Abstract
Objectives
The internal adaptation of composite restorations with or without resin modified glass ionomer cement (RMGIC) was analyzed non-destructively using Microcomputed tomography (micro-CT).
Materials and Methods
Thirty intact human teeth were used. The specimens were divided into 3 groups. In the control group, the cavities were etched with 10% phosphoric acid for 15 sec. Composite resin was filled into the cavity without adhesive. In group 1, light cured glass ionomer cement (GIC, Fuji II LC, GC) was applied as a base. The cavities were then etched, bonded, light cured and filled with composites. In group 2, the cavities were then etched, bonded, light cured and filled with composites without base application. They were immersed in a 25% silver nitrate solution. Micro-CT was performed before and after mechanical loading. One-way ANOVA with Duncan analysis was used to compare the internal adaptation between the groups before or after loading. A paired t-test was used to compare internal adaptation before and after mechanical loading. All statistical inferences were made within the 95% confidence interval.
Results
The silver nitrate solution successfully penetrated into the dentinal tubules from the pulp spaces, and infiltrated into the gap between restoration and pulpal floor. Group 2 showed a lower adaptation than the control group and group 1 (p < 0.05). There was no significant difference between the control group and group 1. For all groups, there was a significant difference between before and after mechanical loading (p < 0.05).
Polymerization shrinkage of adhesive restorative materials and the difference in the physical properties of the tooth structure and restorative materials are considered the most important factors in the microleakage formation of dentin-composite resin adhesive interfaces.1 In the case of a molar restoration with composite resin, resin modfied glass ionomer cements (RMGIC) are recommended as a base because the base materials with low elastic moduli can absorb polymerization shrinkage stress2,3 and the base materials can be used to reduce the mass of the restorations to reduce polymerization shrinkage.4 On the other hand, it is unclear if the use of RMGIC can prevent gap formation in dentin-restoration interfaces. This so-called sandwich technique has not been confirmed and some researchers have reported that this technique did not offer any added advantage5,6. Opdam et al. reported that a totaletch restoration with a highly filled hybrid composite resin showed a higher clinical survival rate than a closed-sandwich restoration.7 The main reason for failure in the glass ionomer (GIC) based composite restorations was a fracture of the composites, whereas Kwon et al. reported that the use of RMGIC as a base material can reduce a marginal defect in an overlying composite restoration when the elastic modulus of RMGIC was high.8
Hayashi and Wilson reported that marginal deterioration and cavo-marginal discoloration were significantly correlated with the clinical failure rate at the 5-year review.9 Souza-Junior et al. evaluated marginal and internal adaptation of restorations, in which internal adaptation were accessed by cutting the samples after marginal adaptations had been measured first.10 In their studies, internal gap formation was most prominent at the pulpal and axiopulpal line angle of restorations. The presence of gaps at these areas could cause fluid flow in dentin tubules, resulting in typical postoperative sensitivity.11 In addition, transudation of dentinal fluid through dentin adhesive could result in the water-filled regions, which could contribute to degeneration of adhesives.12 As for the internal adaptation of restorations, Ratih et al. reported in their fluid measurement and scanning electron microscopic study that the teeth restored with a high shrinkage composite demonstrated the greatest final volume of outward flow, whereas the group lined with RMGIC showed the lowest final volume and the gap between the dentin and restoration was most intimate.13 In contrast, in other studies, the internal adaptation of dentin-restoration interfaces was evaluated by fluid flow measurements,14,15 microgap analysis,14,16 and internal leakage measurements,14 and gap formation was observed frequently when RMGIC was used as a base.
Swept-source optical coherence tomography (SS-OCT) was applied to detect defects of restoration in cross cut image in real time.17 It successfully evaluate marginal gaps, internal porosities and defects. However, it did not differentiate whether radiolucency between composite restoration and tooth was due to defective bonding or it was just image of normal bonding agent.
