Abstract
Objectives
New resin cement (NRC) has been developed as a root repairing material and the material is composed of organic resin matrix and inorganic powders. The aim of this study was to compare the rat subcutaneous tissue response to NRC and mineral trioxide aggregate (MTA) cement and to investigate the tissue toxicity of both materials.
Materials and Methods
Sixty rats received two polyethylene tube-implants in dorsal subcutaneous regions, MTA and NRC specimens. Twenty rats were sacrificed respectively at 1, 4 and 8 wk after implantation and sectioned to 5 µm thickness and stained with Hematoxylin-Eosin (H-E) or von-Kossa staining. The condition of tissue adjacent to the implanted materials and the extent of inflammation to each implant were evaluated by two examiners who were unaware of the type of implanted materials in the tissues. Data were statistically analyzed with paired t-test (p < 0.05).
Results
In specimens implanted with both NRC and MTA, severe inflammatory reactions were present at one wk, which decreased with time. At eighth wk, MTA implanted tissue showed mild inflammatory reaction, while there were moderate inflammatory reactions in NRC implanted tissue, respectively. In NRC group, von-Kossa staining showed more calcification materials than MTA group at eighth wk.
In spite of high success rate in saving teeth by endodontic therapy, conventional endodontic treatment is not always successful.1 Endodontic surgery is performed to resolve periapical inflammations that cannot be favorably treated by conventional endodontic procedures.2 Currently, mineral trioxide aggregate (MTA) cement has been most widely used as root end filling material in apical surgery.3 However, some researchers have offered negative opinions as to whether MTA is really superior to other materials in physical properties. MTA is not easy to handle, and it takes a very long time to set.4,5 An ideal root-end filling should have good biocompatibility, apical sealability, easy handling properties, and long-term clinical success.6 Unfortunately, there is no ideal material which fulfills all of these properties.
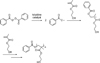
Recently, a novel resin based root-end filling material (termed New resin cement, NRC) has been introduced and the physical properties and cytotoxicity were investigated.7 Compare to MTA which is a mixture of bismuth oxide and contains trace amounts of SiO2, CaO, MgO, K2SO4, and Na2SO4, NRC is composed of HEMA-based resin matrix and inorganic powders as fillers.8 It contains bioactive powders such as calcium oxide and calcium silicate, triphenylbismuth carbonate as opacifier. Organic resin matrix of this cement is composed of 2-hydroxyethylmethacrylate (HEMA) as a resin monomer, benzoyl peroxide as an initiator, toluidine and toluenesulfinate as catalyst and accelerator.7 The probable polymerization reaction of NRC is shown at Figure 1.
According to the results of previous study as to the setting time, compressive strength, pH and cytotoxicity of NRC, it has the possibility to be a suitable root-end filling material. However, there are a few studies until now about this material. The aim of this study was to compare the rat subcutaneous tissue response to NRC and MTA cement and to investigate the tissue toxicity of both materials.
The animal experimental protocol was approved by the Animal Research Committee of Asan Medical Center (2009-14-163, Seoul, Korea), and all ethical criteria contained in Helsinky declaration were followed. NRC samples were prepared following the method previously mentioned in 2009 by Kim et al.7 In brief, the powder component of NRC was mixed with liquid prepared from mixture A and B. Mixture A contains HEMA and benzyl peroxide, and mixture B consists of HEMA, toluidine, and toluenesulfinate. A total of 0.6 g powder was mixed with 150 µL mixture A and mixture B on a glass plate using a metal spatula. Specimens of white MTA cement (Dentsply, Tulsa, OK, USA) were prepared according to the manufacturer's instructions and used as a control groups.
Sixty male Sprague-Dawley rats, 8 weeks old, 230 - 280 g weighed, were housed in metal cage at a constant temperature of 24℃ with commercial rat chow available ad libitum. Anesthesia of the rat was obtained using combination of Zoletil (40 mg/kg IM, Virbac, Carros, France), Xylazine hydrochloride (10 mg/kg, Bayer korea co., Seoul, Korea) and 2% Xylocaine (Including 1/100000 epinephrine, Astra, MA, USA). Sixty polyethylene tubes with 5 mm internal diameter, 5.6 mm external diameter and 8 mm length were filled with test materials. For moist curing the samples were then placed in a heating chamber for 24 hours at 37℃ and 100% relative humidity. Each rat received two implants in dorsal subcutaneous regions; white MTA and NRC specimens. Twenty rats were sacrificed respectively at 7 days, and 4 and 8weeks after implantation. They were sacrificed by CO2-euthanasiabital device, and then implant areas were carefully excised and fixed in formaldehyde.
Block biopsies around implant were sectioned in 5 mm width with sharp knives and dehydrated in alcohol, embedded in paraffin, serially sectioned to 5 µm thickness and stained with Hematoxylin-Eosin (H-E) or von-Kossa staining. Tissue preparations were histologically evaluated under light microscope (Olympus DP-70, Tokyo, Japan).
The type of tissue adjacent to the implanted materials, the extent of inflammation, predominant cell types in tissue, calcification and fibrous connective tissue formation or not next to each implant were evaluated by two examiners who were unaware of the type of implanted materials in the tissues. The H-E stained histological sections were scored as follows according to previous studies.9-11 Grade zero presented none or few inflammatory cells and no reaction, and grade 1 meant less than 25 cells mild reaction and grade 2 showed 25 - 125 cells and moderate reaction in tissues. Also, grade 3 determined more than 125 cells and severe reaction in microscopic examination. To grade the inflammatory reaction, five high-power magnification fields were scanned from all slides. Thus the cell number was counted within a grid per high-power fields as described by Morse et al.12 Necrosis and calcification were recorded as present or absent. Data were statistically analyzed with paired t-test. The level of significance for the overall differences is set at p < 0.05.
