Abstract
Traumatic injuries of the face often involve root fractures especially in anterior teeth. The prognosis and the treatment of the root fracture depend on the extent of the fracture line, general health and patient compliance. This case report outlines a new conservative trial treatment modality to stabilize the maxillary central incisors with horizontal root fracture on the cervical to middle third by fabricating canine guidance to remove loading on the traumatized maxillary central incisors during eccentric movements and thus inducing spontaneous healing of the fractured line between the fragments. Radiographs after thirty months showed adequate healing with no signs of pathological changes including root resorption, ankylosis or displacement. Long term follow-up revealed that vitality, stability and aesthetics were maintained and the patient was satisfied with the outcome.
Traumatic injuries to teeth caused by accidents or sport injuries are a common occurrence encountered by dental practitioners. Maxillary incisors are most frequently affected in such cases, often presenting with signs ranging from uncomplicated crown fractures to complicated crown root fractures, avulsion or intrusion, depending on the severity of the injury. The incidence of horizontal root fracture comprises 0.5 - 7% of injuries affecting permanent teeth.1 Horizontal root fractures frequently occur in the middle third of the root, followed by apical and cervical regions.2 When a root fractures horizontally, the coronal segment is displaced to a varying degree, but generally the apical segment is not displaced. As the apical pulpal circulation is not disrupted, there is an extremely low occurrence of pulp necrosis in the apical segment. The coronal segments fail to maintain vitality and become necrotic in about 25% of horizontal root fracture cases.3 The location of root fracture was shown to be the best indicator of tooth survival. Fractures of the cervical third of the root were found to have the worst prognosis because of decreased stability of coronal fragment and loss of vitality.4
Treatment options with root fractures typically include reduction of the fractured fragments and stabilization by rigid fixation for a variable time.5 This case report presents the successful management of traumatized maxillary central incisors with horizontal fracture lines between the middle and cervical third of the root by fabrication of canine protected occlusion with composite resin to remove loading on the traumatized maxillary central incisors during eccentric movements.
A 49 year-old male patient presented to the urgent care clinic, Korea University dental hospital, with the complaint of slightly mobile maxillary central incisors due to a fall while exercising on the treadmill that happened one day prior to his visit. The patient's medical history was unremarkable.
The extraoral examination revealed abrasion of the chin and contusion of the upper lip. The intraoral clinical examination showed uncomplicated enamel-dentine fracture of the maxillary right canine and lateral incisor. The maxillary central incisors exhibited enamel chipping as well as many superficial enamel craze lines, and grade 1 to 2 mobility. The surrounding periodontal tissue was slightly erythematous in the cervical area of both maxillary central incisors. He had bruises and superficial lacerations on the inner surface of the upper lip. Horizontal fracture lines were radiographically evident between the middle third and the cervical third of the maxillary central incisors (Figure 1).
Otherwise, the status of the traumatized teeth was within normal limits in terms of periodontal pocket, vitality on thermal and electrical test. For the management of soft tissue injuries, analgesic (Ibuprofen 400 mg) and antibiotic (amoxicillin 500 mg) were prescribed to take 3 times a day for the period of 3 adjustment of the opposing mandibular incisors was carried out to eliminate interference on the traumatized incisors in maximum intercuspation. The patient was advised to have a soft diet and avoid loading on the anterior teeth until the teeth become clinically stable. The patient was then referred to the Department of Conservative Dentistry, Korea University Dental Hospital for the management of the maxillary central incisors with horizontal root fractures and the maxillary right lateral incisor and canine with crown fracture. Ten days later, on his first visit to the Department of Conservative Dentistry, slightly increased patient's discomfort and visibly increased mobility of the maxillary central incisors were observed on protrusion and lateral excursion. Composite resin Filtek Z-250 (3M ESPE, St. Paul, MN, USA) was used to repair enamel chipping of the maxillary central incisors, the mesial tip of the maxillary right canine. The fractured incisal third of the maxillary right lateral incisor was restored with composite resin over resin-modified glass ionomer (RMGI) material FUJI II LC (GC, Tokyo, Japan) (Figure 2). In an attempt to eliminate loading on the traumatized maxillary central incisors upon unavoidable eccentric movements during function, the same composite resin material was added on the maxillary canines establishing canine protected occlusion (Figure 3). Contact points were marked with the articulating paper in centric occlusion. Composite resin was added incisal to the contact points marked on the occlusal surfaces of the maxillary canines. Selective adjustment of the composite resin build ups was carried out until uniform lines were marked on the resin during lateral excursion and until any interference on the damaged teeth in centric occlusion and during eccentric movement was not marked on the articulating paper. Calculus removal was carefully performed on the same visit to help maintain periodontal health. The patient returned for periodic monthly follow up for 4 month and 3 month follow up for next 2 years. At every recall, the teeth were clinically evaluated for vitality using an electric pulp tester (Digitest, Parkell, Farmingdale, NY, USA), thermal response to cold, pocket depth, percussion, mobility and occlusion, and periapical status with radiographs. After the construction of canine protected occlusion using composite resin, there was a gradual increase in comfort experienced by the patient owing to declining tooth mobility. At 4 month recall, the mobility of both maxillary central incisors exhibited in the range of physiological allowance and the patient did not report any discomfort associated with the injured teeth. At follow up 30 months later, the vitality, stability and esthetics of the maxillary central incisors were maintained (Figure 4). Despite the presence of noticeable discontinuation of the outlines of the maxillary central incisors between the middle and cervical third root, an increase in the density of the alveolar bone between the root fragments was observed. Radiographically, there were no signs of pathological changes including root resorption or ankylosis (Figures 5 and 6).
