Abstract
This case report demonstrates an unnecessary endodontic treatment of teeth with florid cemento-osseous dysplasia (FCOD) due to a misdiagnosis as periapical pathosis and emphasizes the importance of correct diagnosis to avoid unnecessary treatment. A 30-year-old woman was referred to our institution for apicoectomies of the mandibular left canine and both the lateral incisors. The periapical lesions associated with these teeth had failed to resolve after root canal treatment over a 3-year period. Radiographic examinations revealed multiple lesions on the right canine, the second premolar, and both first molars as well as the anterior region of the mandible. Based on clinical, radiographic and histological evaluations, the patient condition was diagnosed as FCOD. The patient has been monitored for 2 years. To avoid unnecessary invasive treatment, accurate diagnosis is essential before treatment is carried out in managing FCOD.
Cemento-osseous dysplasia (COD) is the most common osseous fibrous lesion, which involves replacement of the normal bone with a poorly cellularized cementum-like material and cellular fibrous connective tissue.1 The cause of COD has not fully understood, and COD lesions are known to originate from periodontal ligament tissues.1 The classification of cemento-osseous lesions remains unclear, and controversies exist among pathologists.1-4 According to the classification system by the 1992 revised World Health Organization (WHO) guidelines, COD is categorized as a form of neoplasm and other bone-related lesions, and it can be divided into periapical cemental dysplasia (PCD, periapical fibrous dysplasia), florid COD (FCOD, gigantiform cementoma, familial multiple cementomas) and other CODs.2,3 COD commonly occurs in the tooth-bearing or edentulous areas of the mandible and it may occasionally occur in the maxilla. PCD is a common type of COD. It predominantly involves the anterior mandible and affects single or multiple teeth. On the other hand, FCOD is characterized by multifocal involvement of the jaws (Table 1).4 Summerlin and Tomich suggested a separate category of COD, i.e., focal COD, which has mixed and distinguishing features of pericemental dysplasia and FCOD.5 Su et al. modified the previous WHO guidelines and proposed the term FCOD for lesions involving the lower anterior teeth and other areas.6,7
On radiographic evaluation during the early stages, a COD lesion may be detected as a round or oval apical radiolucency with a well-defined radiopaque border. In the second, mixed stage, a radiolucent lesion may include radiopacities. In the mature stage, the internal mixed area becomes completely radiopaque with a thin radiolucent periphery.1
FCOD can be differentiated from other bony lesions such as Paget's disease and, ossifying fibroma, as well as endodontic pathosis.8 In most situations, COD is diagnosed on the basis of routine radiographic examinations rather than the subjective symptoms or clinical signs of patients. A diagnosis may be particularly confusing during the early stages, when it can be misdiagnosed as an asymptomatic periapical disease because of localized periapical radiolucency.9-11
The African-American population is considered markedly predisposed to FCOD, although, it does occur occasionally in Caucasians and Asians.12-15 McDonald-Jankowski performed a systemic review of 158 cases and showed that 59% of the cases were reported in blacks, 37% in Asians, and 3% in Caucasians.4 Most cases are diagnosed in female patients in their fourth or fifth decades, with the condition occurring rarely in patients under the age of 20.9,12
Here, we present a case of mandibular FCOD, which had occurred at a relatively young age and was initially misdiagnosed as an infectious periapical disease and unnecessarily treated with root canal therapy by another dentist. This case has been followed for 2 years at our hospital.
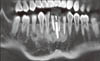
In 2009, a 30-year-old woman was referred to our institution for the evaluation and further treatment of the persistent lesions after root canal treatment of the mandibular anterior teeth (#32, 33, and 42) at a private dental clinic. The patient's medical history was unremarkable. The patient had visited the private dental clinic because of aesthetic concerns caused by congenitally missing mandibular anterior teeth (#31, and 41). The patient decided to receive an orthodontic treatment for teeth alignment and an implant surgery in the missing space. During orthodontic procedure, apical radiolucencies were detected and root canal therapies on those three teeth (#32, 33, and 42) were performed by her previous dentist. Based on the patient's report, she had received endodontic treatments because the dentist had suspected periapical pathosis due to the increased orthodontic force on the treated teeth. However, according to the previous dentist's referring notes, all of the teeth were vital at the time of treatment. On comparing a 4-year series of panoramic radiographs taken from 2005 to 2008, the previous dentist had observed that the apical radiolucencies on these teeth appeared to enlarge (Figures 1a - 1d). The dentist was concerned about the persistent periapical pathosis and referred to our institution for apicoectomies of the affected teeth. Panoramic radiographs obtained in 2007 and 2008 showed additional radiolucencies in the apical area of the mandibular right second premolar and the first molar as well as the left first premolar (Figures 1c and 1d).