At seven days, most of NRC and MTA groups showed severe inflammatory reaction. The heavily inflammed tissues were composed of many infiltrated inflammatory cells such as lymphocytes, macrophages and plasma cells (Figures 2a, 2b, 3, and 4). They showed large areas of tissue necrosis. However, the severe reactions decreased with time in specimens of both group. At 4 weeks, some healed lesions were observed, but granulation tissue and inflammatory area were remained in most of histologic specimens (Figures 2c, 2d, 5, and 6). Remnants of test implant were surrounded by fibrous tissue.
At 8 weeks, MTA group showed mild inflammatory reactions, while NRC group presented moderate reaction with chronic inflammatory cells remained around the particles of the material (Figures 2e, 2f, 7, and 8). In 8 weeks specimens with von-Kossa staining, more mineralization spots were observed in NRC than MTA group (Figure 9). Sometimes, remnants of test implant surrounded by fibrous tissue and dystrophic calcium particles in macrophages and vessels were observed (Figures 10 and 11).
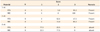
The inflammatory scores of each material and time are presented in Table 1. Statistical analysis of the data was done with the paired t-test. The level of significance for the overall differences was set at p < 0.05. There were no statistically significant differences of scores between MTA and NRC group at 1st week. Both showed severe inflammatory reaction. However, there were significant differences between MTA and NRC in 4 and 8 weeks groups. MTA group showed moderate inflammatory reaction, while NRC group showed severe reaction at 4 weeks. At 8 weeks, MTA showed mild inflammatory reaction while NRC presented moderate reaction.
Biocompatibility of endodontic materials is characterized by many parameters such as genotoxicity, mutagenicity, cytotoxicity, and histocompatibility. It is generally accepted that subcutaneous implantation study using small animal models is suitable to assess the effects of biomaterials preliminarily.12 Since the introduction by Torneck in 1966, the efficacy of this method was revised and substantiated by Olsson et al.13,14 and this has been one of the most common and appropriate methods to evaluate dental materials.15 According to Olsson et al., the placement of an experimental material in a polyethylene tube before implantation prevents the diffusion of the material into the connective tissue, which simulates the situation in the root canal.14 However, due to small areas of recipient site, negative control groups could not be determined. Despite of the absence of negative control groups, many studies have been reported the difference between empty polyethylene tube and MTA filled tube.15-17 Due to the difficulties of handling both materials and small sizes of recipient site, we had implanted the two polyethylene tubes. Recently, a trend towards orthograde filling of MTA in whole root canals might influence on our experimental design.18-20 We expected that a large amount of MTA fillings might induce exaggerated the tissue reaction.
The rat subcutaneous tissue responses to implantation of MTA were consistent with the results of previous investigations, and the responses to NRC also showed similar degree and tendency although the inflammatory scores were not as good as MTA.16 However, it was somewhat different result from the previous study, which demonstrated less cytotoxicity of NRC than MTA as evaluated MTT assay.7 It is suggestive that direct comparison between other studies may be limited because of different study designs. The dimethyl-thiazol-diphenyltetrazolium bromide (MTT) assay in previous study was in vitro study using MC3T3-E1 cells, whereas in this study, rat subcutaneous tissue reactions with different stimulation time were histologically evaluated.
All specimens in the present study showed less severe inflammation at longer time intervals (4 and 8 weeks) compared to one week significantly. Tissue necrosis observed in one week and 4 weeks specimen could not be found in 8 weeks specimen. Because later harmful effects of a material are considered to be more important than its initial effects, the gradual decrease of inflammation score and tissue necrosis with the lapse of time is indicative of promising properties as a root end filling material.10 Both MTA and NRC are strong alkaline substances, which have a pH of approximately 12.5.7 In early period, the strong alkalinity may influence the tissue toxicity. However, the high pH may also means to stimulate mineralization via calcium and hydroxyl ion release and activation of alkaline phosphatase, which plays an important role in hard tissue formation.21 This was proved by the histologic findings of responses to both materials at 8 weeks, which showed calcified materials and dystrophic calcium particles with von-Kossa staining.
It was reported that MTA has the ability to encourage hard-tissue deposition particularly cementogenesis.11,17 Also Asgary et al. reported that MTA release sufficient calcium ions which can react with environmental phosphate and produce hydroxyapatite.22 And cementogenic or dentinogenic activity of MTA may be due to this physicchemical reaction. Calcium is a well-known regulator of transcriptional gene expression in osteoblasts, and many cellular responses to calcium signals are modulated by calcium/calmodulin dependent enzymes, although the role of calcium in cementoblastic differentiation is not known.23 Paula-Silva et al. reported that calcium hydroxide increases in extracellular calcium levels induced cementoblastic differentiation of PDL cells.24
Von-Kossa staining is for demonstrating deposits of calcium or calcium salt so it is not specific for the calcium ion itself. In this staining, tissue sections are treated with a silver nitrate solution and the silver is deposited by replacing the calcium reduced by the strong light, and thereby visualized as metallic silver.25 The von-Kossa staining results of MTA in this study agreed with the result reported by Holland et al., and the von-Kossa positive tissue structures were more evident with NRC than MTA.26 We may assume that this result has some relation to the manner of release of calcium ions from these materials. From the results of this study, NRC demonstrated promising result as a calcium reservoir material. Further studies about the other behaviors and mechanisms of action of this material will be necessary.
Figures and Tables
Figure 2
Representative histologic characteristics of each group. (a) 1 week MTA; (b) 1 week NRC; (c) 4 weeks MTA; (d) 4 weeks NRC; (e) 8 weeks MTA; (f) 8 weeks NRC. Black arrow shows area of inflammatory reaction (H-E, ×40). MTA, mineral trioxide aggregate; NRC, new resin cement.

