Abstract
Objectives
This study evaluated the influence of chlorhexidine (CHX) on the microtensile bonds strength (µTBS) of resin core with two adhesive systems to dentin in endodontic cavities.
Materials and Methods
Flat dentinal surfaces in 40 molar endodontic cavities were treated with self-etch adhesive system, Contax (DMG) and total-etch adhesive system, Adper Single Bond 2 (3M ESPE) after the following surface treatments: (1) Priming only (Contax), (2) CHX for 15 sec + rinsing + priming (Contax), (3) Etching with priming (Adper Single Bond 2), (4) Etching + CHX for 15 sec + rinsing + priming (Adper Single Bond 2). Resin composite build-ups were made with LuxaCore (DMG) using a bulk method and polymerized for 40 sec. For each condition, half of specimens were submitted to µTBS after 24 hr storage and half of them were submitted to thermocycling of 10,000 cycles between 5℃ and 55℃ before testing. The data were analyzed using ANOVA and independent t-test at a significance level of 95%.
Results
CHX pre-treatment did not affect the bond strength of specimens tested at the immediate testing period, regardless of dentin surface treatments. However, after 10,000 thermocycling, all groups showed reduced bond strength. The amount of reduction was greater in groups without CHX treatments than groups with CHX treatment. These characteristics were the same in both self-etch adhesive system and total-etch adhesive system.
Effective cleaning and shaping of the root canal, as well as hermetic apical seal is a significant part for successful endodontic treatment. It was reported that root canal fillings exposed to saliva may become contaminated regardless of the materials and obturation techniques employed.1 Lack of adhesion and sealing between the coronal restoration and tooth structure may jeopardize the prognosis of root canal treatment, because penetration of microorganism from a coronal portion potentially reinfects the canal system.2 Weine indicated that improper restoration leads to loss of endodontically treated teeth more than actual failure of endodontic therapy.3
Lately, the opportunity of restoring nonvital teeth with resin composite has increased as a result of the development of better dentin bonding systems. The restoration of root filled teeth with adhesive systems offers many advantages over the use of traditional, nonadhesive materials. For example, bonded resins permit transmission of functional stresses across the bonded interface to the tooth, with the potential to reinforce the weakened tooth structure.4 Durable bond between adhesive resin and dentin depends on the penetration of the primer and adhesive resin into the conditioned dentine surface in order to interlock micromechanically between the dentine collagen and resin to form a hybrid layer.5
Recently, it has been widely stated that resin-dentin bonds obtained with contemporary adhesive systems can be deteriorated over time. Deterioration of dentin collagen fibrils contributes to the mechanism responsible for bond degradation.6 The issue of collagen instability has potential consequence in the pathogenesis of dentinal caries, with the breakdown of acid-demineralized collagen matrices by host-derived matrix metalloproteinases (MMPs), a class of zinc- and calcium-dependent endopeptidases.7,8 MMPs are capable of degrading all extracellular matrix components. Human dentin contains at least MMP-2, MMP-8, MMP-9 and MMP-20. Some of these MMPs (e.g., MMP-8) attack collagen, while others (e.g., MMp-2 and -9) attack gelatin.9 These MMPs can slowly hydrolyze unprotected collagen fibrils of dentin hybrid layers which are thought to be responsible for the manifestation of thinning and disappearance of collagen fibrils from incompletely infiltrated hybrid layers in aged, bonded dentin.6,7 The low but persistent endogenous collagenolytic and gelatinolytic activities can be inhibited by the use of protease inhibitors, indicating that MMP inhibition might be beneficial in the preservation of hybrid layers.6
Chlorhexidine digluconate (CHX) is widely used as an antimicrobial agent and possesses a broad spectrum of activity against oral bacteria.10 It has been stated that the currently accepted disinfection technique applying CHX to acid-etched dentin may prevent the degradation of collagen fibrils.6 Thus, apart from being a commonly known disinfectant, CHX also functions as a potent MMP inhibitor.11 Furthermore, the use of CHX significantly improved the integrity of the hybrid layers and bond strength created by simplified etch-and-rinse adhesives.12
Modern adhesives can be grouped into two categories according to their etching technique: total-etch and self-etch products.13 Total-etch systems have shown high bond strength to dentin. Self-etch systems have been produced as an alternative to total-etch systems. A self-etch system contains a simultaneously acidic and hydrophilic monomer and does not need to be rinsed away after etching. Effective demineralization provides sufficient adhesive penetration into enamel and dentin.14 These bonding strategies might behave differently on dentine surfaces within pulp chambers altered by irrigants used during root canal treatment.