Root fractures are usually a result of impact that creates compression zones labially or lingually resulting in chipping, dislocation of the fragment or mobility.6 The prognosis of a root fracture depends on the extent of the fracture line, pulp tissue situation, stage of root formation, dislocation of fragments and the general health of the patient.7 Treatment of root fractures requires a multidisciplinary approach that involves stabilization of the fractured segment followed by a combination of endodontic, orthodontic and prosthodontic treatment, which could be time consuming to achieve desired results and results depends on patient compliance. With regard to the healing and prognosis of teeth, it has been reported that fracture type, treatment delay, splinting and duration of fixation were not significantly related to healing while maturity of root, type of injury, diastasis between the fragments were factors that contributed to frequency and type of healing.5 The repair of fracture line depends on the status of periodontal ligament and tissue, from which the hard tissue forming cells for odontoblastic and odontoclastic activity originate.8 In this case, no significant pathological changes were observed in surrounding periodontal tissue except slightly erythematous in cervical area of both maxillary central incisors and the clinical and radiographic observation demonstrated functional fractured roots. The treatment modality chosen in the present case utilized composite resin material to construct canine protected occlusion, thus precluding detrimental movement of the coronal fragments induced by interference during eccentric movements. The rationale of the chosen approach was based on that mobility of the coronal fragment is a clear negative influence upon healing as increased mobility disrupts healing of periodontium and pulp.9 A silicone putty index is a very useful guide that is created over the template on the diagnostic cast as a guide for finished restorations. However, a silicone putty index was not utilized in this case, as it was felt to some degree that impression taking procedure of the traumatized teeth might have disrupted the healing potential.
With regards to the use of RMGI on exposed dentin, despite significant advancements in the development of dentin bonding agents, bonding to dentin is still considered unpredictable. In the present case, RMGI was placed over the exposed dentin surface on the maxillary right lateral incisor beneath composite resin restorations. RMGIs have hydrophilic qualities, therapeutic fluoride release effect, lower thermal expansion, and setting shrinkage. Besides, RMGI can adhere to both tooth structure and composite resin by chemical and micromechanical adhesion. Although, controversy remains regarding the use of RMGI liner, it may have several benefits in the placement of direct composite resins for potentially improved longevity of the restoration where a decrease in the volume of composite resin can reduce interfacial stresses.10
The exposed dentin of the maxillary right lateral incisor was untreated on his first visit to the urgent care clinic as the patient did not complain of accompanying tooth sensitivity and did not seek immediate care of the maxillary right lateral incisor except horizontally root fractured maxillary central incisors. Nevertheless, immediate dentin sealing using either a dentin boning agent or liner should be done as a primary preventive intervention, whenever possible, in order to minimize potential adverse pulpal sequelae due to the exposure of dentin.
There are four types of root fracture healing patterns according to Andreasen and Hjorting-Hansen: Type 1- Healing with interposition of hard tissue: healing with hard tissue, fragments are in close contact and the fracture line is not visible or indistinctly outlined, Type 2- Healing with interposition of bone and soft tissue between the fragments: fragments are separated by ingrowth of hard tissue surrounded by periodontal ligaments like tissue, Type 3- Healing with interposition of soft tissue: fragments are close but separated by a distinct radiolucent line and there is rounding up of the fracture edges, Type 4- No healing: persistent or a widened space between the fragments and the presence of a radiolucency in the alveolar bone adjacent to the root fracture.8 Periapical radiograph and cone beam CT of this case showed a healing pattern in the range of type 1 and 2 that are considered to be variations of the same healing pattern and are regarded as a successful healing pattern. The primary approach in the management of root fracture involves repositioning of the coronal fragment and stabilization with splinting. However, no attempt was made to maneuver their coronal fragments to their original position in this case to prevent possible further damage to their periodontium as the patient could not notice any change in position, and the slight diastasis between the root fragments would not readily be reduced due to the presence of blood clots as a result of late visit 24 hours post injury to the clinic. Root canal therapy was not carried out as the fracture line in this case did not communicate with the oral cavity and positive response on thermal and electrical testing was within normal limits. The maxillary central incisors were not splinted since there was no marked increased mobility. It has also been suggested that splinting procedure may contribute additional trauma during splint application, impair oral hygiene, and impede natural healing due to restriction of mobility causing reduced circulation. The purpose of fabrication of canine protected occlusion with composite resin was to disocclude the damaged maxillary central incisors to allow spontaneous healing of the fractured line preferably by interposition of hard tissue between the fragments and provide adequate stability between the teeth and the surrounding periodontal ligament while allowing physiological movement.
Healing of horizontal root fractures without treatment has been reported in many cases. This case described successful management of horizontal root fracture by conservative approach using composite resin. Long term follow up revealed that vitality, stability and aesthetics were maintained and patient was satisfied with the outcome.
Figures and Tables
Figure 1
Periapical radiograph showing horizontal root fractures of both maxillary central incisors.
Note visible gap between middle and cervical third of the maxillary central incisors.
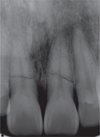
Figure 2
Radiographs showing crown fractures of the maxillary right lateral incisor and canine. (a) initial; (b) after composite resin build-up.
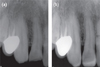
Figure 3
After restoration of the maxillary right lateral incisor, and compostie resin overlay on both maxillary canines. (a) anterior view; (b) articulating paper marking of eccentric movements after fabrication of canine protected occlusion using composite showing no contact on the traumatized central incisors.

