Abstract
Hypoesthesia after an inferior alveolar nerve (IAN) block does not commonly occur, but some cases are reported. The causes of hypoesthesia include a needle injury or toxicity of local anesthetic agents, and the incidence itself can cause stress to both dentists and patients. This case presents a hypoesthesia on mental nerve area followed by IAN block anesthesia with 2% lidocaine. Prescription of steroids for a week was performed and periodic follow up was done. After 1 wk, the symptoms got much better and after 4 mon, hypoesthesia completely disappeared. During this healing period, only early steroid medication was prescribed. In most cases, hypoesthesia is resolved within 6 mon, but being aware of etiology and the treatment options of hypoesthesia is important. Because the hypoesthesia caused by IAN block anesthesia is a mild to moderate nerve injury, early detection of symptom and prescription of steroids could be helpful for improvement of the hypoesthesia.
Hypoesthesia is defined as a decrease in normal sensation. Paresthesia, which is commonly confused with hypoesthesia, might have a decrease in normal sensation or might not. It is defined as any abnormal sensation such as burning, tingling, pricking, or numbness.1 Although local anesthetics are considered to be safe, they may involve some complications. One of these complications is hypoesthesia.2 When dentists perform inferior alveolar nerve (IAN) block anesthesia, a needle is injected near the IAN and lingual nerve, and then a local anesthetic agent infiltrates into these nerves. During this procedure, a direct mechanical injury or a chemical injury derived from the local anesthetic agents can be happened. Estimates of the incidence of local anesthetic-related neurosensory disturbance vary widely ranging from 1/42 to 1/750,000.3-7 Though over 85 percent of such injuries resolve spontaneously, it can remain permanently in some cases.8 Furthermore, incidence of hypoesthesia or paresthesia itself can cause stress to both dentists and patients. Therefore, dentists should understand the etiology and degree of nerve injury to provide a proper treatment or medication when a problem happens.
This unusual case report presents the hypoesthesia after IAN block anesthesia with 2% lidocaine, and discusses about the possible causes of hypoesthesia and ways to manage it.
A 36-year-old woman was presented to the department of conservative dentistry in Yonsei University, Dental College, Seoul, Korea. She received a root canal treatment for about five times before, but complained of spontaneous pain on the mandibular right second premolar. She had no specific medical history. The mandibular right second premolar was tested positive response to percussion, so it was diagnosed as previously initiated therapy, and symptomatic apical periodontitis. A nonsurgical root canal treatment was explained to the patient. She understood the treatment options and risk factors and signed the consent forms to proceed with the nonsurgical root canal treatment.
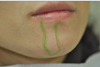
On the first day of the treatment, the IAN block anesthesia using 2% lidocaine (1:100,000 epinephrine, Huons Co., Ltd., Sungnam, Korea) was performed, and canal irrigation was done. Two days later, she called to our clinic and complained of feeling numb on her lower right lip and chin area. She also complained about feeling weird when chewing. Since hypoesthesia was suspected, we recommended her to visit our clinic as soon as possible. She visited our clinic two days after the call. She complained about dull sensation lasting on her lower right lip and chin area which is suspected to be a mental nerve innervations region. A Light touch test and pin prick test was performed and scored one-tenth comparing to the normal left side on her lip and chin. Hypoesthesia was diagnosed, so oral steroid was prescribed for a week and the patient was informed about the tapering procedure. Also, on the same day, mapping on the hypoesthetic region was performed (Figure 1).
After a week, she felt better but tickling sensation persisted on the region. Light touch test and pin prick test was again performed and scored one-half to two-thirds comparing to the left side. It was thought that healing was taking place, so additional medicine was not prescribed. At the 2 weeks follow up, the hypoesthesia was consistently getting better and 80 to 90 percent of sensation was recovered, compared to the left side. Five weeks after hypoesthesia was noticed, mapping was performed again (Figure 2). Comparing with the first mapping, the hypoesthetic region was decreased in size. During this period, non-surgical root canal treatment was accomplished including several canal irrigation appointments.
Four months later, she came to our office for a regular check-up. The hypoesthesia was completely resolved.
Hypoesthesia can occur when any kind of injuries cause damage to the nerve fiber. The causes of injury are direct injury from needle injection around the nerve fiber, mechanical injury including indirect pressure to the mandibular canal during surgical procedures, and toxicity of local anesthetic agents.2,7,9 The needle injury can be a direct injection to the nerve fiber or a vascular damage around the nerve making hematoma that presses the nerve fiber. Furthermore, surgical dental procedure such as implant surgery or orthognatic surgery can also cause hypoesthesia. Although it is not commonly accepted but toxicity of local anesthetic agents may also offer a chance to cause hypoesthesia. It had been reported that hypoesthesia happened more often with 4% articaine or prilocaine.10
