Abstract
Objectives
The maintenance of the healthy periodontal ligament cells of the root surface of donor tooth and intimate surface contact between the donor tooth and the recipient bone are the key factors for successful tooth transplantation. In order to achieve these purposes, a duplicated donor tooth model can be utilized to reduce the extra-oral time using the computer-aided rapid prototyping (CARP) technique.
Materials and Methods
Briefly, a three-dimensional digital imaging and communication in medicine (DICOM) image with the real dimensions of the donor tooth was obtained from a computed tomography (CT), and a life-sized resin tooth model was fabricated. Dimensional errors between real tooth, 3D CT image model and CARP model were calculated. And extra-oral time was recorded during the autotransplantation of the teeth.
Results
The average extra-oral time was 7 min 25 sec with the range of immediate to 25 min in cases which extra-oral root canal treatments were not performed while it was 9 min 15 sec when extra-oral root canal treatments were performed. The average radiographic distance between the root surface and the alveolar bone was 1.17 mm and 1.35 mm at mesial cervix and apex; they were 0.98 mm and 1.26 mm at the distal cervix and apex. When the dimensional errors between real tooth, 3D CT image model and CARP model were measured in cadavers, the average of absolute error was 0.291 mm between real teeth and CARP model.
Autogenous tooth transplantation is a viable option for replacing missing teeth when donor teeth are available. Wisdom teeth have traditionally been extracted due to concerns that this tooth might cause inflammation of the surrounding tissue, which is true when the tooth is not properly positioned. However, many well-erupted wisdom teeth can later be used as a donor for a missing tooth.1
However, unlike the soft tissue organs, hard tissue transplantation such as teeth requires a procedure for contouring the recipient bone in order for the donor tooth to sit properly in the recipient site. The tooth root is covered with a thin layer of connective tissue, which is known as the periodontal ligament. The presence of intact and viable periodontal ligament cells on the root surface of a donor tooth is most important for the healing of transplanted teeth.2 Several factors affecting the periodontal ligament healing include the extra-oral time of the donor tooth, the storage method until transplant, surgical trauma, and contamination of the root surface and/or root canal. Among those, the extra-oral time of the donor tooth prior to transplantation has the most significant effect on the success rate.3 In clinics, it is frequently found that the extended extra-oral time of the donor tooth causes severe root resorption (Figure 1).
Another important factor in tooth transplantation is the distance between the recipient bone tissue and the root surface of the transplanted tooth. Optimal contact with the recipient site can improve the level of blood supply and nutrients to the periodontal ligament cells, which can improve the success rate of the tooth transplantation.4
The major problem in tooth transplantation is how to precisely contour the recipient alveolar bone to fit the donor tooth in such a limited time so as to prevent the cell death of the root surface. Previously, most of the donor teeth were extracted first, and then used as templates for contouring of the recipient bone, which involved a process of trial and error for fitting. Multiple insertions of the extracted donor tooth in a prepared socket would not only result in an extended extra-oral time but damage the root cells of the donor tooth, which can lead to failure. If a duplicated tooth model that has exactly the same shape and size as the donor tooth can be obtained, the recipient bone cavity can be prepared using this model tooth prior to extraction, which can avoid the complications arising from multiple trials of real donor tooth.
The computer-aided rapid prototyping (CARP) technique was first introduced in mechanical engineering and has been used mainly to pre-evaluate the procedures for assembling and manufacturing designed products ahead of actual production. It has gained a great amount of attention in clinical medicine, particularly in oral maxillofacial surgery for simulating orthognatic surgery. In a comparison of a dry skull and RP model, Choi et al. and Lill et al. reported 0.64 mm and 1.47 mm discrepancies, respectively.5,6 In teeth, the discrepancy was 0.291 mm on average.7 With the aid of this new technology, this study fabricated a duplicated donor tooth before extraction the tooth using a CT data and visualization program.8
The aims of this paper are two folds, first, how to reduce the extra-oral time and secondly, how to secure an optimal contact between the donor tooth and the recipient bone using the CARP model in autogenous tooth transplantation. This paper consists of two experimental procedures, one is in vivo cases in which autogenous tooth transplantation were performed with CARP technique, two is in vitro experiment to evaluate the dimensional errors between real tooth, 3D CT image and CARP model using two maxilla and two mandible cadaver block bones.
A total of 182 patients (80 males and 102 females) who received a wisdom tooth transplant at the Dental Hospital of Yonsei University were selected. Their ages ranged from 13 to 67 years (mean 36 years). All the patients were in good health and had no contra-indicative systemic diseases prior to surgery. The patients consented to this procedure after being informed about the potential benefits and risks of the procedure as well as other treatment options such as conventional prosthodontics or implants.
a. Pre-examination of the donor tooth and the recipient site Initially, CT radiographs of the donor tooth and the recipient bone were carefully examined. In this process, the width and height of the donor tooth were evaluated to determine the adaptability of the donor tooth to the recipient area (Figure 2). Possible impingement of the anatomical structures, such as the mandibular canal or the maxillary sinus cavity was also checked at this time.