Some adhesive systems produce lower bond strengths to deep dentin.15,16 The dentin walls that make up the pulp chamber are the deepest possible dentin. Bonding to deep dentin has been more challenging than bonding to superficial dentin mainly due to the reduced area of solid intertubular dentin associated with the increased water content and large tubule diameters and high density.17,18 In addition, chemical irrigants used during root canal treatment may alter the chemical composition of dentin substrate and affect its interaction with materials used for coronal sealing. The adverse effects of irrigants such as sodium hypochlorite (NaOCl) on resin-dentin bond strength have been investigated and confirmed previously.19 Increased adhesive strength was reported when CHX was used at the coronal part, but investigation of bond strengths of adhesive materials to the pulp chamber dentin after the root canal treatment has not been performed extensively.6,12
The purpose of this in vitro study was to evaluate the influence of CHX on the microtensile bonds strength (µTBS) of resin core with two different adhesive systems to dentin in endodontic cavities. The null hypotheses tested were that: (1) CHX does not cause a detrimental effect on immediate µTBS to dentin; (2) CHX application does not influence µTBS after thermocycling, regardless of the adhesive categories (total-etch or self-etch system).
Forty freshly extracted caries-free molars, which had been stored in 0.1% thymol solution were used in this study. The occlusal enamel and dentin were ground flat using a model trimmer (Model Trimmer, Aurora Labs, Aurora, CO, USA) under running water up to expose the top of pulp chamber. The root of the specimen was removed from the crown approximately 2 mm below the cementoenamel junction using a slow-speed diamond saw under running water (Figure 1). To avoid touching pulpal wall dentin, the pulp tissue was removed carefully with a spoon excavator and a barbed broach. A flat cavity wall was made by Endo-Z bur with sprayed water. NaOCl 5.25% was applied to the all teeth pulp chamber for 40 minutes (this corresponds to the clinical time that irrigating substances are used in root canals during endodontic treatment) and rinsed with distilled water and completely air dried.20 Gutta-percha were wedged into the canal orifices without sealer, to serve as a stop against which the bonding agent could flow into.
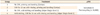
All the endodontic cavities were submitted to the bonding protocols using two-step total-etch adhesive system (Adper Single Bond 2, 3M ESPE, St. Paul, MN, USA), two-step self-etch adhesive system (Contax, DMG, Germany, pH = 3.5) and dual-cured composite (LuxaCore Dual Smartmix, DMG, Hamburg, Germany) was used as the core material in the pulp chamber. The materials used in this study and their compositions are listed in Table 1. The adhesive systems were applied to the pulp chamber walls of the teeth according to the manufacturers' directions.
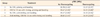
Forty teeth were randomly divided into 4 groups of 10 teeth each. Table 2 shows the experimental groups with their respective modalities.
In group 1, the dentin surfaces were primed with Contax-Primer and gently dried, after then, Contax-Bond was applied following the manufacturer's directions.
In group 2, the dentin surfaces were wetted with Consepsis, a 2% CHX cavity disinfectant for 15 seconds and rinsed with water and air-dried, then Contax was applied as the same manner in group 1.
In group 3, the dentin surfaces were acid-etched with 37% phosphoric acid and washed with water spray for 10 seconds and gently dried for 10 seconds and Single Bond was applied.
In group 4, the dentin surfaces were acid-etched with 37% phosphoric acid, rinsed off, air-dried as the same manner in group 3, then rewetted with Consepsis, a 2% CHX cavity disinfectant for 15 seconds. Afterwards, the Single Bond was applied.
Following the pre-treatment sequences of the individual groups, the cavities were filled with LuxaCore resin composite and they were polymerized for 40 seconds. Half of the specimens for each group were stored in water for 24 hours, and the other half of the specimens were then submitted to thermocycling of 10,000 cycles with temperature changing from 5 to 55℃, with a dwelling time for 15 seconds each and interval time for 10 seconds.
After 24 hours of storage in 37℃ water, cut the tooth in half across the furcation (Figure 2a). The restored specimens were serially sectioned into 1 mm thick dentin-resin slabs, and then rotated 90℃ and sectioned again to obtain resin-dentin sticks from the pulp chamber wall with a rectangular cross-sectional area of approximately 1 mm2 using diamond cutter (RB205 Metsaw-LS, TOPMET, R&B, Deajeon, Korea). One to two sticks were obtained from each restoration (Figure 2b). The bonded surface area was calculated before each test by measuring the narrowest portion with a digital caliper (Absolute digimatic 573, Mitutoyo, Kawasaki, Japan). The slabs were attached to a testing apparatus (Micro tensile tester, BISCO, Schaumburg, IL, USA) with cyanoacrylate adhesive (Zapit, DVA, Corona, CA, USA) applied to the composite and dentin sides of the slabs. After setting, they were subjected to tensile forces at a crosshead speed of 1 mm/min. The microtensile bond strengths were expressed into MPa.