Panoramic and periapical radiographs obtained at the initial visit (after the patient referral) showed mixed radiolucent and radiopaque areas in the mandibular anterior region (#32, 33, 42 and the implant between 32 and 42) and multiple radiolucent areas on the right lower posterior teeth (Figure 2).
A clinical examination revealed no swelling or bony expansion in the mandibular anterior region. None of the teeth were sensitive to percussion. The rest of the teeth except for #42, 43, and 32 responded normally to the thermal and electronic pulp tests. The patient experienced slight discomfort during palpation of the buccal mucosa of the mandibular incisors.
In the periapical areas of #32, 33, 36, 42, 43, 45, 46 and the implant, lobular-shaped radiolucencies that contained small radiopaque masses were revealed by computed tomography (CT, Somatom Sensation 64, Siemens, Munich, Germany, 120 Kvp, 90 mA). All of the lesions were related to the cortical plates, and perforation of labial and lingual cortical bones was observed on the mandibular lateral incisors. No cortical bony expansion was detected (Figure 3). Periapicies of maxillary teeth were examined as normal condition.
Based on the clinical and radiographic findings, the possibility of endodontic pathosis was excluded. An excisional biopsy was performed in the area of the mandibular incisors because the patient had experienced occasional discomfort in that area during palpation.
When the periodontal flap was elevated, the soft tissue was exposed through the perforated cortical bone around the apices of #42 and 32. After removal of the soft tissue, a sand-like structure with a firm consistency was detected. Histological analysis of the specimen revealed multiple small fragments without any fibrous capsules (Figure 4a). Multiple trabeculae of cementum-like material were observed in a dense fibrous tissue, with no signs of inflammation (Figure 4b). The calcified material was associated with collagen fibres in the trabeculae and fibroblasts. No signs of free haemorrhage or osteoclastic activity were observed. A definite diagnosis of COD was established at the following histopathological examination. Combined with the radiographic findings that showed multiple radiolucent and radiopaque lesions in both right and left mandibular teeth and incisors, our definite diagnosis for this case was FCOD.
The patient did not report any moderate or severe postoperative pain or discomfort. At the one-year follow-up appointment, the patient did not report any experience of pain or discomfort. She was scheduled for annual routine check-ups.
The patient visited the hospital without an appointment 21 months after the biopsy because of discomfort in the mandibular anterior vestibule. Her chief complaint was pain on palpation, which had started 2 days prior to her visit. No signs of infection were detected. Cone-beam CT (CBCT, Pax-Zenith3D, Vatech, Hwaseong, Korea, 104 Kvp, 5.5 mA) radiograph was taken to assess any changes in lesion size and development (Figure 5). Based on CBCT views, the apical lesions of madibular anterior teeth and the implant appeared to become more radiopaque. The patient was requested to return if she exhibited any signs of fever, swelling or pain. She did not experience any discomfort after the emergency visit. The patient was instructed to maintain annual routine check-ups.
In this report, we have described a case of FCOD misdiagnosed as inflammatory periapical diseases, which had resulted in unnecessary root canal therapy. To minimize unnecessary invasive treatments, pulp vitality tests and a careful review of the radiographs may be helpful. FCOD can be differentiated from periapical diseases by its typical radiographic appearances such as multiple lesions frequently in mandibular teeth and mixed radiolucent and radiopaque lesions. Previous dental history and pulp vitality tests are also crucial for differential diagnosis of FCOD. In this case, with the exception of the three endodontically treated teeth, the other affected teeth were vital and unrestored, which may indicate a FCOD.
A biopsy is the only definitive method for distinguishing COD from other bony lesions. However, a surgical biopsy is rarely performed. Conversely, a biopsy is recommended when the diagnosis is unclear.16,17 A biopsy of the lesion on the anterior teeth was performed in this case to confirm the diagnosis of COD and to eliminate the possibility of secondary infection due to the perforated cortical bone, since the patient had experienced slight discomfort during palpation. The texture and features of the removed specimen were consistent with those of a case described previously, in which multiple gritty fragments were obtained.18 The biopsy lesion revealed multiple bony or cementum like material and fibrous connective tissue, which was the typical appearance of COD from previous findings.10,18 Unlike cemento-ossifying fibroma, fibrous dysplasia of the jaw is a non-demarcated lesion, and it is self-limiting. However, in many instances, after the active phase of the lesion has passed, the affected bone never returns to normal, either radiographically and histologically.2 Thus, an old area of fibrous dysplasia is sometimes explored surgically, and the tissue shows a rather characteristic appearance which is sometimes referred to as an osteoid keloid.19 This was consistent with our finding that a slightly radiolucent area of the madibular right lateral incisor (#42) remained in the 21-month CBCT images (Figure 5).