In the current study, we did not perform any surgical procedure. Therefore, a needle injury or local anesthetic agent toxicity was suspected to be the possible causes of the hypoesthesia. After carefully examining the possible causes of hypoesthesia, we first excluded the needle injury from the possible causes because of the following reasons. When performing IAN block anesthesia, shooting sensation or any uncomfortable feeling was not detected. In addition, it is hard to inject directly to the IAN because of the low tension of the nerve.
The toxicity of local anesthetic agents, which was the second possibility of the causes, is not clearly identified, but it is known that the toxicity can be a problem only when local anesthetic agents are used in animal studies with high dose.11 In vivo, some case reports suggested that the articaine or prilocaine can cause hypoesthesia or paresthesia more frequently, but it was self-reporting article and the incidence could have been overestimated. In our case, 2% lidocaine was used during the procedure and is known to be safe in most reports, so we also excluded this possibility.12
Lastly, hematoma can occur when the feeding vessels near the IAN are damaged. Inside or outside the epineurium, there are some feeding vessels running along the IAN. When these vessels are damaged by the needle during local anesthetic procedure, hematoma can be resulted. If the formed hematoma is large enough to press the nerve, then complications like hypoesthesia or paresthesia can develop. We concluded this to be only possible explanation to the hypoesthesia because other reasons cannot fully explain the hypoesthesia.
When hypoesthesia is suspected, there is a clinical testing called a neurosensory testing and it is performed in two parts: mechanical stimulation and nociceptive stimulation.13 From these tests, we can examine condition of nerve fiber. A light touch test is to test mechanical stimulation and a pin prick test is to test nociceptive stimulation. Among many other tests, in our case light touch test and pin prick test are used because additional special instrument is not needed and easy to perform. Since there was no abnormal sensation and just reduced sensation, hypoesthesia is diagnosed and treated accordingly.
In management of hypoesthesia, understanding the degree of injury is important. According to the classification by Sunderland, nerve injury is divided into 5 categories, from degree 1 which means conduction block to degree 5 which is nerve damage to epineurium.14 In this case, hypoesthesia was caused by the hematoma, so the injury was estimated to be degree 1. It is also called neuropraxia in Seddon's classification.15 Since the severity was in the degree 1, complete healing was expected.
When hypoesthesia or paresthesia occurs, it is recommended to prescribe oral steroids within 10 days since the nerve injury. Usually, steroids are used to treat nerve injuries such as facial palsy, optic neuritis, and spinal cord injury.16-19 Steroid is effective in healing of an early nerve injury because it reduces cytotoxic edema and improves nerve cell survival. Because of these same reasons, steroid is widely used and effective not only in nerve injuries but also in hypoesthesia.20 Steroids play a significant role in the anti-inflammatory action to subside the swelling. When the symptom persists, prescription of gabapentin or tricylclic antidepressants (TCA) is recommended from 10 days to 3 months after the nerve injury. After 3 months, a combination of these medications is indicated, and a surgery can be considered. Usually medications used after 10 days since the nerve injury is only effective for pain control and not for treating the symptoms of hypoesthesia or paresthesia. If the patients do not complain any painful feelings, additional medications are not indicated. However, when patients feel severe pain, additional NSAIDs can be helpful for pain control.21,22
In our study, the hypoesthesia was from the hematoma, and the degree of injury was 1 according to the Sunderland's classification. The patient did not feel any kind of pain. Therefore, we expected the complete healing within 6 months aided by early steroid prescription. As expected, the hypoesthesia was completely resolved at the 4 month follow-up visit. Prescription of oral steroids was the proper management in this case. If she had complained painful feeling, NSAIDs could have been prescribed additionally.
This case report presents a hypoesthesia after IAN block anesthesia that finally resolved in 4 months. The hypoesthesia may have been caused by a hematoma formation near the IAN which resulted pressure to the nerve. The patient did not complain of any pain from the region; therefore early oral steroid prescription was done which can be helpful to overcome the hypoesthesia. Because overprescribing of medication is not recommended, dentists should be aware of degree of nerve injury, timing of intervention, and proper management methods including medication prescription to ensure a better prognosis dealing with hypoesthesia.
Figures and Tables
References
1. Lichtor T, Mullan JF. A 10-year follow-up review of percutaneous microcompression of the trigeminal ganglion. J Neurosurg. 1990. 72:49–54.