Three-D data (DICOM format; Digital Imaging and Communication in Medicine) of the donor tooth was obtained using the CT Highspeed Advantage and a Denta Scan program produced by GE Medical Systems (Milwaukee, WI, USA). The CT protocol involved a slit thickness of 1 mm. The 3-D digital data obtained was fed into a visualization program (V-works, Cybermed Co., Seoul, Korea) and exported to the rapid prototyping machine to fabricate the actual sized tooth model. The material for the tooth model was starch/resin (Figure 3).
An artificial jaw model was also fabricated using the RP process. On this artificial jaw model, the surgical contouring of the recipient bone was simulated. The adaptability of the donor tooth to the recipient site was then examined. The bucco-lingual dimensions of the recipient site were carefully checked and compared with the size of the donor tooth. This procedure also provided an opportunity for the operator to practice real bone contouring of the recipient site prior to the actual surgery.
After administering local anesthesia, the flap of the recipient site was reflected, and the recipient bone was carefully contoured using a round implant bur (Center Punch Bur #3 mm, Degussa Co., Frankfurt, Germany) with abundant saline irrigation until the model tooth fitted snuggly into the recipient site with proper occlusion. A root canal treatment was performed before extracting the donor tooth.
The donor tooth was extracted with minimal injury and transferred to the prepared bone socket. Root end management (apicoectomy and retrograde-filling) was performed where necessary in order to prevent possible complications. Every effort was made to keep the root surface moist using physiological saline throughout the extra-oral procedures. For cases where the donor tooth did not have good retention in the bone, a wire-resin splint was used for two to eight weeks. Routine post-operative instructions were given to the patients.
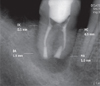
The distance between the transplanted root surface and the alveolar bone was measured on the post-operative x-ray in order to determine the adaptability of the transplanted tooth to the recipient bone using this protocol (Figure 4). The measurements from four points were obtained: mesiocervical (MC), mesio-apical (MA), disto-cervical (DC) and disto-apical (DA). Cases with large pre-existing periodontal bone destruction were eliminated.
The extra-oral time was defined as the period from extracting the donor tooth to its insertion into the recipient site, which was measured using a stopwatch. The average extra-oral time for those receiving intra-oral root canal treatment prior to extraction was separated from those which received the root canal treatment extra orally.
An in vitro experiment was performed to evaluate the accuracy of CARP model compared with 3D CT image and the real donor tooth in two maxilla and two mandible cadaver block bones.7
Two maxilla and two mandible block bones with 53 teeth were taken from two cadavers. Computed tomography was taken either in dry state and in wet state. After then, all teeth were extracted and the dimensions of the real teeth were measured using a digital caliper. The dimensions measured were the tooth length, mesio-distal and buccolingual width in crown and cervical portion. 3D CT image was generated using the V-works 4.0 (Cybermed Inc.) software and same measurements were made from the reconstructed 3D CT images. Twelve out of 53 teeth were randomly selected and the CARP model was fabricated. The same dimensions of each CARP model were measured and the discrepancies between the real tooth/3D CT image and the 3D CT image/CARP model were determined.
From our 251 clinical cases, the average distance between the transplanted root surface and the alveolar bone was 1.17 mm at the mesial cervix, 1.35 mm at the mesial apex, 0.98 mm at the distal cervix, and 1.26 mm at the distal apex.
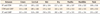
Absolute difference was 0.199 mm between real teeth and 3D CT image model, 0.169 mm between 3D CT image model and CARP model and 0.291 mm between real teeth and CARP model, respectively. Average size of 3D CT image was smaller than real teeth by 0.149 mm and that of CARP model was smaller than 3D CT image model by 0.067 mm (Table 1).
The success rates of conventional auto-transplantation technique of the teeth with fully developed roots, which were assessed according to loss of transplant, root resorption and ankylosis, varied from 60% to 88%.9-13 These comparatively unpromising results were presumably due to the sustained extra-oral time of the donor tooth and the physical trauma to the periodontal ligament during the extraction and repeated insertion of the donor tooth into the recipient bone cavity because bone contouring usually requires a number of trial fittings in order to obtain the proper seating.
The rapid prototyping tooth model was quite useful in solving these problems. Extraoral time ranged from immediately after extraction to 25 minutes, with a mean of 7 minutes 45 seconds. In the 168 patients who underwent an intraoral endodontic treatment for the donor tooth, the mean extraoral time was 7 minutes 10 seconds. The mean extraoral time in the 9 patients who were treated with extraoral endodontic treatment was 15 minutes 20 seconds, which was significantly different from the intraoral endodontic cases. The extra-oral time in regards with root canal treatment methods, 80.8% were performed within 10 minutes, 11.3% from 10 minutes to 15 minutes, and 7.9% were more than 15 minutes. Although no definite time limit has been suggested for the preservation of viable periodontal ligament cells, it is obvious that a shorter extra-oral time offers better integrity of the healthy periodontal cells of the donor tooth. It is generally accepted that the extra-oral time is the most important criterion for the successful periodontal healing in tooth re-implantation and transplantation.3,14-16