Some studies employed micro-CT to analyze the adaptation between the tooth and restorative materials. Some researchers reported that micro-CT was a powerful tool for quantifying polymerization shrinkage and corresponding microleakage.18,19 Kakaboura et al. evaluated the adaptation of composite resins to dentin versus the shrinkage strain of the composites.20 They reported that there was a positive correlation between the setting shrinkage and interfacial gap volume at the bottom sites of the composite restoration due to differential shrinkage. On the other hand, these studies may not be relevant to a clinical situation because the composites were placed in a cavity without adhesives. Eden et al. prepared standard class II cavities in 14 primary teeth and restored them with composite resin and adhesive.21 The teeth were then immersed in 50% silver nitrate solution for 4 hours and the penetration depth was measured with micro-CT. That study successfully analyze non-destructively the marginal adaptation of composite resin adhesive interfaces to enamel and dentin, but it did not evaluate the internal adaptation inside the restorations. In the present study, the initial internal adaptation of dentin-composite resin adhesive interfaces with or without RMGICs, and the degree of destruction of internal adaptation by mechanical loading were analyzed non-destructively using micro-CT and a silver nitrate solution.
Thirty intact human premolars or molars extracted within a month for orthodontic treatment were used. A high speed diamond bur was used to amputate the roots from the cervical regions and 3 mm (bucco-lingual) × 3 mm (mesiodistal) × 4 mm (depth) class I cavities were prepared. Using digital radiographs and its software, the distance between the cavity floors and pulp chambers was controlled within 1.0 mm. Thirty specimens were divided randomly into 3 groups.
The interior parts of the cavities were etched with 10% phosphoric acid (ALL-ETCH, Bisco Inc., Shaumburg, IL, USA) for 15 seconds. During the etching process, enamel was agitated with a minibrush, whereas dentin was not. Composite resin (Tetric N-Ceram, Ivoclar Vivadent, Schaan, Lietchtestein) was filled into the cavity without an adhesive. The cavity was filled 2 mm at each time using an incremental technique. In each increment, the composite was light cured for 20 seconds using an LED type light curing unit (Bluephase, Ivoclar Vivadent).
After a conditioner (DENTIN CONDITIONER, GC, Tokyo, Japan) was applied to the interior parts of the cavities for 20 seconds, it was irrigated and dried gently. Care was taken not to dry the exposed dentin surface too much because. Then, base layers, the thicknesses of which were 2 mm, were formed using light cured GIC (Fuji II LC, GC, Tokyo, Japan). The cavities were then processed with 10% phosphoric acid for 15 seconds, and washed and blot dried. The dentin adhesive (All-bond II, Bisco Inc.) was applied according to the manufacturer's recommendations, and cured for 20 seconds using a LED type light curing unit. The same composite resin as the control group was applied 2 mm each time using an incremental technique. The resin was cured with the LED type light curing unit for 20 seconds.
The pulp chambers were soaked with 17% Ethylenediamine tetraacetic acid (EDTA) for 5 minutes. They were then washed with saline. The teeth were immersed in 25% silver nitrate solution and were under a pressure of 3 kgf for 3 days.
High resolution micro-CT (Model 1076, SkyScan, Aartselaar, Belgium) was used to take photographs under the conditions of 100 kV acceleration voltage, 100 µA beam current, 0.5 mm Al filter, 18 µm resolution and 360° rotation at 0.5° step. Two dimensional images of 550 - 560 sagittal and coronal of each specimen were taken. During this procedure, the tooth specimen was mounted in a special template that was made purely for that specimen. This template minimizes the change in the position of the specimen during repeated use in the process. The 2D images were analyzed using the CTAn (SkyScan, Aartselaar, Belgium) program.
A custom made chewing simulator was used to apply a mechanical load of 5 kgf (- 49 N) for 640,000 times under a continuous water flow. The conical-shaped opposing plunger, which was made of nickel-chromium, was initially positioned at the center of restorations, and vertical force was applied about 2 mm above the restoration through long axis of tooth crown.
Using the same methods employed in pre-loading silver nitrate solution application, the silver nitrate solution was applied to the specimen after being loaded.
The specimen was analyzed by micro-CT using the same method as in pre-loading. The 2D images were analyzed using the CTAn program .
Among the 2D images of each specimen, 100 images clearly confirming the relationship between the pulpal floors and silver nitrate solution based on the central regions of the disto-mesial distances of cavities were selected. For the same specimen, a selection of 2D images before and after mechanical loading was made by choosing 100 cuts of 2D images arranged at equal intervals beginning from the initially photographed 2D image of a tooth. The silver nitrate penetration into the microgap between the tooth and restorative materials was considered to be valid when the densities were over 141 index, which was based on the observation that the parts clearly penetrated by the silver nitrate solution had densities > 141 index when the sagittal and coronal images (Figures 1a and 1b) of the same phase were compared. For each specimen, the length of the margin of the pulpal floor showing a microgap or intact margin was calculated in each image, and all the data was collected and summed. The ratio of the silver nitrate penetration length into the micro gap between the tooth and restoration with regard to the entire length of the pulpal floor was calculated for each specimen (% SNPL). In this way, 100 datum points were collected for each specimen and the mean % SNPL was calculated. For each group, the data of 10 specimens were collected in the same manner.