To analyze the effect of adhesive resin categories and CHX treatment on bond strength before and after thermocycling, three-way ANOVA was used. Data were also analyzed with Scheffe post hoc test to determine any differences among groups. Another Independent t-test was also used. Statistical significance was pre-set at α = 0.05.
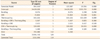
The results of the µTBS values (Table 3) and of three-way ANOVA (Table 4) are summarized. In this study, CHX and thermocycling treatment gave a great impact on the µTBS, while the type of adhesive system did not (Table 4). Only the interaction of CHX and thermocylcing treatment showed the significant difference among the interactions of three variables, such as CHX, thermocycling treatment and bonding system (Table 4).
There was no significant difference of bond strength among groups at the immediate testing period. However, after 10,000 cycles of thermocycling, all groups resulted in significant bond strength reduction (p < 0.05), although CHX treated groups showed lesser degree of reduction. This means that thermocycling deteriorated the bond strength of resin core system in endodontic cavity.
There was no significant difference of bond strength between groups without CHX treatment and groups with CHX pre-treatment at the immediate testing period. After 10,000 cycles of thermocycling, resulted in significant bond strength reduction in both groups irrespective of CHX treatment (p < 0.05), however, less decrease appeared in groups treated with CHX.
Sealing of the pulp chamber is an important factor that may influence the outcome of root canal treatment.21 Endogenous MMPs are found in dentin and their activation results in degradation of hybrid layers created by dentin adhesives.22 The most plausible explanation would be the inhibition of dentin matrix-bound MMPs, resulting in decreased degradation of hybrid layer and sub-hybrid layer collagen fibril.11 Therefore, MMPs in durability studies is an important issue to investigate, because this could be the key to increase the durability of restorations involving dentin bonding.
In the present study, since the application of CHX did not produce detrimental effect on bond strength of the specimens immediately submitted to µTBS test, the first hypothesis tested was supported. This was also observed in previous in vivo study.23 After 10,000 cycles of thermocycling, the groups treated with CHX showed significant reduction in bond strength compared to the immediate groups. However, this reduction was less than that of groups without CHX treatment, showing that CHX was able to diminish, but not completely eliminate the loss of bond strength over time. Therefore, the second hypothesis was rejected. Current study apparently indicates beneficial effects of CHX on the preservation of dentin bond strength.
CHX digluconate has the potential to minimize the reductions in the resin-dentin bond strengths commonly observed for simplified conventional adhesives after long-term water storage and also to preserve the morphological properties of hybrid layers by inhibiting host-derived proteases.12 Edermir et al. reported that endodontic irrigation with CHX solution significantly increased bond strength to root dentin.24 While in vitro study have suggested that the application of 2% CHX solution, a MMP inhibitor, was able to diminish the loss of µTBS over time associated to two-step etch-and-rinse and self-etch adhesive.25 The substantivity of CHX is related to the release of positively charged molecules from CHX treated surfaces and its ability to adsorb onto surfaces of the oral cavity.26 Theoretically, this can also occur in the demineralized exposed collagen fibrils, and is the explanation for the bonds being preserved after long-term water exposure. One may suggest that CHX is likely to bind to collagen fibrils at a very fast rate, and thus even short periods of time, such as 15 seconds, seem to be sufficient to guarantee such binding. This hypothesis was raised on the basis of the results of a recent investigation.26 Loguercio et al. demonstrated that the application time of CHX was reduced (15 seconds) and this reduction did not jeopardize the benefits of CHX in the preservation of dentin bonds.27 Therefore, application time for 15 seconds, was believed to be sufficient to preserve dentin bonds under the laboratory conditions in this study.
