Abstract
The autogenous tooth transplantation is an alternative treatment replacing a missing tooth when a suitable donor tooth is available. It is also a successful treatment option to save significant amount of time and cost comparing implants or conventional prosthetics. These cases, which required single tooth extraction due to deep caries and severe periodontal disease, could have good results by transplanting non-functional but sound donor tooth to the extraction site.
Autogenous tooth transplantation or autotransplantation is a surgical movement of a tooth from its original location to another site in the mouth within the same person.1 It can be applied in cases like traumatic tooth loss, impacted or ectopic positioned teeth, congenitally missing tooth, large endodontic lesions, and localized severe periodontitis which does not show promising prognosis.2
Autotransplantation is an alternative to dental implant or it is better than implant treatment, because it can save time, provide faster healing, function, and esthetic advantages. Moreover, it also have advantages of maintaining unique sensory system and promoting proper healing of the periodontal environment to sound tissue.3
However, several complications, such as root resorption, ankylosis, loss of the autotransplanted tooth, or fracture during the extraction, can be occurred.4,5 Especially, insufficient nutrition to the root surface of an autotransplanted tooth could be an explanation for the high rates of root resorption or loss of tooth transplant.6
The purpose of this article was to report two cases of successful autotransplantation for replacing lost teeth. The first case is transplantation of the third molar to periodontally healthy socket. The second case is transplantation of the second molar to periodontally involved socket.
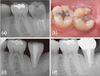
A 28 year old male visited the Department of Conservative Dentistry at Chonnam National University Dental Hospital for treatment of mandibular left second molar. The patient complained no clinical symptoms and had a normal periodontal pocket depth. However, the clinical and radiographic examination revealed that the mandibular left second molar was severely decayed. A single implant installation after extraction was one of the treatment options. However, considering the opinion of the patient and other oral environments, autotransplantation of maxillary right third molar was decided (Figures 1, 2a, and 2b).
A duplicated tooth model was fabricated with resin using computerized tomography (CT) image of the maxillary right third molar. Cone-bean CT scans of maxillary right third molar had been acquired using Mercuray (Hitachi, Tokyo, Japan) with 120 kV and 150 mAs. Under local anesthesia using 2% lidocaine with 1:100,000 epinephrine, the carious mandibular left second molar was extracted. The duplicated tooth model fitting the recipient site was used. The recipient site was prepared with a round bur under copious sterile saline irrigation. The maxillary right third molar was then carefully extracted with forceps. Root end resection and retrograde filling with ProRoot MTA (MTA, Dentsply Tulsa, Tulsa, OK, USA) was performed on the donor tooth to prevent endodontic complications. After fitting of the maxillary right third molar into the prepared recipient site, it was stabilized with 4-0 silk sutures and a semi-rigid resin wire splint. The extra-oral time from extraction of the maxillary right third molar to transplantation was 10 minutes. Amoxicillin 500 mg three times a day and Ibuprofen 400 mg three times a day were prescribed for a week, and a 0.1% chlorhexidine rinse was used for 7 days.
Stich-out was done after 1 week. The root canal therapy was started at 4 weeks. After the calcium hydroxide dressing was maintained for 2 weeks, root canal therapy completed with thermoplasticized gutta-percha and AH Plus sealer (Dentsply De Trey GmbH, Konstanz, Germany) at 6 weeks (Figure 2c). All endodontic procedures were carried out under a rubber dam and a strict aseptic condition. At the 6 month follow up, the transplanted tooth was asymptomatic and periodontally healthy. In addition, new bone formation on the mesial side of the tooth was observed and periodontal pocket depth is normal. After confirming such condition, the tooth was restored with a full crown (Figure 2d).
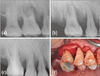
A 43 year old male visited the clinic complaining about the discomfort and pain in the upper right molar area while biting. The clinical and radiographic examination revealed that the maxillary right second premolar and the maxillary right first molar were both associated with localized severe chronic periodontitis. In contrast, the maxillary right second molar had healthy condition without an opposing tooth (Figures 3 and 4a). Considering the financial difficulty of the patient, autotransplantation was preferred to implant installation. Following consultation with a periodontist, the maxillary right second molar was planned to be transplanted to maxillary right first molar space and periodontal treatment was planned after that.
Scaling and root planning was performed at 1 month before autotransplantation. Due to the trismus of the patient, root canal therapy was performed after the surgery. Surgical procedure was similar to that described for case 1. Under local anesthesia, the maxillary right first molar was extracted. The recipient site was prepared with a round bur and a duplicated tooth model. The maxillary right second molar was extracted and immediately placed into the recipient site. It was stabilized with 4-0 silk sutures and a semi-rigid resin wire splint (Figure 4b). The extra-oral time from extraction of the maxillary right second molar to transplantation was 11 minutes. Amoxicillin 500 mg three times a day and Ibuprofen 400 mg three times a day were prescribed for a week, and a 0.1% chlorhexidine rinse was used for 7 days.
The root canal therapy was begun 2 weeks later. After the calcium hydroxide dressing was maintained for 2 weeks, root canal therapy was completed at 4 weeks after the surgery.
At the 7 month follow up, there was no clinical symptom or radiographic signs of root resorption (Figure 4c). As planned, the regenerative periodontal surgery was done on the maxillary right second premolar which had deep periodontal pocket. A new bone formation around the bifurcation area of the transplanted tooth was confirmed during the surgery (Figure 4d). The autotransplanted tooth will be restored with a full crown. At the 18 month follow up, the transplanted tooth had a normal periodontal pocket depth and no mobility.
The factors affecting the prognosis of autotransplantation are donor tooth, recipient site, the duration and method of splinting after surgery, and the timing of endodontic treatment of the transplanted tooth.2,5
Above all, the decisive factor of the prognosis is the healing of periodontal ligament (PDL) cells, which depends on the vitality of PDL cells attached to the root surface of the donor tooth.3,7 Therefore, extraction without damaging the root surface of the donor tooth and fast transplantation in the recipient site are the key points for the successful autotransplantation. In these cases, a duplicated tooth model was used to prepare the recipient site with minimizing the extra-oral time of the donor tooth. Andreasen et al. reported that extra-alveolar time exceeding 18 minutes of a donor tooth affected the survival rate of PDL cells significantly.7-9 In this regard, the extra-oral time of 10 to 11 minutes in these cases seems to be the safe margin.
In addition, the root maturity of donor tooth is a very important factor with regard to the prognosis of autotransplantation. Any teeth, whether its root is opened or closed, can be the donor teeth for the autotransplantation, but the teeth with half to three-quarter root development is the optimum.2,8,10,11
Ideal recipient sites should have sufficient alveolar bone support in all dimensions, appropriate amount of attached keratinized tissue, and no inflammation.5 However, autotransplantation can be applied in localized severe periodontitis which does not show promising prognosis.2 Nethander et al. reported that it was possible for an autotransplanted tooth to obtain better blood supply by using a 2 stage operation technique.6 Lee et al. also advocated that the waiting for 2 - 4 weeks before autotransplantation showed good healing in severe periodontal cases.7
In case 2, the transplanted tooth had a normal periodontal pocket depth and no mobility at the 18-month follow up without delayed transplantation. It may be assumed that several factors contributed to this success. In addition to scaling and root planning before 1 month, we tried immediate autotransplantation after removing all inflammatory tissues in the periodontally involved socket. A periodontally healthy donor tooth was also extracted atraumatically to protect PDL cells attached to the root surface of the donor tooth. And then, it was closely adapted into the socket with 4-0 silk sutures and a semi-rigid resin wire splint. Healthy distal alveolar bone might be also considered to contribute to the stable adaptation.
The autotransplanted tooth should be held in the recipient site for periodontal healing. Flexible splinting allows functional movement of teeth, which stimulates activity of PDL cells and functional arrangement.8 Tsukiboshi reported that splinting is not essential but beneficial in the most autotransplantation cases, and the tooth should be fixed for between 2 weeks and 2 months depending on whether the mobility is reduced.3,12 In our series, the fixation was removed after 2 weeks when any vertical mobility had disappeared.
Finally, a donor tooth with complete or near complete root formation generally require endodontic treatment. Preoperative root canal therapy is preferred. Otherwise, root canal therapy after 2 weeks of surgery should be done. Since extra-alveolar endodontic treatment increases the risk of subsequent root resorption, it is to be done carefully.2,5 In case 1, root end resection and retrograde filling with MTA was performed after looking for the presence of isthmus between principals and secondary canals to prevent endodontic complications. In case 2, conventional endodontic treatment was done at 2 weeks of surgery due to the trismus of the patient.
According to Tsukiboshi, the successful transplants must show normal pocket depth, physiological mobility, no clinical discomfort, and normal PDL space and lamina dura.12 Judging by such criteria, these cases, though had short follow-up period, showed successful results.
Figures and Tables
References
1. Leffingwell CM. Autogenous tooth transplantation: a therapeutic alternative. Dent Surv. 1980. 56:22–23.
2. Thomas S, Turner SR, Sandy JR. Autotransplantation of teeth: is there a role? Br J Orthod. 1998. 25:275–282.

