Abstract
Although several methods including composite resin restoration and microabrasion have been used for management of white spot lesion, tooth jewelry can be considered as another noninvasive option. This case report describes the management of white spot lesions by using tooth jewelry. This report also highlights the patients' preference for tooth jewelry as an esthetic concern.
The management of a white spot lesion is an important topic in operative dentistry. Although there are several ways to manage white spot lesions, most of them are invasive approaches including composite resin restorations and prosthetic approaches.1 Furthermore, even the minimally invasive techniques such as microabrasion and resin infiltration technique cannot be considered as predictable approaches. Son et al. reported that neither microabrasion nor resin infiltration technique can remove white spot lesions completely.2 Notably, the management of a white spot lesion with tooth jewelry has attracted much attention because it possesses not only temporary masking effect of white spot lesion but also cosmetic effect for the patients who are interested in beauty. Historically, tooth jewelry is documented to have been popular among ancient people. According to an analysis of thousands of teeth examined at the Mexico's National Institute of Anthropology and History, ancient people of southern North America used semi-precious gems to beautify their teeth. Even nowadays the use of intraoral jewelry and piercings of oral or perioral tissues is becoming popular among young adults.3
Various types of tooth jewelry are available in the market including Skyce (Ivoclar Vivadent AG, Schaan, Liechtenstein) and Twinkles (TwindentAB, Uppsala, Sweden) (Figure 1). They have been preferably attached on upper incisive and canine teeth using composite resin cements just for cosmetic purpose.4 However, to our knowledge, there hasn't been any case report about the use of tooth jewelry for management of white spot lesions. Therefore, this case report describes two clinical cases of the management of white spot lesions using tooth jewelry.
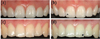
A 23-year-old female patient with a non-contributory medical history, presented to Wonkwang University Dental Hospital, Department of Conservative Dentistry for the removal of white spot lesions on the labial surface of the maxillary incisors (Figure 2a). Intraoral examination showed that the white spot lesions were present on maxillary central incisors and maxillary left canine. No specific feature was found on diagnostic radiographs. After clinical and radiographic examination, the white spots on maxillary central incisors and left canine were diagnosed as enamel hypomineralization.
Based on the moderate degree of hypomineralization, the treatment options including resin restoration or laminate veneer were explained to the patient. However, the patient showed a considerable fear of dental procedure and rejected tooth preparation. After discussing with the patient, tooth jewelry was considered as a treatment option. The lesion located on the distal part of the labial surface of the maxillary right central incisor was most notable, thus we decided as an appropriate position for tooth jewelry.
After discussing the final location of the tooth jewelry with the patient, phosphoric acid etching (Scotchbond Etchant, 3M ESPE, St. Paul, MN, USA) and adhesive system application (Adper Scotchbond Multi-Purpose Adhesive, 3M ESPE) were performed. One drop of flowable composite resin (Filtek Supreme Ultra Flowable Restorative, A1, 3M ESPE) was placed on the bottom surface of tooth jewelry (Twinkles) which was stuck to the tip of the resin instrument using petroleum jelly and transferred on the white spot lesion (Figure 3). Then, the location of jewelry was adjusted by the operator and confirmed by the patient with a hand mirror at the same time. After removal of redundant resin, light polymerization was performed for 60 seconds. The patient was informed that there could be a feeling of irritation during the first 1 or 2 days and the discomfort would disappear with time. Oral hygiene instructions were given as well. The patient has been satisfied with the result after 6 months (Figure 2b).
A 25-year-old male patient presented with a chief complaint of an unattractive smile because of the presence of a white spot lesion (Figure 2c). The medical history of the patient was non-contributory. Intraoral examination showed that a single white spot lesion was present on the incisal third of the maxillary left central incisor. The patient's oral hygiene index was scored as 0. Multiple gingival recessions and cervical abrasions were detected and cold sensitivity was observed on the cervical region of the maxillary central incisors.
The patient rejected all treatment options requiring tooth preparation. After discussing with the patient, tooth jewelry was considered as a treatment option. We explained that the tooth jewelry would have a masking effect, didn't need any tooth preparation, and could be removed at any time. Tooth jewelry (Shine, Vertriebsges, Innsbruck, Austria) was bonded to the distal part of the maxillary left central incisor following same procedure shown in the first case (Figure 2d). Cautions were given to the patient that debonding should be done only in a dental clinic. After 4 months, the patient came for removal of the tooth jewelry. The tooth jewelry was maintained well without marginal discoloration. After rubber dam isolation, tooth jewelry was debonded safely using an ultrasonic scaler, followed by removal of remaining resin with a low-speed finishing carbide bur.
White spot lesions have been managed with various options in the clinic. However, it is difficult to correctly inform the concerned patient about the outcome of his or her white spot lesion, because the operator cannot clinically see the entire volume of the white spot lesion but only its surface area. In addition, when planning treatment, many aspects such as the complete removal of lesion, tooth preparation and various demands of the patients should be considered.
Restorative treatment is a conventional approach for treating with spot lesion; however, this technique has the disadvantage of being invasive.1 The microabrasion technique was advocated for the removal of white spot lesions as well. Murphy et al.5 showed 83% success in the reduction of white spot lesions by microabrasion. Resin infiltration, a new minimally invasive technique for treating white spot lesion has the advantage that, when their microporosities are filled with the resin, the whitish appearance of the enamel lesions disappear and look similar to sound enamel.6,7 But this technique is contraindicated in other causes of white spot lesion, such as flurosis, hypoplasia, hypocalcification, erosion and tetracycline staining. Previous reports supposed that correct diagnosis concerning lesion depth and prognosis of the resin infiltration or microabrasion of white spot lesion was a crucial factor in the decision-making process and in the success.8,9 The current cases suggested a cosmetic, noninvasive and reversible treatment option for white spot lesions with tooth jewelry.
Before the clinician decides to use tooth jewelry for masking white spot lesion, the patient's agreement regarding tooth jewelry, level of oral hygiene and the type of white spot lesion should be considered. If the patient wants to postpone invasive treatment and accepts the attachment, tooth jewelry might be considered as a temporary option. But if the patient has poor oral hygiene and high caries risk factors, tooth jewelry is not recommended because it might increase the accumulation of plaque and cariogenic microorganisms around the tooth jewelry and might cause secondary caries.10 Regarding the placement of tooth jewelry, there are a few things to be considered. First, at a single spot, tooth jewelry can simply be placed on the lesion as shown in second case. In the case of multiple white spot lesions as shown in the first case, tooth jewelry can be placed on the largest lesion to disperse the attention. Second, it is essential to debond tooth jewelry without damaging the enamel surface. Chan et al.11 showed the existence of transitional zone between the affected and the unaffected enamel. The enamel in this transitional region adjacent to affected enamel has notable alterations in the prism sheath which likely contributes to the lowered mechanical properties. In the second case, bonding failure was detected at the jewelry-adhesive interface which leaves a relatively intact enamel surface. Thus it was thought to be debonded safely with ultrasonic debonding.
Depending on the type of white spot lesion, the noninvasive treatment options have some limitations. The remineralization procedure is often limited to the surface of the lesion, resulting in a poor aesthetic outcome.12 Bleaching protocol for masking white fluorosis blemishes has been reported, but its aesthetic effect is also limited, and side effects such as post-treatment sensitivity are commonly encountered.13,14 In the second case, the patients had an excellent oral hygiene and relatively well-demarcated hypomineralized lesion, and looked for the most conservative treatment option. Before making the decision, the patients were informed that bonding of the jewelry would not promote remineralization of the lesion and that tooth jewelry technique was not a permanent treatment but a temporary masking technique. Considering these factors, tooth jewelry can be used to treat white spot lesions.
Figures and Tables
References
1. Malterud MI. Minimally invasive restorative dentistry: a biomimetic approach. Pract Proced Aesthet Dent. 2006. 18:409–414.
2. Son JH, Hur B, Kim HC, Park JK. Management of white spots: resin infiltration technique and microabrasion. J Korean Acad Conserv Dent. 2011. 36:66–71.