To manage COD, no treatment is necessary; however, periodic clinical and radiographic follow-up is recommended.9 In an asymptomatic case, regular routine check-ups are recommended, with panoramic radiographs. Because lower anterior lesions are often blurred in a panoramic view, additional periapical radiographs of the mandibular anterior teeth can be obtained. CT may be valuable for the assessment of newly developed signs and symptoms.3,20 In this case, CT was performed when the patient was referred to the specialist. A meticulous review of the CT scans may have helped to avoid endondontic surgery. None of the lesions detected by CT showed any expansion of the cortical plates, which may have been an indication for the elimination of cyst-like lesions. According to Alsufyani and Lam, the radiographic features of COD are a bilateral occurrence, involving the anterior and posterior teeth simultaneously, with a well-defined border, a radiolucent rim and a mixed radiolucent and radiopaque structure.21 CBCT scans were repeated during the check-ups performed after the patient had expressed intermittent discomfort. Compared with CT, CBCT is associated with reduced radiation levels and provides enough information to diagnose COD lesions. However, in this case, the CBCT obtained in 21 months was not considered the ideal approach due to the unnecessary exposure to radiation. Instead, close follow-up examinations, without further panoramic radiography may be recommended in this situation.
In this case, during the routine check-ups, the patient reported that she was experiencing some discomfort. However, the symptoms had resolved without any interventions. Previous cases of FCOD with pain have been reported to be associated with pain. Cavalcante et al. reported a case in which a 44-year-old female patient had experienced uncomfortable pressure and intermittent pain in the mandibular left premolar region, and an incisional biopsy had revealed the presence of FCOD.16 Previous case reports have revealed that Asians (particularly Chinese) with FCOD had a high prevalence of pain.16 The majority of pain-related cases were in the long-term edentulous area.12
Secondary infection can occasionally occur in FCOD, and its management is known to be complicated.10 The infection is possibly secondary to osteomyelitis in an adjacent bone, or it is possible that FCOD makes the bone more susceptible to osteomyelitis.16,17
In the current case, the patient was 26-years old when the apical radiolucency (on three anterior teeth) was first detected. This is considered a relatively young age, since COD is predominantly diagnosed in middle-aged women. The transition from periapical COD to FCOD was observed by comparing the panoramic radiograph obtained in 2005 with those obtained after 2007. The conversion from periapical or focal COD to FCOD has also been reported.5 According to previous reports, periapical COD, focal COD, and FCOD are caused by the same pathologic process.1,12 In this case, a referring note from the patient's dentist demonstrated that an implant had been installed after the development of periapical radiolucencies in the mandibular anterior region. Based on this finding, COD did not appear to affect the osseointegration of the implant. Bencharit et al. also reported the successful management of FCOD including implant surgery.22
Figures and Tables
 | Figure 1A series of panoramic radiographs obtained during a previous dental consultation. (a) A panoramic radiograph obtained in February, 2005 (4 years before the initial visit to our institution) when the patient's dentist initiated orthodontic treatment. Slight periapical radiolucency on #32, 33, and 42 was detected; (b) A panoramic radiograph obtained in October, 2005 when the root canal therapies were performed on #32, 33, and 42; (c) A panoramic radiograph obtained in 2007; (d) A panoramic radiograph obtained in 2008. Compared with the radiographs in 2005, the size of the lesion in the mandibular incisors increased, and a mixed radiopaque and radiolucent area was clearly distinguishable in the apical areas of the right first molar, right second molar, and left first molar. |
 | Figure 2Radiographic examinations performed at the initial visit (in April, 2009) of the patient. (a) A panoramic radiograph showing multiple mixed radiopaque and radiolucent areas at the apices of the mandibular teeth; (b) A periapical radiograph of the lower anterior teeth. Two incisors and left canine were endodontically treated and an implant was included in the apical lesion. |
 | Figure 3Computed tomography (CT) images at the initial visit. (a) A panoramic reconstruction of the CT images at the level of the apices. Multiple lesions bony lesions were detected; (b) Axial images of #42, 32, and 46 at the apical level. Mixed radiopaque and radiolucent lesions as well as cortical bone perforation were observed; (c) Vertical images showing thinning and perforation of the cortical plate without any expansion. |
 | Figure 4Results of examination of the excisional biopsy specimens. (a) Gross appearance of the specimens. The largest specimen was 7.0 × 5.0 × 5.0 mm; (b) A histologic examination showed bony trabeculae mixed with cellularity in the stroma (hematoxylin-eosin stain, ×50). |
References
1. Waldron CA. Bone pathology. In : Neville BW, Damm DD, Allen CM, Bouquot JE, editors. Oral & Maxillofacial Pathology. 2nd ed. Philadelphia: Saunders;2002. p. 533–587.
2. Beylouni I, Farge P, Mazoyer JF, Coudert JL. Florid cemento-osseous dysplasia: report of a case documented with computed tomography and 3D imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 85:707–711.
3. Kramer IR, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumours. A commentary on the second edition. Cancer. 1992; 70:2988–2994.