2. Hillerup S, Jensen RH, Ersbøll BK. Trigeminal nerve injury associated with injection of local anesthetics: needle lesion or neurotoxicity? J Am Dent Assoc. 2011. 142:531–539.
3. Haas DA, Lennon D. A 21 year retrospective study of reports of paresthesia following local anesthetic administration. J Can Dent Assoc. 1995. 61:319–320. 323–326. 329–330.
4. Krafft TC, Hickel R. Clinical investigation into the incidence of direct damage to the lingual nerve caused by local anaesthesia. J Craniomaxillofac Surg. 1994. 22:294–296.

5. Dower JS Jr. Anesthetic study questioned. J Am Dent Assoc. 2007. 138:708. 710. author reply 710, 712.

6. Pogrel MA, Thamby S. Permanent nerve involvement resulting from inferior alveolar nerve blocks. J Am Dent Assoc. 2000. 131:901–907.
7. Pogrel MA, Bryan J, Regezi J. Nerve damage associated with inferior alveolar nerve blocks. J Am Dent Assoc. 1995. 126:1150–1155.

8. Haas DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002. 68:546–551.
9. Reina MA, López A, De Andrés JA, Machés F. Possibility of nerve lesions related to peripheral nerve blocks. A study of the human sciatic nerve using different needles. Rev Esp Anestesiol Reanim. 2003. 50:274–283.
10. Garisto GA, Gaffen AS, Lawrence HP, Tenenbaum HC, Haas DA. Occurrence of paresthesia after dental local anesthetic administration in the United States. J Am Dent Assoc. 2010. 141:836–844.

11. Kirihara Y, Saito Y, Sakura S, Hashimoto K, Kishimoto T, Yasui Y. Comparative neurotoxicity of intrathecal and epidural lidocaine in rats. Anesthesiology. 2003. 99:961–968.

12. Gaffen AS, Haas DA. Retrospective review of voluntary reports of nonsurgical paresthesia in dentistry. J Can Dent Assoc. 2009. 75:579.
13. Omer GE Jr. Methods of assessment of injury and recovery of peripheral nerves. Surg Clin North Am. 1981. 61:303–319.

14. Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain. 1951. 74:491–516.

15. Seddon HJ, Medawar PB, Smith H. Rate of regeneration of peripheral nerves in man. J Physiol. 1943. 102:191–215.

16. Lagalla G, Logullo F, Di Bella P, Provinciali L, Ceravolo MG. Influence of early high-dose steroid treatment on Bell's palsy evolution. Neurol Sci. 2002. 23:107–112.
17. Austin JR, Peskind SP, Austin SG, Rice DH. Idiopathic facial nerve paralysis: a randomized double blind controlled study of placebo versus prednisone. Laryngoscope. 1993. 103:1326–1333.
18. Wray SH. Optic neuritis: guidelines. Curr Opin Neurol. 1995. 8:72–76.
19. Ramsey MJ, DerSimonian R, Holtel MR, Burgess LP. Corticosteroid treatment for idiopathic facial nerve paralysis: a meta-analysis. Laryngoscope. 2000. 110:335–341.

20. Seo K, Tanaka Y, Terumitsu M, Someya G. Efficacy of steroid treatment for sensory impairment after orthognathic surgery. J Oral Maxillofac Surg. 2004. 62:1193–1197.

21. Lewis MA, Sankar V, De Laat A, Benoliel R. Management of neuropathic orofacial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. 103:S32.e1–S32.e24.

22. Park JH, Lee SH, Kim ST. Pharmacologic management of trigeminal nerve injury pain after dental implant surgery. Int J Prosthodont. 2010. 23:342–346.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download