One of the two-step systems (Contax, pH = 3.5) is a self-etching bonding system which combines the etching and priming procedures into one step by a self-etching primer. An acidic monomer in the primer can demineralize the smear layer and the underlying dentin, resulting in mild etching. Another adhesive system (Single Bond) is a one-bottle system combining the priming and bonding procedures into one step. Phosphoric acid is used to remove the smear layer, and a moist dentin surface is required to maintain a non-collapsed demineralized collagen network mediated by hydrogen bonding of water.28 Once primer application of self-etching adhesive is performed without air-drying, collapse of collagen fibrils is avoided and the quality and integrity of the collagen available for resin infiltration may be of fundamental importance.29 It was known that CHX at 2% applied prior to self-etch adhesive system resulted in higher µTBS values.30 Ozturk and Ozer also showed self-etching priming systems showed the best performance on pulp chamber dentinal wall.31 The bonding interface of self-etch adhesives could be less affected by evaporative water flux during resin application due to their mild acid-etching effect. Moreover, mild acid-etching effect could lead to limited loss of inorganic matrix in the successively formed hybrid layer which has been verified to contribute to chemical bonding through the reaction with functional group of adhesive monomers.32 2% CHX application after acid-etching preserves both the durability of the hybrid layer and bond strength in vitro of aged specimens.33 Generally total-etch system showed high adhesive strength to dentin, but there was not much difference in adhesive strength between total-etch system and self-etch adhesive system in class I cavity. Self-etch adhesive systems were produced as an alternative for total-etch systems to reduce the technique sensitivity and application time. Systems employing a separate acid etching step are apparently more sensitive to dentin depth than are self-etching systems.17 For the total etch bonding agents, the assumption is that the acid etching process followed by rinsing may be capable of removing the dissolved mineral component of dentine and the remaining irrigating solutions or interaction byproducts. With self-etch dentine bonding system, the smear layer and any possible free or interacted residual chemical irrigant components may remain on the bonding site and be included in the hybrid layer.34 However, the weaker acidic primer in self-etching bonding systems results in less obvious change in the dentinal wall structure than the stronger total etch systems. These bonding strategies might behave differently on dentine surfaces within pulp chambers altered by irrigants used during root canal treatment.
Bonding to pulp chamber dentin was differently affected by the endodontic chemical irrigants. Sodium hypochlorite (NaOCl) has been extensively used in endodontic therapy to provide gross debridement, disinfection, lubrication, and dissolution of tissues.35 In this study, NaOCl was applied to reproduce similar clinical situation. This powerful antimicrobial agent had been previously shown to jeopardize the polymerization of bonding resins, because oxidizing effects of NaOCl and its reaction byproducts.25,26 They may cause inhibition of the interfacial polymerization of adhesives and possible dentinal surface contamination. Another speculation was that removal of collagen fibers from dentinal surfaces with NaOCl may have prevented creation of a healthy hybrid layer.31,36
In general, lower bond strengths were produced in deep dentin when compared with those produced in superficial dentin. These regional variation resulted in the variations in water content and dentinal permeability because of difference in the number of tubules per unit area.37
Although lots of studies showed the merits of CHX to pulp chamber wall dentin, in many in vitro studies, coronal dentin was used to test materials.2,25,31,36,38 However, for evaluation of adhesive cores, bonding to pulp chamber wall dentin is important to test. Therefore, pulp chamber wall dentin of teeth was used in this study as a bonding area. In this research, the application of 2% CHX to pulp chamber dentin reduce the decrease of resin-dentin bond strength for at least 10,000 cycles under the laboratory conditions. This result may be due to many factors that can influence the bonding performance of adhesive systems to dentin. Among these are the dentin substrate, the testing procedures, and the handling of the materials. Also lack of the simulation of pulpal pressure can be considered. So further in vivo studies are needed to clarify whether the use of 2% CHX solution to pulpal wall is able to preserve resin-dentin bonds after long-term function. It is hoped that the prospective development of adhesive resin systems and bonding techniques take into consideration the specific features of the pulp chamber substrate to achieve better bond strength.
Within the limitations of this in vitro study, 2% CHX application for 15 seconds proved to alleviate the decrease of bond strength of dentin bonding systems. There was no significant difference in microtensile bond strength between total-etching and self-etching systems. Based on the research, applying CHX for 15 seconds to endodontic cavity can be an effective way to get a relatively durable bond.
Figures and Tables
Figure 2
Specimen preparation for microtensile bond test. (a) Bonding substrate were restored with adhesive (sky blue) and composite (pink) to endodontic cavity wall (yellow); (b) Resin-dentin sticks with a rectangular cross-sectional area of approximately 1 × 1 mm.