3. American Academy of Pediatric Dentistry Council on Clinical Affairs. Policy on intraoral and perioral piercing. Pediatr Dent. 2008-2009. 30:56–57.
4. Jeger F, Lussi A, Zimmerli B. Oral jewelry: a review. Schweiz Monatsschr Zahnmed. 2009. 119:615–631.
5. Murphy TC, Willmot DR, Rodd HD. Management of postorthodontic demineralized white lesions with microabrasion: a quantitative assessment. Am J Orthod Dentofacial Orthop. 2007. 131:27–33.

6. Paris S, Meyer-Lueckel H. Masking of labial enamel white spot lesions by resin infiltration-a clinical report. Quintessence Int. 2009. 40:713–718.
7. Shivanna V, Shivakumar B. Novel treatment of white spot lesions: a report of two cases. J Conserv Dent. 2011. 14:423–426.

8. Torlakovic L, Olsen I, Petzold C, Tiainen H, Øgaard B. Clinical color intensity of white spot lesions might be a better predictor of enamel demineralization depth than traditional clinical grading. Am J Orthod Dentofacial Orthop. 2012. 142:191–198.

9. Reston EG, Corba DV, Ruschel K, Tovo MF, Barbosa AN. Conservative approach for esthetic treatment of enamel hypoplasia. Oper Dent. 2011. 36:340–343.

10. Greene JC, Vermillion JR. The oral hygiene index: a method for classifying oral hygiene status. J Am Dent Assoc. 1960. 61:172–179.

11. Chan YL, Ngan AH, King NM. Degraded prism sheaths in the transition region of hypomineralized teeth. J Dent. 2010. 38:237–244.

12. Willmot DR. White lesions after orthodontic treatment: does low fluoride make a difference? J Orthod. 2004. 31:235–242.

13. Wright JT. The etch-bleach-seal technique for managing stained enamel defects in young permanent incisors. Pediatr Dent. 2002. 24:249–252.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download