Abstract
The restorative management of deep carious lesions and the preservation of pulp vitality of immature teeth present real challenges for dental practitioners. New tricalcium silicate cements are of interest in the treatment of such cases. This case describes the immediate management and the follow-up of an extensive carious lesion on an immature second right mandibular premolar. Following anesthesia and rubber dam isolation, the carious lesion was removed and a partial pulpotomy was performed. After obtaining hemostasis, the exposed pulp was covered with a tricalcium silicate cement (Biodentine, Septodont) and a glass ionomer cement (Fuji IX extra, GC Corp.) restoration was placed over the tricalcium silicate cement. A review appointment was arranged after seven days, where the tooth was asymptomatic with the patient reporting no pain during the intervening period. At both 3 and 6 mon follow up, it was noted that the tooth was vital, with normal responses to thermal tests. Radiographic examination of the tooth indicated dentin-bridge formation in the pulp chamber and the continuous root formation. This case report demonstrates a fast tissue response both at the pulpal and root dentin level. The use of tricalcium silicate cement should be considered as a conservative intervention in the treatment of symptomatic immature teeth.
Preserving dental pulp vitality is a significant clinical challenge in restorative dentistry, especially with regard to the management of permanent immature teeth.1 According to the consensus report of the European Society of Endodontology, when the pulp of a tooth with incomplete root formation is exposed, the therapeutic procedure should preserve the vitality of the remaining part of the pulp.2 After removing the damaged pulpal tissue, it is recommended that materials that protect the underlying healthy pulpal tissues should be used to allow and promote healing and repair.2 Indicators for successful management are a normal response to pulp sensitivity tests and the absence of pain, the radiological evidence of a dentin-bridge formation, and the continuing root formation in immature teeth. In addition, there should be no evidence of clinical or radiographic signs of internal root resorption or apical periodontitis.2
Calcium hydroxide is described as the material of choice for direct pulp capping and partial or coronal pulpotomy.3 However, recent clinical studies question the predictability of the results with calcium hydroxide. In addition, the use of calcium hydroxide has been shown to be time-consuming with iterative clinical applications of the medication often required.4 Mineral Trioxide Aggregate (MTA), a tricalcium silicate cement arising from the Portland cement, was developed in the mid 1990's, initially for endodontic treatment procedures (root perforation and surgical endodontics). This material was shown to have good physico-chemical and biological properties and secondary properties preventing bacterial leakage, which are better than other current restorative materials.5-10 MTA also demonstrated additional dentin mineralization properties when used as a pulp capping agent.8,10,11 However, its handling properties remain relatively poor compared to that of calcium hydroxide.11,12
In 2009, a synthetic tricalcium silicate cement (Biodentine, Septodont, Saint Maur-des-Fossées, France) became commercially available. This new tricalcium silicate cement has high mechanical properties for restorative dentistry and appears to induce an early dental pulp mineralization.13-15
In vitro studies have demonstrated ionic uptake and infiltration of minerals at the dentinmaterial interface, which is associated with a porous internal hydrogel formation allowing for ion exchange.16-18 Although Biodentine was initially developed for endodontic applications, preliminary results with Biodentine demonstrated a successful and quick positive outcome with respect to direct pulp capping. Tricalcium silicate cements could be indicated as restorative materials for direct pulp capping with regard to their dentin-mineralizing properties.19 Indeed, the chemical setting reaction of the two main components (tricalcium silicate = Ca3SiO5 and dicalcium silicate = Ca2SiO4) of these cements leads to the release of calcium hydroxide.20
In this case report, the authors report on a clinical case where a tricalcium silicate cement (Biodentine) was used as a pulpotomy agent in the treatment of a pulpitis in permanent immature premolar.
A 12 year-old girl presented at the emergency dental clinic, Hospices Civils de Lyon, Lyon, France, for an acute, spontaneous and lasting referred pain in the right posterior mandibular quadrant. Clinical and radiographic examinations revealed extensive occlusal caries invading the pulp on the second right lower premolar, an immature permanent tooth with incomplete root formation (Figure 1a). The diagnosis was acute pulpitis (#45).
After taking the informed consent of her parents due to the young age of the patient, a conservative pulpal treatment option was adopted in order to allow for further root formation and to preserve the growing potential of the root and the healing potential of the pulp. Accordingly, #45 was anesthetized by a peri-apical injection with 1.5 mL of a 2% articaine and 1/200,000 epinephrine solution (Primacaine Adrenaline 1/200,000, Acteon Pierre Rolland, Merignac, France) and isolated under rubber-dam.
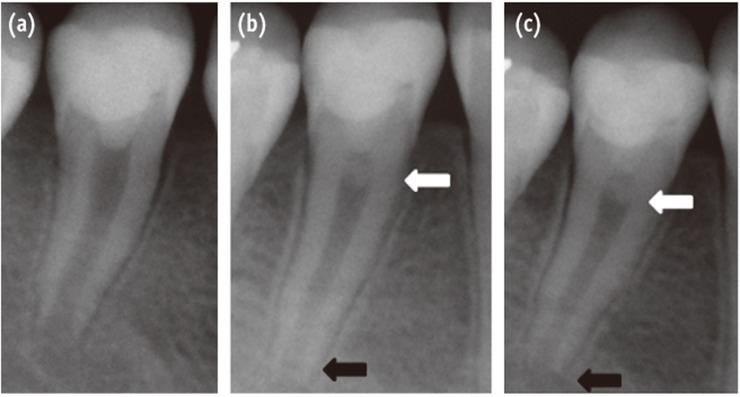