References
1. Swanson K, Madison S. An evaluation of coronal microleakage in endodontically treated teeth. Part I. Time periods. J Endod. 1987. 13:56–59.

2. Kijsamanmith K, Timpawat S, Harnirattisai C, Messer HH. Micro-tensile bond strengths of bonding agents to pulpal floor dentine. Int Endod J. 2002. 35:833–839.

3. Weine FS. Nonsurgical re-treatment of endodontic failures. Compend Contin Educ Dent. 1995. 16:324326–335. quiz 335.
4. Eakle WS. Fracture resistance of teeth restored with class II bonded composite resin. J Dent Res. 1986. 65:149–153.

5. Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982. 16:265–273.

6. Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, Ito S. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004. 83:216–221.

7. Tjäderhane L, Larjava H, Sorsa T, Uitto VJ, Larmas M, Salo T. The activation and function of host matrix metalloproteinases in dentin matrix breakdown in caries lesions. J Dent Res. 1998. 77:1622–1629.

8. Sulkala M, Wahlgren J, Larmas M, Sorsa T, Teronen O, Salo T, Tjäderhane L. The effects of MMP inhibitors on human salivary MMP activity and caries progression in rats. J Dent Res. 2001. 80:1545–1549.

9. Martin-De Las Herasa S, Valenzuela A, Overall CM. The matrix metalloproteinase gelatinase A in human dentine. Arch Oral Biol. 2000. 45:757–765.

10. Bok YB, Lee DY, Lee CY, Kim KN, Kum KY. The sustaining effect of three polymers on the release of chlorhexidine from a controlled release drug device for root canal disinfection. J Korean Acad Conserv Dent. 2004. 29:548–554.

11. Gendron R, Grenier D, Sorsa T, Mayrand D. Inhibition of the activities of matrix metalloproteinases 2, 8, and 9 by chlorhexidine. Clin Diagn Lab Immunol. 1999. 6:437–439.

12. Hebling J, Pashley DH, Tjäderhane L, Tay FR. Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res. 2005. 84:741–746.

13. Kanca J 3rd. Improving bond strength through acid etching of dentin and bonding to wet dentin surfaces. J Am Dent Assoc. 1992. 123:35–43.

14. Kaaden C, Powers JM, Friedl KH, Schmalz G. Bond strength of self-etching adhesives to dental hard tissues. Clin Oral Investig. 2002. 6:155–160.

15. Suzuki T, Finger WJ. Dental adhesives: site of dentin vs. bonding of composite resins. Dent Mater. 1988. 4:379–383.
16. Pashley EL, Tao L, Matthews WG, Pashley DH. Bond strengths to superficial intermediate and deep dentin in vivo with four dentin bonding systems. Dent Mater. 1993. 9:19–22.

