apical root was planned.

Figure 2
6-year follow up case of horizontal root fracture. (a) Horizontal root fractures were found on teeth #11 and #21 at the first visit in 2006; (b) The tooth #11 became necrotic and received non-surgical root canal therapy in 2007; (c) 3-year follow up radiograph in 2009; (d) 6-year follow up radiograph in 2012.

Figure 3
8-year follow up case of apical root resorption due to orthodontic treatment. (a) Radiograph before orthodontic treatment in 2004; (b) Radiograph just after orthodontic treatment in 2006; (c) 5-year follow up radiograph; (d) 8-year follow up radiograph.

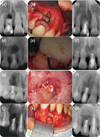
Figure 4
Failure case due to endo-perio communication. (a) Pre-operative radiograph showing apical lesion of mesial root and furcation bone loss on tooth #36; (b) Clinical photo after apical root resection showing very narrow buccal bone plate due to furcation bone loss and osteotomy for apical surgery; (c) Post-operative radiograph; (d) 3-month follow up radiograph showing increased apical to furcal bone loss; (e) 5-month follow up radiograph showing complete bone loss of apex to furcation.

Figure 5
Post-operative radiographs and clinical photos during surgery of 4 cases in Figure 1. (a), (d), (g), and (j), post-operative radiograph of each case; (b), (e), (h), and (k), clinical photos during apical surgery, showing narrow but intact buccal marginal bone; (c), (f), (i), and (l), 4, 9, 9 and 10-year follow-up radiographs after surgery, showing complete healing of apical lesion.
References
2. Nyman SR, Lang NP. Tooth mobility and the biological rationale for splinting teeth. Periodontol 2000. 1994; 4:15–22.

3. Nyman S, Lindhe J, Lundgren D. The role of occlusion for the stability of fixed bridges in patients with reduced periodontal tissue support. J Clin Periodontol. 1975; 2:53–66.

4. Sorensen JA, Martinoff JT. Endodontically treated teeth as abutments. J Prosthet Dent. 1985; 53:631–636.

5. Goodacre CJ, Spolnik KJ. The prosthodontic management of endodontically treated teeth: a literature review. Part I. Success and failure data, treatment concepts. J Prosthodont. 1994; 3:243–250.

6. Shillingburg HT. Fundamentals of fixed prosthodontics. 3rd ed. Chicago: Quintessence Pub. Co.;1997.
7. Rosenstiel SF, Land MF, Fujimoto J. Contemporary fixed prosthodontics. 4th ed. St. Louis, MO: Mosby Elsevier;2006.
8. Johnston JF, Dykema RW, Goodacre CJ, Phillips RW. Johnston's Modern practice in fixed prosthodontics. 4th ed. Philadelphia, PA: Saunders;1986.
9. Carr AB, McGivney GP, Brown DT. McCracken's removable partial prosthodontics. 5th ed. St. Louis, MO: Mosby Elsevier;2005.
10. Penny RE, Kraal JH. Crown-to-root ratio: its significance in restorative dentistry. J Prosthet Dent. 1979; 42:34–38.

11. McGuire MK. Prognosis versus actual outcome: a long-term survey of 100 treated periodontal patients under maintenance care. J Periodontol. 1991; 62:51–58.

12. McGuire MK, Nunn ME. Prognosis versus actual outcome. III. The effectiveness of clinical parameters in accurately predicting tooth survival. J Periodontol. 1996; 67:666–674.

13. Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of Periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012; 91:914–920.

14. Grossmann Y, Sadan A. The prosthodontic concept of crown-to-root ratio: a review of the literature. J Prosthet Dent. 2005; 93:559–562.

15. Kim E, Song JS, Jung IY, Lee SJ, Kim S. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod. 2008; 34:546–551.

16. Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature-part 1: Comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 2010; 36:1757–1765.

17. Jepsen A. Root surface measurement and a method for x-ray determination of root surface area. Acta Odontol Scand. 1963; 21:35–46.

18. Ante IH. The fundamental principles of abutments. Bull Mich State Dent Soc. 1926; 8:232–257.
19. Leempoel PJ, Käyser AF, Van Rossum GM, De Haan AF. The survival rate of bridges. A study of 1674 bridges in 40 Dutch general practices. J Oral Rehabil. 1995; 22:327–330.

20. Fayyad MA, Al-Rafee MA. Failure of dental bridges. IV. Effect of supporting periodontal ligament. J Oral Rehabil. 1997; 24:401–403.

21. Levy AR, Wright WH. The relationship between attachment height and attachment area of teeth using a digitizer and a digital computer. J Periodontol. 1978; 49:483–485.

22. Hermann DW, Gher ME Jr, Dunlap RM, Pelleu GB Jr. The potential attachment area of the maxillary first molar. J Periodontol. 1983; 54:431–434.

23. Dejak B, Mlotkowski A, Romanowicz M. Finite element analysis of stresses in molars during clenching and mastication. J Prosthet Dent. 2003; 90:591–597.

24. Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent. 2010; 30:89–95.
25. Himmlová L, Dostálová T, Kácovský A, Konvicková S. Influence of implant length and diameter on stress distribution: a finite element analysis. J Prosthet Dent. 2004; 91:20–25.

26. Cvek M, Tsilingaridis G, Andreasen JO. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7-17 years. Dent Traumatol. 2008; 24:379–387.

27. Remington DN, Joondeph DR, Artun J, Riedel RA, Chapko MK. Long-term evaluation of root resorption occurring during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989; 96:43–46.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download