One-way ANOVA was used to compare the % SNPL between the groups before and after loading, respectively. A paired t-test was used to compare the % SNPL before and after mechanical loading. Duncan analysis was used for post hoc analysis. All statistical inferences are made within a 95% confidence interval.
Generally, the silver nitrate solution successfully penetrated into the dentinal tubules from the pulp spaces, and infiltrated into the gap between restoration and pulpal floor.
In control group, silver nitrate solution was distributed uniformly throughout the entire pulpal floors of the teeth in a control group (Figure 2a). The amount of silver nitrate penetration increased after mechanical loading. In addition, a silver nitrate solution primarily penetrated the axio-pulpal line angle regions (Figure 2b).
In group 1, a few air bubbles were observed inside the base materials and gaps were visible around the axiopulpal line angle regions. In a comparison with other groups, silver nitrate penetration was concentrated in the axiopulpal line angle regions. Even before mechanical loading, a large amount of a silver nitrate solution penetrated the specimens (Figure 3a), but a change in the penetration quantities after mechanical loading appeared to be smaller than in the control group (Figure 3b).
In group 2, before loading, a thin radiolucent line, which was assumed to be dentin adhesive, was present between the composite resin restorations and cavity floors. This line was thicker in the cavity corner than in the middle part of the cavity. After loading, the line appeared to be affected more by silver nitrate. The level of silver nitrate penetration (Figure 4a) and the change between before and after mechanical loading appeared to be smaller than in the control group (Figure 4b).
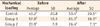
Table 1 lists the mean % SNPL and standard deviations. Group 2 showed a lower % SNPL than the control group and group 1 (p < 0.05). There was no significant difference between the control group and group 1. In all groups, there was a significant difference between before and after mechanical loading (p < 0.05).
In a pilot study which was done before this experiment, the appropriate silver nitrate concentration enabling adequate radiopacity and permeation through the dentinal tubules was studied. In addition, tooth preparation methods, the use of pressure and acid conditioning in the pulp space to enhance the penetration of silver nitrate solution from the pulp space to the gap spaces between the restoration and cavity floor were tested under many conditions. In this pretest, when the distance between the cavity floor and pulp chamber was within 1 mm, the pulp chamber was soaked with 17% EDTA for 5 minutes, and a 25% silver nitrate solution was allowed to penetrate from the pulp space to the pulpal floor of the cavity under a pressure of 3 kgf for 3 days, the silver nitrate solution could fill the gap between the teeth and restoration successfully and provided adequate radiopacity. These experimental conditions were applied in the present study. Even though it is very difficult for silver nitrate solution to penetrate deeply into gap spaces, it successfully penetrated into the dentinal tubules from the pulp spaces, and infiltrated into the gap between restoration and pulpal floor in all samples.
Before mechanical loading, % SNPL might show the internal adaptation of the initial conditions. The control group and Group 1 showed a higher % SNPL than group 2 and there was no significant difference between the control group and group 1. Many studies reported that adaptations between the tooth and glass ionomer were poor.14-16,22 Composite resin restorations with bases had inferior internal adaptation because of the porosity of light-cured GIC14 and polymerization shrinkage of the composite resin and light-cured GIC.15,23,24 The 2D image of group 1 showed many air bubbles (Figures 3a and 3b). These porocities might be incorporated during the mixing procedure of the light-cured GIC powder and solution, which could promote fluid storage and accelerate micro-gap formation.25 In the present study, as the GICs were hand mixed, more favorable results would be expected when encapsulated materials would be used. It needs further research.