Hammarström et al., who used two different extra-oral periods for replanted teeth, reported that the ankylotic area did not increase after the initial ankylosis in a 15 minutes extra-oral period group while a 60 minutes group showed progressive ankylosis.17 Andreasen et al. observed normal periodontal ligament healing in more than 80% of cases after an extra-oral time of 18 minutes.18,19 This means that the donor tooth must be transplanted as quickly as possible. In this regard, the average extra-oral time of 7.58 minutes achieved from this study appears to be a reasonably safe margin.
The major complication after tooth transplantation or replantation is root resorption. This occurs as a result of the extraordinary activities of the dentinoclasts in the procedure of periodontal healing. Root resorption is traditionally classified into three categories, surface resorption, inflammatory resorption, and replacement resorption (ankylosis). Among those, replacement resorption is the most irreversible phenomenon because replacement resorption is part of the physiological process of normal bone remodeling. Once it begins, there are no effective methods to stop it. Briefly, while the initial physiological remodeling process of the osteoclasts resorbs the root dentin, a replacement is substituted only by bone and not by dentin. As this process continues, the whole root dentin is replaced by bone, which leads to exfoliation of the tooth (Figure 1). In our clinical trials, the root resorption was observed in only 4 out of 251 cases (1.6%). It is believed that these favorable results were the result of the relatively short extra-oral time of the donor tooth.
Good provision of blood supply is important for wound healing.20 Optimal contact between the donor tooth and the recipient bone would ensure good blood supply, as well as good immobilization. However, to our knowledge, there has been no report on the optimal distance of the transplanted root surface and the alveolar bone in tooth transplantation. In an effort to provide better blood supply and easy seating of the donor tooth, Nethander advocated a two-stage procedure for tooth transplantation.21 He first created a recipient bone cavity 2 mm larger than the estimated donor tooth size. After a two-week period when the bone cavity reached the primary healing stage with new connective tissue, he performed the second procedure, in which the donor tooth was snuggly seated in the connective tissue-healed bone cavity. Promising results were obtained after a follow-up of up to a five-year, and it was possible to transplant autogenous teeth with little risk of root resorption or other complications using this two-stage surgical technique. Although this protocol provided a good capillary bed for the donor tooth, there were still several problems. One is this technique requires two procedures. The second is there are few circumstances where such a large bone cavity can be prepared. The large gap between the bone cavity and the root surface can also be a problem.
In this protocol, the post-operative distance between the transplanted root surface and the alveolar bone ranged from 0.97 mm to 1.28 mm. The apical area was generally associated with a larger distance than the cervical area, which is probably because the apical portions of the donor teeth have more anatomical variations than the cervical portions. Considering that the cervical area is associated with the periodontium, the distance at this area is of greater clinical significance than in the apical area. Future studies should be aimed at determining the optimal distance between the transplanted root surface and the alveolar bone. It was interesting to find that there was a tendency toward better adaptability in the mesial surface than in the distal surface. This was probably because the curved distal roots required more room. Moreover, although the computer-aided tooth model offers a donor tooth of a similar size, the operator still has to manually contour the recipient bone.
The three-dimensional tooth image obtained by computerized tomography in this study was achieved by subtracting the different densities from the total data. For example, because bone and the teeth have different densities, only densities similar to that of the teeth are retained if all the densities lower than those of the teeth are subtracted. It was found that the computer-generated results were reasonably accurate when the model teeth were compared with the extracted donor teeth. However, in several cases, there were some difficulties encountered whilst placing a donor tooth into the pre-contoured bone cavity. It was unclear if this was due to errors in tooth fabrication or to surgical variances even though it is appreciated that these types of errors are difficult to eradicate, particularly with inexperienced operators. Therefore, we recommend the use of a 110% magnification of the CARP model tooth for initial attempts instead of a 100%.
The average discrepancy was 0.199 mm between the real teeth/3D CT image model, 0.169 mm between the 3D CT image model/CARP model and 0.291 mm between the real teeth/CARP model (Tables 1 - 3). It was found that 3D CT image and CARP models were generally smaller than the real teeth by 0.149 mm and 0.216 mm, respectively.
From these results, the computer-aided rapid prototyping process might be of value in reducing the extra-socket time and providing good apposition between the donor tooth and recipient bone, which can reduce the possibility of injury to the transplanted tooth during the tooth transplantation process.
Figures and Tables
Figure 1
(a) A 12-year old male patient visited for reposition of the avulsed tooth (center). The extra-oral time before reposition was about two hours; (b) Root of the repositioned tooth became severely resorbed after 4 years; (c) Extracted tooth showed almost no root structure left.
Figure 2
(a) Bucco-lingual cross-sections show the bucco-lingual dimension; (b) Distance between the alveolar crest and the mandibular canal; (c) 3-D images with the real dimensions of donor tooth.

