Abstract
Objectives
The purpose of this study was to enhance curing light penetration through resin inlays by modifying the thicknesses of the dentin, enamel, and translucent layers.
Materials and Methods
To investigate the layer dominantly affecting the power density of light curing units, resin wafers of each layer with 0.5 mm thickness were prepared and power density through resin wafers was measured with a dental radiometer (Cure Rite, Kerr). The dentin layer, which had the dominant effect on power density reduction, was decreased in thickness from 0.5 to 0.1 mm while thickness of the enamel layer was kept unchanged at 0.5 mm and thickness of the translucent layer was increased from 0.5 to 0.9 mm and vice versa, in order to maintain the total thickness of 1.5 mm of the resin inlay. Power density of various light curing units through resin inlays was measured.
Results
Power density measured through 0.5 mm resin wafers decreased more significantly with the dentin layer than with the enamel and translucent layers (p < 0.05). Power density through 1.5 mm resin inlays increased when the dentin layer thickness was reduced and the enamel or translucent layer thickness was increased. The highest power density was recorded with dentin layer thickness of 0.1 mm and increased translucent layer thickness in all light curing units.
Patient demand for tooth-colored posterior restorations is increasing. Resin inlays are alternatives to direct composite restorations in posterior teeth, because the resin inlays are polymerized in the laboratory before cementation.1 Therefore, the risk of postoperative sensitivity and microleakage due to polymerization shrinkage can be reduced.2-4 Also, a superior contact with the adjacent teeth can be achieved under a more controlled environment. Usually, the indirect composite resin systems are composed of dentin or opaque layer, enamel layer, and translucent layer. And as tooth preparation for resin inlays is minimum 1.5 mm in the occusal surface, the manufacturers recommend building up each layer in 0.5 mm.5 However, little information is provided about the curing light penetration of each layer and the combination of the layers forming the resin inlay.
Resin cements are the material of choice for the adhesive cementation of resin inlays. Resin inlays require a perfect seal and a strong, durable resin bond provides high retention and improves marginal adaptation.6 Therefore, microleakage is prevented and fracture resistance of the restored tooth and the restoration itself is increased.7,8 Resin cements are available in chemical cure, light cure, and dual cure formulations. Dual cure cements are usually used for resin inlays. They polymerize chemically when the base and catalyst components are mixed and also when they are subjected to the curing light from a light curing unit (LCU). Dual cure resin cements offer the advantages of extended working time and controlled polymerization and chemical activators ensure a high degree of polymerization.9
During cementation of resin inlays, the peripheral parts of the cement interface, mainly at the occlusal aspects, are the only parts that can benefit from both chemical and light curing, because they are readily accessible to the curing light. Polymerization of the more remote parts of the cement, for example, at the pulpal floor, rely more extensively on the chemical component of the curing mechanism.10 However, most dual cure resin cements still require light curing and demonstrate inferior hardness when light activation is omitted.10,11 Hasegawa et al. studied the hardening of three dual cure cements under resin inlays and reported that chemical curing alone did not completely harden the cements when light was attenuated by the tooth structure and the restoration material.11 Chan and Boyer studied the hardening of light cure resin cements through porcelain and found that the thickness and shade of the porcelain can affect the hardness of the cement.12
Light intensity decreases as a function of depth, whereas composite resin characteristics such as optical translucency and the refractive index of the resin dictate the amount of light scattering, and consequently, limit the depth of cure. Thorough light curing, therefore, depends on light penetration to a desired depth through resin inlays that may prevent such penetration.13 For polymerization of composite resins, curing light with a minimum intensity of 300 mW/cm2 is required.14,15 Therefore, to polymerize dual-cure resin cements, curing light must have an intensity of at least 300 mW/cm2 after transmitting through the resin inlay. Most studies on power density measurement through various indirect restorations such as ceramics, zirconia, and composite resins were limited to single shade materials, and only a few studies dealt with the shade combinations of a resin inlay simulating the clinical situation including the dentin, enamel, and translucent shades.13,16-20
Therefore, the purpose of this study was to determine the resin inlay layer combination having an increased curing light penetration for light curing of the dual cure resin cements beneath the resin inlay. At first, the power density of LCUs through resin wafers of dentin, enamel, and translucent layer of 0.5 mm thickness was measured to investigate which layer dominantly affected the curing light penetration. Then the corresponding layer was modified for increasing curing light penetration through resin inlays. Also, the effect of LCUs with various power densities on curing light penetration was investigated.