Following caries removal, a partial pulpotomy was performed using a round low-speed carbide bur (H1.204.021, Komet France, Paris, France) under constant irrigation until a normal bleeding was obtained (Figure 1b). The hemostasis was obtained by irrigation with saline solution and application of sterile cotton pellets. Biodentine was processed according to the manufacturer's instruction by mixing a single-unit powder part (tricalcium silicate-dicalcium silicate-zircon dioxide) and 5 drops of a single-unit liquid part (calcium chloride-distilled water) for 30 seconds (Figure 1c). Figure 2a displays the immediate post treatment X-ray which shows the pulp capping material located at the roof of the pulp chamber. Direct pulp capping was performed with a 2 mm-thickness layer of the tricalcium silicate cement (Biodentine). The tooth #45 was restored with conventional glass ionomer cement (Fuji IX extra, GC Corp., Tokyo, Japan) and checked for centric occlusion. At a postoperative phone call the following day, the patient reported complete cessation of the painful episode within 12 hours after completion of the treatment. At seven day follow-up, a clinical examination found responses to thermal pulpal tests within normal limits for a non-inflammatory pulp (hot and cold were discriminated and the response did not exceed the stimulus duration). At a three months recall, a clinical examination showed a normal pulpal sensitivity. There were no clinical or radiographic signs of root resorption or apical periodontitis. A radiograph showed morpho-differentiation of a dentin bridge immediately under the tricalcium silicate cement. (Figures 2b and 2c). Root formation had occurred and a thickening of the root dentin walls was noted. At 6 month recall, the bevel-shaped ends of the dentin at 3 months appeared to change to thicker round-shaped root-dentin walls.
Studies have shown that the partial pulpotomy technique obtains good clinical outcomes independent of the material used. However, the main discriminative factor between materials is the speed and quality of the dentin bridge formation.21,22 The literature cites calcium hydroxide as the gold standard for pulp capping. It is acknowledged to have many biological properties including antibacterial, antifungal and dentinogenetic effects. However, its high solubility leads to leakage and requires an additional high quality coronal sealing. Although calcium hydroxide allows for the formation of a dentin bridge, studies have shown that the resulting dentin contains tunnels, which could favour infection or necrosis of the pulp.3 In addition, the resulting root dentin is weaker than the original tissue and a higher occurrence of late root canal fracture has been reported.23
In order to overcome these deficits, researchers have looked to develop new materials with a higher sealing ability and enhanced biological properties, with one example being hard-setting calcium hydroxide. More recent developments belonging to the family of tricalcium silicate cements have seen improved biological and clinical effects. ProRoot MTA (Dentsply, Johnson City, TN, USA) was the first of a new generation biomaterials to be commercially available.
At the present time, this category of dental materials can be divided into two main groups:
- Portland-derived cements like ProRoot MTA, MTA Angelus (Angelus Soluções Odontológicas, Londrina, Brazil) or MMMTA (MicroMega, Besançon, France)
- Synthetic tricalcium silicate cements which result in an industrial mixing of tricalcium silicate and dicalcium silicate clusters like Biodentine.
The clinical interest of tricalcium silicate cements has been reported both in endodontic and restorative treatment.4,6,8,11,21,24-28 Among the tricalcium silicate cements, Biodentine has a short setting time, good mechanical properties and an effective sealing capacity (to mineralized tissues), which enables its use as a direct pulp capping and restorative material.13,17
Some authors have suggested that the favorable biological properties of tricalcium silicate cements make them valuable for preserving the vitality of the pulp in immature permanent teeth with irreversible pulpitis.19,29 Such a conservative approach using tricalcium silicate cements, as opposed to pulpectomy and root canal therapy or apexification with a standard therapy, would allow for the growth in length and thickness of the root-walls.23 Moreover, in vitro and in vivo studies have shown that the dentin bridge formation is more homogeneous and root dentin formation occurs earlier with tricalcium silicate than with calcium hydroxide based materials.4,11,22,24,28-31 These features (increased speed and quality of dentin bridge formation and root dentin formation) were observed in our case report and support the conservative approach adopted to treating this case of an irreversible pulpitis.
Biodentine tricalcium silicate cement appears to offer a valuable alternative therapeutic intervention to maintain pulp vitality for immature permanent teeth. Moreover, its handling and mechanical properties, as well as its short setting time allow for its clinical use as a conventional dentine substitute. It will be important to conduct more clinical studies to validate these observations. Conservative techniques that improve treatment outcomes in immature permanent teeth with inflammatory and infectious pulpal diseases should be encouraged.
References
1. Witherspoon DE, Small JC, Harris GZ. Mineral trioxide aggregate pulpotomies: a case series outcomes assessment. J Am Dent Assoc. 2006; 137:610–618. PMID: 16739540.
2. European Society of Endodontology. Quality guidelines for endodontic treatments: consensus report of the European Society of Endodontology. Int Endod J. 2006; 39:921–930. PMID: 17180780.
3. Mohammadi Z, Dummer PM. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011; 44:697–730. PMID: 21535021.