4. MacDonald-Jankowski DS. Florid cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2003; 32:141–149.

5. Summerlin DJ, Tomich CE. Focal cemento-osseous dysplasia: a clinicopathologic study of 221 cases. Oral Surg Oral Med Oral Pathol. 1994; 78:611–620.

6. Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasia and cemento-ossifying fibromas. II. A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 84:540–549.

7. Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasias and cemento-ossifying fibromas: I. A pathologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 84:301–309.

8. Mupparapu M, Singer SR, Milles M, Rinaggio J. Simultaneous presentation of focal cemento-osseous dysplasia and simple bone cyst of the mandible masquerading as a multilocular radiolucency. Dentomaxillofac Radiol. 2005; 34:39–43.

9. Rodrigues CD, Estrela C. Periapical cemento-osseous dysplasia in maxillary teeth suggesting apical periodontitis: case report. Gen Dent. 2009; 57:e21–e24.
10. Galgano C, Samson J, Küffer R, Lombardi T. Focal cemento-osseous dysplasia involving a mandibular lateral incisor. Int Endod J. 2003; 36:907–911.

11. Resnick CM, Novelline RA. Cemento-osseous dysplasia, a radiological mimic of periapical dental abscess. Emerg Radiol. 2008; 15:367–374.

12. Kawai T, Hiranuma H, Kishino M, Jikko A, Sakuda M. Cemento-osseous dysplasia of the jaws in 54 Japanese patients: a radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:107–114.
13. Komabayashi T, Zhu Q. Cemento-osseous dysplasia in an elderly Asian male: a case report. J Oral Sci. 2011; 53:117–120.

14. Miyake M, Nagahata S. Florid cemento-osseous dysplasia. Report of a case. Int J Oral Maxillofac Surg. 1999; 28:56–57.

15. Ong ST, Siar CH. Florid cemento-osseous dysplasia in a young Chinese man. Case report. Aust Dent J. 1997; 42:404–408.

16. Cavalcante AS, Sgarbi FC, Agapito Lda C, Roveroni LH, Brandao AA, Cabral LA. Florid cemento-osseous dysplasia: a report of three cases. Gen Dent. 2008; 56:186–190.
17. Singer SR, Mupparapu M, Rinaggio J. Florid cemento-osseous dysplasia and chronic diffuse osteomyelitis: report of a simultaneous presentation and review of the literature. J Am Dent Assoc. 2005; 136:927–931.
18. Islam MN, Cohen DM, Kanter KG, Stewart CM, Katz J, Bhattacharyya I. Florid cemento-osseous dysplasia mimicking multiple periapical pathology-an endodontic dilemma. Gen Dent. 2008; 56:559–562.
19. Makek MS. So called 'fibro-osseous lesions' of tumorous origin. Biology confronts terminology. J Craniomaxillofac Surg. 1987; 15:154–167.
20. Ariji Y, Ariji E, Higuchi Y, Kubo S, Nakayama E, Kanda S. Florid cemento-osseous dysplasia. Radiographic study with special emphasis on computed tomography. Oral Surg Oral Med Oral Pathol. 1994; 78:391–396.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download