During polymerization, a composite resin develops contraction force and the shear bond strength that can resist this contraction force and stop micro-gap formation was reported to be 17 - 21 MPa.26 The bond strength between the light-cured GIC and dentin is relatively low, 5 - 10 MPa,27 whereas the shear bond strength between dentin and dentin adhesives was reported to be 21 - 29 MPa.28-31 When a light cured glass ionomer is used as the base material in composite restoration, it is believed that the HEMA components of light-cured GIC form chemical bonds with the composites.32 Therefore, the micro gap in group 1 might be developed during the polymerization stage because the composites might pull up the light cured glass ionomer during the course of polymerization. When traditional GIC was used as a base and composite resin was used for the restoration, traditional GIC formed smaller micro-gaps with the dentin and larger micro-gaps with the composite resin than light-cured GIC.14 This outcome can be explained by the fact that during polymerization shrinkage of composite resin, gaps are formed between the composite resin and traditional GIC because of its lower bonding strength with the composite resin compared to that of light-cured GIC and thus stress is not transmitted to traditional GIC.24 In the present study, however, a relatively thick, 2-mm base material, Fuji II LC, was placed. The elastic modulus of Fuji II LC (6.2 - 10.8 GPa)33 is higher than that of the other light cured glass ionomer base materials, such as Vitrabond (1.1 GPa)34 and GC Lining Cement (2.9 GPa).35 The base thickness and relatively high elastic modulus of the base material might reduce the internal gaps better than the other GIC.
Polymerization shrinkage of light-cured GIC itself might be one of causes of the poor adaptation to dentin interfaces.24 Polymerization shrinkage of light-cured GIC was reported to be lower than that of the composites partly because GIC absorbs moisture and expands, thereby compensating for polymerization shrinkage.36 When light-cured GIC is used as a base, the composites on the top of the base completely exclude external moisture and only dentinal tubule fluid originating from the pulp chamber provides moisture. In the present study, the pulp chamber was removed from the extracted teeth, and the source of moisture was eliminated completely. Therefore, the light-cured GICs used as a base were self-dried and unable to compensate for polymerization shrinkage.37 Comparative analysis of internal adaptation showed that the vital teeth restored with composite resin, and light-cured GIC as bases showed superior internal adaptation but the extracted teeth with the same restorations had multiple microgaps.38 As GIC is a water-based material, it may be more likely to take up silver nitrate in the water component and porosities would be quickly filled with the silver nitrate solution, which does not represent the reality of degree of leakage/gap formation. It will also need further research.
When glass ionomers were used as base materials, the hypersensitivity after posterior composite restorations was reported to be reduced39 or at least comparable to restorations filled with the composites only.40,41 Unemori et al. reported that the postoperative sensitivity in the resin composite restorations was not related to the absence of protective layers but increased with the depth of the cavities restored with the resin composite and type of dentine-bonding.41 The internal adaptation of GIC was poor. Therefore, the internal adaptation of the base material may not affect the post operative sensitivity. In a 2D image of group 1, microgaps were formed in the axio-pulpal line angle areas of the light-cured GIC (Figures 3a and 3b). This is consistent with a previous study, which reported that polymerization shrinkage stress was concentrated mainly in the axio-pulpal line angle regions of the restoration-detin interfaces. As a result, micro-gaps were formed in those regions by a photoelastic model after restoring the teeth with composite resin, and light-cured GIC as bases.24
In group 2, the % SNPL was lower than the other groups. This might be related to the strong bonding strength of the dentin adhesives resisting the contraction force of composite resin polymerization.15 All the groups showed significant differences in %SNPL between before and after mechanical loading. In the present study, a chewing simulator was used to compare the extent of destruction of internal adaptation. Although there is some dispute as to whether the chewing simulator can mimic the long term clinical conditions,42 it would be possible to use it to evaluate the effect on the restoration after mechanical loading. In this study, thermocyling was not applied based on the study by Heintze et al., who reported that it had a slight effect on marginal adaptation, whereas mechanical loading had a significant effect.43