4. Nair PN, Duncan HF, Pitt Ford TR, Luder HU. Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with mineral trioxide aggregate: a randomized controlled trial. Int Endod J. 2008; 41:128–150. PMID: 17956562.

5. Camilleri J, Pitt Ford TR. Mineral trioxide aggregate: a review of the constituents and biological properties of the material. Int Endod J. 2006; 39:747–754. PMID: 16948659.

6. Yun YR, Yang IS, Hwang YC, Hwang IN, Choi HR, Yoon SJ, Kim SH, Oh WM. Pulp response of mineral trioxide aggregate, calcium sulfate or calcium hydrate. J Korean Acad Conserv Dent. 2007; 32:95–101.
7. Chang SW, Yoo HM, Park DS, Oh TS, Bae KS. Ingredients and cytotoxicity of MTA and 3 kinds of Protland cements. J Korean Acad Conserv Dent. 2008; 33:369–376.
8. Roberts HW, Toth JM, Berzins DW, Charlton DG. Mineral trioxide aggregate material use in endodontic treatment: a review of the literature. Dent Mater. 2008; 24:149–164. PMID: 17586038.

9. Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review-part II: leakage and biocompatibility investigations. J Endod. 2010; 36:190–202. PMID: 20113774.

10. Chang SW. Chemical characteristics of mineral trioxide aggregate and its hydration reaction. Restor Dent Endod. 2012; 37:188–193. PMID: 23429542.

11. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review-part III: clinical applications, drawbacks and mechanism of action. J Endod. 2010; 36:400–413. PMID: 20171353.

12. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review-part I: chemical, physical, and antibacterial properties. J Endod. 2010; 36:16–27. PMID: 20003930.

13. Koubi G, Colon P, Franquin JC, Hartmann A, Richard G, Faure MO, Lambert G. Clinical evaluation of the performance and safety of a new dentine substitute, Biodentine, in the restoration of posterior teeth-a prospective study. Clin Oral Investig. 2013; 17:243–249.
14. Darvell BW, WU RC. 'MTA'-an hydraulic silicate cement: review update and setting reaction. Dent Mater. 2011; 27:407–422. PMID: 21353694.

15. Laurent P, Camps J, About I. Biodentine induces TGF-β 1 release from human pulp cells and early dental pulp mineralization. Int Endod J. 2012; 45:439–448. PMID: 22188368.
16. Han L, Okiji T. Uptake of calcium and silicon released from calcium silicate-based endodontic materials into root canal dentine. Int Endod J. 2011; 44:1081–1087. PMID: 21777256.

17. Villat C, Tran XV, Pradelle-Plasse N, Ponthiaux P, Wenger F, Grosgogeat B, Colon P. Impedance methodology. A new way to characterize the setting reaction of dental cements. Dent Mater. 2010; 26:1127–1132. PMID: 20728209.