Figure 3
The histologic specimen of 1 week MTA (H-E, ×200). Black arrow shows inflammatory cells. MTA, mineral trioxide aggregate.
Figure 4
The histologic specimen of 1 week NRC (H-E, ×200). There are many inflammatory cells on the border of the material (Black arrow). NRC, new resin cement.
Figure 5
The histologic specimen of 4 weeks MTA (H-E, ×200). Calcified materials are encapsulated and surrounded by inflammatory cells (Black arrow). MTA, mineral trioxide aggregate.
Figure 6
The histologic specimen of 4 weeks NRC (H-E, ×200). Calcified materials are surrounded by inflammatory cells (Black arrow). NRC, new resin cement.
Figure 7
The histologic specimen of 8 weeks MTA (H-E, ×200). Calcified particles are surrounded with chronic inflammatory cells (Black arrow). MTA, mineral trioxide aggregate.
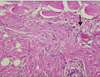
Figure 8
The histologic specimen of 8 weeks NRC (H-E, ×200). There are some inflammatory cells under the materials (Black arrow). NRC, new resin cement.
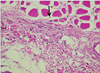
Figure 9
Histologic specimen of (a) 1 week MTA; (b) 1 week NRC; (c) 4 weeks MTA; (d) 4 weeks NRC; (e) 8 weeks MTA; (f) 8 weeks NRC. Black arrow shows calcified materials (von-Kossa, ×40). MTA, mineral trioxide aggregate; NRC, new resin cement.