3. Tsukiboshi M. Autotransplantation of teeth: requirements for predictable success. Dent Traumatol. 2002. 18:157–180.

4. Cho JH, Hwang HS, Chang HS, Hwang YC. Application of orthodontic forces prior to autotransplantation-case reports. Int Endod J. 2013. 46:187–194.

5. Clokie CML, Yau DM, Chano L. Autogenous tooth transplantation: an alternative to dental implant placement? J Can Dent Assoc. 2001. 67:92–96.
6. Nethander G, Andersson JE, Hirsch JM. Autogenous free tooth transplantation in man by a 2-stage operation technique. A longitudinal intra-individual radiographic assessment. Int J Oral Maxillofac Surg. 1988. 17:330–336.

7. Lee SJ, Jung IY, Lee CY, Choi SY, Kum KY. Clinical application of computer-aided rapid prototyping for tooth transplantation. Dent Traumatol. 2001. 17:114–119.

8. Teixeira CS, Pasternak B Jr, Vansan LP, Sousa-Neto MD. Autogenous transplantation of teeth with complete root formation: two case reports. Int Endod J. 2006. 39:977–985.

9. Andreasen JO. The effect of pulp extirpation or root canal treatment on periodontal healing after replantation of permanent incisors in monkeys. J Endod. 1981. 7:245–252.

10. Lundberg T, Isaksson S. A clinical follow-up study of 278 autotransplanted teeth. Br J Oral Maxillofac Surg. 1996. 34:181–185.

11. Mejàre B, Wannfors K, Jansson L. A prospective study on transplantation of third molars with complete root formation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 97:231–238.

12. Tsukiboshi M. Autogenous tooth transplantation: a reevaluation. Int J Periodontics Restorative Dent. 1993. 13:120–149.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download