18. Atmeh AR, Chong EZ, Richard G, Festy F, Watson TF. Dentin-cement interfacial interaction: calcium silicates and polyalkenoates. J Dent Res. 2012; 91:454–459. PMID: 22436906.
19. Eghbal MJ, Asgary S, Baglue RA, Parirokh M, Ghoddusi J. MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J. 2009; 35:4–8. PMID: 19335509.

20. Camilleri J. Characterization and hydration kinetics of tricalcium silicate cement use as a dental biomaterial. Dent Mater. 2011; 27:836–844. PMID: 21600643.
21. Accorinte Mde L, Holland R, Reis A, Bortoluzzi MC, Murata SS, Dezan E Jr, Souza V, Alessandro LD. Evaluation of mineral trioxide aggregate and calcium hydroxide cement as pulp-capping agents in human teeth. J Endod. 2008; 34:1–6. PMID: 18155482.
22. Leye Benoist F, Gaye Ndiaye F, Kane AW, Benoist HM, Farge P. Evaluation of mineral trioxide aggregate (MTA) versus calcium hydroxide cement (Dycal) in the formation of a dentine bridge: a randomized controlled trial. Int Dent J. 2012; 62:33–39. PMID: 22251035.
23. Huang GT. Apexification: the beginning of its end. Int Endod J. 2009; 42:855–866. PMID: 19549154.

24. Aeinehchi M, Eslami B, Ghanbariha M, Saffar AS. Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report. Int Endod J. 2003; 36:225–231. PMID: 12657149.
25. Iwamoto CE, Adachi E, Pameijer CH, Barnes D, Romberg EE, Jefferies S. Clinical and histological evaluation of white ProRoot MTA in direct pulp capping. Am J Dent. 2006; 19:85–90. PMID: 16764130.
26. Witherspoon DE. Vital pulp therapy with new materials: new directions and treatment perspectives-permanent teeth. Pediatr Dent. 2008; 30:220–224. PMID: 18615987.

27. Accorinte ML, Loguercio AD, Reis A, Bauer JR, Grande RH, Murata SS, Souza V, Holland R. Evaluation of two mineral trioxide aggregate compounds as pulp-capping agents in human teeth. Int Endod J. 2009; 42:122–128. PMID: 19134040.

28. Bakland LK, Andreasen JO. Will mineral trioxide aggregate replace calcium hydroxide in treating pulpal and periodontal healing complications subsequent to dental trauma? A review. Dent Traumatol. 2012; 28:25–32. PMID: 21895969.

29. Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S. One-year of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter, randomized, noinferiority clinical trial. Clin Oral Investig. 2013; 17:431–439.
30. El-Meligy OA, Avery DR. Comparison of mineral trioxide aggregate and calcium hydroxide as pulpotomy agents in young permanent teeth (apexogenesis). Pediatr Dent. 2006; 28:399–404. PMID: 17036703.
31. Tran XV, Gorin C, Willig C, Baroukh B, Pellat B, Decup F, Opsahl Vital S, Chaussain C, Boukpessi T. Effect of a calcium-silicate-based restorative cement on pulp repair. J Dent Res. 2012; 91:1166–1171. PMID: 22983409.

Figure 1
(a) Preoperative radiograph of tooth #45 demonstrating an extensive occlusal caries close to the pulp chamber and incomplete root maturation; (b) Clinical view following caries removal and partial pulpotomy; (c) Color and texture of Biodentine before application.
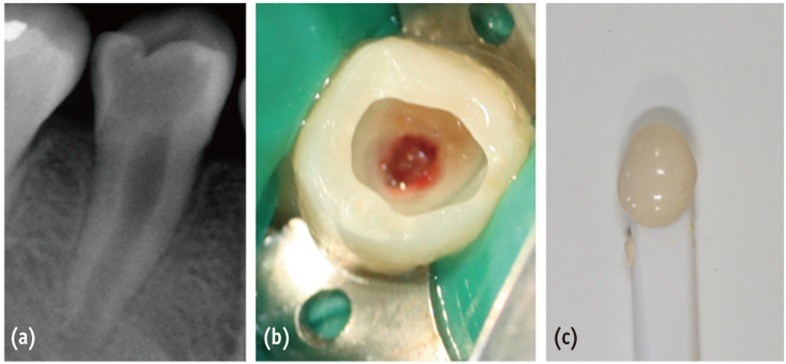
Figure 2
(a) Immediate post-operative radiograph following silicate cement (Biodentine) placement and glass ionomer cement (Fuji IX) restoration; (b) Three months follow-up radiograph: formation of pulpal roof dentin bridge (white arrow) and root edification (black arrow); (c) Six months follow-up radiograph.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download