Figure 4
Thirty-months follow-up. (a) anterior view showing good aesthetics; (b) occlusal view showing functional composite overlay on the maxillary canines.

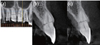
Figure 5
Periapical radiograph after 30 months showing healing and reduced gap between the fracture lines.

Figure 6
Coronal and cross-sectional CBCT images of spontaneously healed root fractures of the central incisors without any signs of periradicular pathology or root resorption. (a) Coronal image; (b) Cross-sectional image of the maxillary right central incisor; (c) Crosssectional image of the maxillary left central incisor. CBCT, Cone-beam computed tomography.
References
1. Andreasen FM, Andreasen JO. Andreasen JO, Andreasen FM, editors. Root fractures. Textbook and color atlas of traumatic injuries to the teeth. 1994. 3rd ed. Copenhagen: Munksgaard;279–314.
2. Calişkan MK, Pehlivan Y. Prognosis of root-fractured permanent incisors. Endod Dent Traumatol. 1996. 12:129–136.

3. Andreasen FM, Andreasen JO, Bayer T. Prognosis of root-fractured permanent incisors-prediction of healing modalities. Endod Dent Traumatol. 1989. 5:11–12.
4. Welbury R, Kinirons MJ, Day P, Humphreys K, Gregg TA. Outcomes for root-fractured permanent incisors: a retrospective study. Pediatr Dent. 2002. 24:98–102.
5. Cvek M, Mejàre I, Andreasen JO. Healing and prognosis of teeth with intra-alveolar fractures involving the cervical part of the root. Dent Traumatol. 2002. 18:57–65.

6. Rintaro T, Kiyotaka M, Minoru K. Conservative treatment for root fracture located very close to gingiva. Dent Traumatol. 2005. 21:111–114.

7. Andreasen JO, Bakland LK, Flores MT, Andreasen FM, Andersson L. Epidemiology of traumatic dental injuries. Traumatic dental injuries - a manual. 2003. 2nd ed. Oxford: Blackwell Munksgaard;10–15.
8. Andreasen JO, Hjorting-Hansen E. Intraalveolar root fracture: radiographic and histologic study of 50 cases. J Oral Surg. 1967. 25:414–426.
9. Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 1. Effect of pre-injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent Traumatol. 2004. 20:192–202.

10. Wakefield CW, Kofford KR. Advances in restorative materials. Dent Clin North Am. 2001. 45:7–29.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download