Before the length measurement, the Data Viewer (SkyScan) program was used to measure the densities of dentin, restorations and silver nitrate. The measured densities were 40 - 65 for dentin, 60 - 75 for light-cured GIC, 90 - 130 for the composite resin, and 125 - 180 for silver nitrate. In the present study, some light cured glass ionomers that showed a similar density to dentin were excluded, and Fuji II LC was selected because a restoration material with a similar radio-density to dentin might show background noise.44 In the present study, silver nitrate penetration into the microgap between the tooth and restorative materials was considered to be valid when the densities were > 141 index. This was based on the observation of pilot studies that the parts clearly penetrated by a silver nitrate solution had densities > 141 index when sagittal and coronal images of the same phase were compared. The index may vary in other studies because the radiodensities can differ according to the silver nitrate solution concentration and loading periods. Even though evaluating the marginal adaptation between enamel and composite was not the purpose of the present study, we could not observe any significant silver nitrate penetration in this area. In a very few cases, there were only a slight infiltration less than 100 µm. Therefore, the possibility that silver nitrate penetrated into internal gap from marginal gap seems to be very low.
In the present study, the same samples, which were used for pre-loading test, were used for post-loading test. To analyze the % SNPL after loading, the silver nitrate solution was applied to the specimen once again after being loaded using the same methods employed in preloading silver nitrate solution application. In the pilot study of this experiment, when the silver nitrate solution was not additionally applied for the after-loading analysis, the penetration of it was the same as that of pre-loading data. It means there was no further movement of silver nitrate solution after the pre load analysis. The silver nitrate may stick to the tooth substance once it contact with it. That was the reason why another silver nitrate solution was applied for post-loading test.
Overall, the method using micro-CT and a silver nitrate solution was effective in the non destructive analysis of internal adaptation between restorations and dentin. For further study, comparing the data with that of conventional sectioning or SS-OCT is necessary to corroborate the outcomes as this experiment.
The internal adaptation between dentin and restorative materials before and after loading was better when composites were bonded to tooth using adhesive agent than composites based with RMGIC. The proposed method, in which a silver nitrate solution was penetrated from the pulp space through the dentinal tubules and the amount of silver nitrate penetration in micro-gap areas was assessed by micro-CT, may provide a new measure for evaluating the internal adaptation non-destructively, but comparing the data with that of conventional sectioning seems to be necessary.
Figures and Tables
 | Figure 1Sagital and coronal section of micro-CT image. (a) Sagital section, The ratio of the silver nitrate penetration length into the microgap between the tooth and restoration with regard to the entire length of the pulpal floor was calculated for each micro-CT image (% SNPL); (b) Coronal section, Silver nitrate was penetrating into the pulpal horn (*) and into microgap between tooth and restoration (v).
Micro-CT, microcomputed tomography; R, restoration; D, dentin; V, silver nitrate infiltration lesion.
|
 | Figure 2Micro-CT image of control group before and after load cycling. (a) Before mechanical loading,compared to the other groups, a silver nitrate solution was distributed uniformly throughout the entire pulpal floors of the teeth; (b) After mechanical loading, silver nitrate solution penetrated more into the gap.
Micro-CT, microcomputed tomography; R, restoration; D, dentin; E, enamel; V, silver nitrate infiltration lesion.
|
 | Figure 3Micro-CT image of group 1 before and after load cycling. (a) Before mechanical loading, compared to other groups, silver nitrate penetration was more pronounced in the cavity corner; (b) After mechanical loading, silver nitrate solution penetrated more into the gap.
Micro-CT, microcomputed tomography; R, restoration; D, dentin, E, enamel; G, glass ionomer cement; V, silver nitrate infiltration lesion.
|
 | Figure 4Micro-CT image of group 2 before and after load cycling. (a) Before mechanical cycling; (b) After mechanical cycling. Silver nitrate penetration was more pronounced after mechanical loading in the whole pulpal wall.
Micro-CT, microcomputed tomography; R, restoration; D, dentin; E, enamel; V, silver nitrate infiltration lesion.
|
References
1. Retief DH. Do adhesives prevent microleakage? Int Dent J. 1994. 44:19–26.
2. Friedl KH, Schmalz G, Hiller KA, Mortazavi F. Marginal adaptation of composite restorations versus hybrid ionomer/composite sandwich restorations. Oper Dent. 1997. 22:21–29.
3. Tolidis K, Nobecourt A, Randall RC. Effect of a resin-modified glass ionomer liner on volumetric polymerization shrinkage of various composites. Dent Mater. 1998. 14:417–423.