17. Yoshiyama M, Carvalho R, Sano H, Horner J, Brewer PD, Pashley DH. Interfacial morphology and strength of bonds made to superficial versus deep dentin. Am J Dent. 1995. 8:297–302.
18. Giannini M, Carvalho RM, Martins LR, Dias CT, Pashley DH. The influence of tubule density and area of solid dentin on bond strength of two adhesive systems to dentin. J Adhes Dent. 2001. 3:315–324.
19. Nikaido T, Takano Y, Sasafuchi Y, Burrow MF, Tagami J. Bond strengths to endodontically-treated teeth. Am J Dent. 1999. 12:177–180.
20. Farina AP, Cecchin D, Barbizam JV, Carlini-Júnior B. Influence of endodontic irrigants on bond strength of a self-etching adhesive. Aust Endod J. 2011. 37:26–30.

21. Hommez GM, Coppens CR, De Moor RJ. Periapical health related to the quality of coronal restorations and root fillings. Int Endod J. 2002. 35:680–689.

22. Tay FR, Pashley DH, Loushine RJ, Weller RN, Monticelli F, Osorio R. Self-etching adhesives increase collagenolytic activity in radicular dentin. J Endod. 2006. 32:862–868.

23. Carrilho MR, Geraldeli S, Tay F, de Goes MF, Carvalho RM, Tjäderhane L, Reis AF, Hebling J, Mazzoni A, Breschi L, Pashley D. In vivo preservation of the hybrid layer by chlorhexidine. J Dent Res. 2007. 86:529–533.

24. Erdemir A, Ari H, Güngüneş H, Belli S. Effect of medications for root canal treatment on bonding to root canal dentin. J Endod. 2004. 30:113–116.

25. Campos EA, Correr GM, Leonardi DP, Barato-Filho F, Gonzaga CC, Zielak JC. Chlorhexidine diminishes the loss of bond strength over time under simulated pulpal pressure and thermo-mechanical stressing. J Dent. 2009. 37:108–114.

26. Rosenthal S, Spångberg L, Safavi K. Chlorhexidine substantivity in root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 98:488–492.

27. Loguercio AD, Stanislawczuk R, Polli LG, Costa JA, Michel MD, Reis A. Influence of chlorhexidine digluconate concentration and application time on resin-dentin bond strength durability. Eur J Oral Sci. 2009. 117:587–596.

28. Kanca J 3rd. Effect of resin primer solvents and surface wetness on resin composite bond strength to dentin. Am J Dent. 1992. 5:213–215.
29. Frankenberger R, Perdigão J, Rosa BT, Lopes M. "No-bottle" vs "Multi-bottle" dentin adhesives-a microtensile bond strength and morphological study. Dent Mater. 2001. 17:373–380.

30. Mazzoni A, Pashley DH, Nishitani Y, Breschi L, Mannello F, Tjäderhane L, Toledano M, Pashley EL, Tay FR. Reactivation of inactivated endogenous proteolytic activities in phosphoric acid-etched dentine by etch-and-rinse adhesives. Biomaterials. 2006. 27:4470–4476.

31. Ozturk B, Ozer F. Effect of NaOCl on bond strengths of bonding agents to pulp chamber lateral walls. J Endod. 2004. 30:362–365.

32. Yuan Y, Shimada Y, Ichinose S, Tagami J. Effect of dentin depth on hybridization quality using different bonding tactics in vivo. J Dent. 2007. 35:664–672.

33. Butz F, Lennon AM, Heydecke G, Strub JR. Survival rate and fracture strength of endodontically treated maxillary incisors with moderate defects restored with different post-and-core systems: an in vitro study. Int J Prosthodont. 2001. 14:58–64.
34. Kazemi RB, Meiers JC, Peppers K. Effect of caries disclosing agents on bond strengths of total-etch and self etching primer dentin bonding systems to resin composite. Oper Dent. 2002. 27:238–242.
35. Spangberg L, Engström B, Langeland K. Biologic effects of dental materials. 3. Toxicity and antimicrobial effect of endodontic antiseptics in vitro. Oral Surg Oral Med Oral Pathol. 1973. 36:856–871.
36. Santos JN, Carrilho MR, De Goes MF, Zaia AA, Gomes BP, Souza-Filho FJ, Ferraz CC. Effect of chemical irrigants on the bond strength of a self-etching adhesive to pulp chamber dentin. J Endod. 2006. 32:1088–1090.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download