Figure 10
Dystrophic calcium particles in blood vessels (8 weeks MTA, von-Kossa, ×100). MTA, mineral trioxide aggregate.

Notes
References
1. Imura N, Pinheiro ET, Gomes BP, Zaia AA, Ferraz CC, Souza-Filho FJ. The outcome of endodontic treatment: a retrospective study of 2000 cases performed by a specialist. J Endod. 2007. 33:1278–1282.

2. McDonald NJ, Hovland EJ. Walton RE, Torabinejad M, editors. Surgical endodontics. Principles and practice of endodontics. 1996. 2nd ed. Philadelphia, PA: W.B. Saunders Co.;401–422.
3. Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod. 1993. 19:541–544.

4. Lee YL, Lin FH, Wang WH, Ritchie HH, Lan WH, Lin CP. Effects of EDTA on the hydration mechanism of mineral trioxide aggregate. J Dent Res. 2007. 86:534–538.

5. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review-Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010. 36:400–413.

6. Johnson BR. Considerations in the selection of a root-end filling material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 87:398–404.

7. Kim M, Ko H, Yang W, Lee Y, Kim S, Mante FK. A new resin-bonded retrograde filling material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 108:e111–e116.

8. Roberts HW, Toth JM, Berzins DW, Charlton DG. Mineral trioxide aggregate material use in endodontic treatment: a review of the literature. Dent Mater. 2008. 24:149–164.

9. Gomes-Filho JE, Rodrigues G, Watanabe S, Estrada Bernabé PF, Lodi CS, Gomes AC, Faria MD, Domingos Dos Santos A, Silos Moraes JC. Evaluation of the tissue reaction to fast endodontic cement (CER) and Angelus MTA. J Endod. 2009. 35:1377–1380.

10. Yaltirik M, Ozbas H, Bilgic B, Issever H. Reactions of connective tissue to mineral trioxide aggregate and amalgam. J Endod. 2004. 30:95–99.

11. Holland R, de Souza V, Nery MJ, Otoboni Filho JA, Bernabé PF, Dezan Júnior E. Reaction of rat connective tissue to implanted dentin tubes filled with mineral trioxide aggregate or calcium hydroxide. J Endod. 1999. 25:161–166.

12. Morse DR, Wilcko JM, Pullon PA, Furst ML, Passo SA. A comparative tissue toxicity evaluation of the liquid components of gutta-percha root canal sealers. J Endod. 1981. 7:545–550.

13. Hammad HM, Hamadah MA, Al-Omari WM. Histological evaluation of rat tissue response to GMTA, Retroplast, and Geristore retrograde filling materials. Aust Endod J. 2011. 37:18–25.

14. Torneck CD. Reaction of rat connective tissue to polyethylene tube implants. I. Oral Surg Oral Med Oral Pathol. 1966. 21:379–387.
15. Olsson B, Sliwkowski A, Langeland K. Subcutaneous implantation for the biological evaluation of endodontic materials. J Endod. 1981. 7:355–367.

16. Parirokh M, Mirsoltani B, Raoof M, Tabrizchi H, Haghdoost AA. Comparative study of subcutaneous tissue responses to a novel root-end filling material and white and grey mineral trioxide aggregate. Int Endod J. 2011. 44:283–289.

17. Shahi S, Rahimi S, Lotfi M, Yavari H, Gaderian A. A comparative study of the biocompatibility of three root-end filling materials in rat connective tissue. J Endod. 2006. 32:776–780.

18. Mohammadi Z, Yazdizadeh M. Obturation of immature non-vital tooth using MTA. Case report. N Y State Dent J. 2011. 77:33–35.
19. Witherspoon DE, Small JC, Regan JD, Nunn M. Retrospective analysis of open apex teeth obturated with mineral trioxide aggregate. J Endod. 2008. 34:1171–1176.

20. Jung IY, Kim ES, Lee CY, Lee SJ. Continued development of the root separated from the main root. J Endod. 2011. 37:711–714.
21. Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP. Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys. J Endod. 1997. 23:225–228.

22. Foreman PC, Barnes IE. Review of calcium hydroxide. Int Endod J. 1990. 23:283–297.
23. Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J. Effect of two storage solutions on surface topography of two root-end fillings. Aust Endod J. 2009. 35:147–152.

24. Zayzafoon M. Calcium/calmodulin signaling controls osteoblast growth and differentiation. J Cell Biochem. 2006. 97:56–70.

25. Paula-Silva FW, Ghosh A, Arzate H, Kapila S, da Silva LA, Kapila YL. Calcium hydroxide promotes cementogenesis and induces cementoblastic differentiation of mesenchymal periodontal ligament cells in a CEMP1- and ERK-dependent manner. Calcif Tissue Int. 2010. 87:144–157.

26. Sheehan D, Hrapchak B. Theory and practice of histotechnology. 1980. 2nd ed. Columbus, Ohio: Battelle Press;226–227.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download