4. Krejci I, Lutz F, Krejci D. The influence of different base materials on marginal adaptation and wear of conventional Class II composite resin restorations. Quintessence Int. 1988. 19:191–198.
5. Unemori M, Matsuya Y, Akashi A, Goto Y, Akamine A. Composite resin restoration and postoperative sensitivity: clinical follow-up in an undergraduate program. J Dent. 2001. 29:7–13.

6. van Dijken JW. A 6-year clinical evaluation of Class I poly-acid modified resin composite/resin composite laminate restorations cured with a two-step curing technique. Dent Mater. 2003. 19:423–428.

7. Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. Longevity and reasons for failure of sandwich and totaletch posterior composite resin restorations. J Adhes Dent. 2007. 9:469–475.
8. Kwon OH, Kim DH, Park SH. The influence of elastic modulus of base material on the marginal adaptation of direct composite restoration. Oper Dent. 2010. 35:441–447.

9. Hayashi M, Wilson NH. Marginal deterioration as a predictor of failure of a posterior composite. Eur J Oral Sci. 2003. 111:155–162.

10. Souza-Junior EJ, de Souza-Régis MR, Alonso RC, de Freitas AP, Sinhoreti MA, Cunha LG. Effect of the curing method and composite volume on marginal and internal adaptation of composite restoratives. Oper Dent. 2011. 36:231–238.

11. Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996. 21:17–24.
12. Tay FR, Pashley DH. Water treeing-a potential mechanism for degradation of dentin adhesives. Am J Dent. 2003. 16:6–12.
13. Ratih DN, Palamara JE, Messer HH. Minimizing dentinal fluid flow associated with gap formation. J Dent Res. 2006. 85:1027–1031.

14. Banomyong D, Palamara JE, Messer HH, Burrow MF. Sealing ability of occlusal resin composite restoration using four restorative procedures. Eur J Oral Sci. 2008. 116:571–578.

15. Ciucchi B, Bouillaguet S, Delaloye M, Holz J. Volume of the internal gap formed under composite restorations in vitro. J Dent. 1997. 25:305–312.

16. Peliz MI, Duarte S Jr, Dinelli W. Scanning electron microscope analysis of internal adaptation of materials used for pulp protection under composite resin restorations. J Esthet Restor Dent. 2005. 17:118–128.

17. Ishibashi K, Ozawa N, Tagami J, Sumi Y. Swept-source optical coherence tomography as a new tool to evaluate defects of resin-based composite restorations. J Dent. 2011. 39:543–548.

18. Sun J, Eidelman N, Lin-Gibson S. 3D mapping of polymerization shrinkage using X-ray micro-computed tomography to predict microleakage. Dent Mater. 2009. 25:314–320.

19. Zeiger DN, Sun J, Schumacher GE, Lin-Gibson S. Evaluation of dental composite shrinkage and leakage in extracted teeth using X-ray microcomputed tomography. Dent Mater. 2009. 25:1213–1220.

20. Kakaboura A, Rahiotis C, Watts D, Silikas N, Eliades G. 3D-marginal adaptation versus setting shrinkage in light-cured microhybrid resin composites. Dent Mater. 2007. 23:272–278.

21. Eden E, Topaloglu-Ak A, Cuijpers V, Frencken JE. Micro-CT for measuring marginal leakage of Class II resin composite restorations in primary molars prepared in vivo. Am J Dent. 2008. 21:393–397.
22. Peters OA, Laib A, Rüegsegger P, Barbakow F. Three-dimensional analysis of root canal geometry by high-resolution computed tomography. J Dent Res. 2000. 79:1405–1409.