Notes
References
1. Lee SJ, Jung IY, Lee CY, Choi SY, Kum KY. Clinical application of computer-aided rapid prototyping for tooth transplantation. Dent Traumatol. 2001. 17:114–119.

2. Andreasen JO. Interrelation between alveolar bon and periodontal ligament repair after replantation of mature permanent incisors in monkeys. J Periodontal Res. 1981. 16:228–235.

3. Hupp JG, Mesaros SV, Aukhil I, Trope M. Periodontal ligament vitality and histologic healing of teeth stored for extended periods before transplantation. Endod Dent Traumatol. 1998. 14:79–83.

4. Andreasen JO. Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int J Oral Surg. 1981. 10:54–61.

5. Choi JY, Choi JH, Kim NK, Kim Y, Lee JK, Kim MK, Lee JH, Kim MJ. Analysis of errors in medical rapid prototyping models. Int J Oral Maxillofac Surg. 2002. 31:23–32.

6. Lill W, Solar P, Ulm C, Watzek G, Blahout R, Matejka M. Reproducibility of three-dimensional CT-assisted model production in the maxillofacial area. Br J Oral Maxillofac Surg. 1992. 30:233–236.

7. Lee SJ, Kim E, Kim KD, Lee SJ. In vitro study for Accuracy of computer aided rapid prototyping model(CARP model) compared with real donor tooth in autogenous tooth transplantation. J Korean Dent Assoc. 2006. 44:115–122.
8. Kim E, Jung JY, Cha IH, Kum KY, Lee SJ. Evaluation of the prognosis and causes of failure in 182 cases of autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 100:112–119.

9. Sobhi MB, Rana MJ, Manzoor MA, Ibrahim M, Tasleemul-Hudda . Autotransplantation of endodontically treated third molars. J Coll Physicians Surg Pak. 2003. 13:372–374.
10. Mejàre B, Wannfors K, Jansson L. A prospective study on transplantation of third molars with complete root formation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 97:231–238.

11. Cohen AS, Shen TC, Pogrel MA. Transplanting teeth successfully: autografts and allografts that work. J Am Dent Assoc. 1995. 126:481–485.

12. Schwartz O, Bergmann P, Klausen B. Autotransplantation of human teeth. A life-table analysis of prognostic factors. Int J Oral Surg. 1985. 14:245–258.
13. Nethander G, Andersson JE, Hirsch JM. Autogenous free tooth transplantation in man by a 2-stage operation technique. A longitudinal intra-individual radiographic assessment. Int J Oral Maxillofac Surg. 1988. 17:330–336.

14. Andreasen JO, Paulsen HU, Yu Z, Schwartz O. A long-term study of 370 autotransplanted premolars. Part III. Periodontal healing subsequent to transplantation. Eur J Orthod. 1990. 12:25–37.

15. Van Hassel HJ, Oswald RJ, Harrington GW. Replantation 2. The role of the periodontal ligament. J Endod. 1980. 6:506–508.

16. Andreasen JO. Gutmann JL, Harrison JW, editors. Root fractures, luxation and avulsion injuries-diagnosis and management. Proceedings of the International Conference on Oral Trauma. 1986. Chicago: American Association of Endodontics;79–92.
17. Hammarström L, Blomlöf L, Lindskog S. Dynamics of dentoalveolar ankylosis and associated root resorption. Endod Dent Traumatol. 1989. 5:163–175.

18. Andreasen JO, Kristerson L. The effect of extra-alveolar root filling with calcium hydroxide on periodontal healing after replantation of permanent incisors in monkeys. J Endod. 1981. 7:349–354.

19. Andreasen JO, Andreasen FM. Textbook and color atlas of traumatic injuries to the teeth. 1994. 3rd ed. St. Louis: Mosby Co;18.
20. Goerig AC, Nagy WW. Successful intentional reimplantation of mandibular molars. Quintessence Int. 1988. 19:585–588.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download