23. Hotta M, Aono M. Adaptation to the cavity floor of the light-cured glass ionomer cement base under a composite restoration. J Oral Rehabil. 1994. 21:679–685.

24. Oliveira LC, Duarte S Jr, Araujo CA, Abrahão A. Effect of low-elastic modulus liner and base as stress-absorbing layer in composite resin restorations. Dent Mater. 2010. 26:e159–e169.

25. Nomoto R, Komoriyama M, McCabe JF, Hirano S. Effect of mixing method on the porosity of encapsulated glass ionomer cement. Dent Mater. 2004. 20:972–978.

26. Retief DH, Mandras RS, Russell CM. Shear bond strength required to prevent microleakage of the dentin/restoration interface. Am J Dent. 1994. 7:44–46.
27. Erickson RL, Glasspoole EA. Bonding to tooth structure: a comparison of glass-ionomer and composite-resin systems. J Esthet Dent. 1994. 6:227–244.

28. Nery S, McCabe JF, Wassell RW. A comparative study of three dental adhesives. J Dent. 1995. 23:55–61.

29. Tjan AH, Castelnuovo J, Liu P. Bond strength of multistep and simplified-step systems. Am J Dent. 1996. 9:269–272.
30. Triolo PT Jr, Swift EJ Jr, Barkmeier WW. Shear bond strengths of composite to dentin using six dental adhesive systems. Oper Dent. 1995. 20:46–50.
31. van der Vyver PJ, de Wet FA. Shear bond strength of four dentine bonding systems to dry and moist dentine. J Dent Assoc S Afr. 1997. 52:555–558.
32. Eliades G, Palaghias G. In vitro characterization of visible light-cured glass ionomer liners. Dent Mater. 1993. 9:198–203.
33. Cattani-Lorente MA, Dupuis V, Moya F, Payan J, Meyer JM. Comparative study of the physical properties of a polyacid-modified composite resin and a resin-modified glass ionomer cement. Dent Mater. 1999. 15:21–32.

34. Tam LE, McComb D, Pulver F. Physical properties of proprietary light-cured lining materials. Oper Dent. 1991. 16:210–217.
35. Tam LE, Pulver E, McComb D, Smith DC. Physical properties of calcium hydroxide and glass-ionomer base and lining materials. Dent Mater. 1989. 5:145–149.

36. Young AM. FTIR investigation of polymerisation and polyacid neutralisation kinetics in resin-modified glass-ionomer dental cements. Biomaterials. 2002. 23:3289–3295.

37. Feilzer AJ, Kakaboura AI, de Gee AJ, Davidson CL. The influence of water sorption on the development of setting shrinkage stress in traditional and resin-modified glass ionomer cements. Dent Mater. 1995. 11:186–190.

38. Mason PN, Ferrari M. In vivo evaluation of glass-ionomer cement adhesion to dentin. Quintessence Int. 1994. 25:499–504.
39. Akpata ES, Sadiq W. Post-operative sensitivity in glass-ionomer versus adhesive resin-lined posterior composites. Am J Dent. 2001. 14:34–38.
40. Burrow MF, Banomyong D, Harnirattisai C, Messer HH. Effect of glass-ionomer cement lining on postoperative sensitivity in occlusal cavities restored with resin composite-a randomized clinical trial. Oper Dent. 2009. 34:648–655.

41. Unemori M, Matsuya Y, Akashi A, Goto Y, Akamine A. Composite resin restoration and postoperative sensitivity: clinical follow-up in an undergraduate program. J Dent. 2001. 29:7–13.

42. Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007. 9:Supplement 1. 77–106.
43. Heintze S, Forjanic M, Cavalleri A. Microleakage of Class II restorations with different tracers-comparison with SEM quantitative analysis. J Adhes Dent. 2008. 10:259–267.
44. Chen X, Cuijpers V, Fan M, Frencken JE. Optimal use of silver nitrate and marginal leakage at the sealant-enamel interface using micro-CT. Am J Dent. 2009. 22:269–272.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download