A custom-made cylindrical aluminum mold 60 mm in diameter and 45 mm in length with a hole 15 mm in diameter and 30 mm in depth at the center was used to fabricate the resin wafers and resin inlays (Figure 1). A hole of 1.5 mm diameter was fabricated in order to ensure that the resin specimens could completely cover the power density measurement spot of dental radiometer, and also be larger than the fiberoptic tip diameter of the LCUs. A flat Teflon plate 15 mm in diameter was inserted into the hole and a bolt was attached to the opposite side of the plate, so that the space in the hole could be adjusted by the rotation of the bolt. By rotating the bolt 360 degrees counterclockwise, the Teflon plate could be moved in a downward direction thereby rendering a 1 mm deep empty space in the aluminum mold. The rotation of the bolt was marked in 10 steps such that one step corresponded to a downward movement of the Teflon plate by 0.1 mm.
Three layers of Sinfony indirect lab composite (3M ESPE, Seefeld, Germany) were used: A2 dentin (D2), E2 enamel (E2), and T1 translucent (T1) layers. To investigate the effect of shade on the power density, resin wafers of different shades measuring 0.5 mm in thickness were fabricated. The Teflon plate was lowered by 0.5 mm by rotating the bolt counterclockwise and the empty space in the aluminum mold was filled with one of the shades. Then, the upper surface of the aluminum mold was covered with a polyester film and a glass slab to put pressure on the surface and was light cured with a light emitting diode (LED) LCU (Elipar FreeLight 2, 3M ESPE, St Paul, MN, USA) for 5 seconds. After removing the glass slab and the polyester film, the dentin layer was light cured for 20 seconds using an overlapping curing procedure in order to ensure that every part of the specimen was light cured. Seven specimens of each resin wafer were fabricated.
The resin inlays were placed over the measurement spot of a hand-held dental radiometer (Cure Rite, Kerr, Milford, MA, USA) and the LCUs were activated with the touch of the fiberoptic tip to the resin inlays. The power density of the LCUs through resin inlays was measured at 10 seconds from the start of light curing, according to the manufacturer's instructions. Three kinds of LCUs were investigated: a low-power density halogen LCU (360, Optilux 360, Demetron, Danbury, CT, USA), a high-power density LED LCU (FL2, Elipar FreeLight 2), and a newly introduced high-power density LED LCU (S10, Elipar S10, 3M ESPE, Table 1). The power densities of LCUs were 530 mW/cm2, 1,040 mW/cm2, and 1,340 mW/cm2, respectively, measured with the dental radiometer.
To enhance the power density through resin inlays, the thickness of the dentin layer was reduced stepwise from 0.5 to 0.1 mm by 0.1 mm. To simplify the variations of other layer thicknesses, the thickness of the enamel layer was kept unchanged at 0.5 mm and the thickness of the translucent layer was increased and vice versa to maintain the thickness of 1.5 mm of the resin inlay. Therefore, the resin inlays were fabricated using layer thickness combinations of 0.5-0.5-0.5 mm (d5e5t5), 0.4-0.5-0.6 mm (d4e5t6), 0.4-0.6-0.5 mm (d4e6t5), 0.3-0.5-0.7 mm (d3e5t7), 0.3-0.7-0.5 mm (d3e7t5), 0.2-0.5-0.8 mm (d2e5t8), 0.2-0.8-0.5 mm (d2e8t5), 0.1-0.5-0.9 mm (d1e5t9), 0.1-0.9-0.5 mm (d1e9t5) in the order of dentin-enamel-translucent shades.
For example, to fabricate resin inlays of d5e5t5 combination, the Teflon plate was lowered by 0.5 mm and the empty space in the aluminum mold was filled with dentin layer. After light curing the dentin layer as described above, the Teflon plate with light cured dentin layer was lowered by another 0.5 mm and the empty space in the aluminum mold was filled with the enamel layer and light cured. The same procedure was repeated with the translucent layer in order to fabricate the resin inlay of 1.5 mm thickness. The other thickness combinations of resin inlays were fabricated as described above by controlling the thickness of each layer by the rotation of the bolt. Seven specimens of resin inlays with each thickness combination were fabricated.
The power densities of LCUs through resin inlays and resin wafers were analyzed with two-way ANOVA at 0.05 significance level followed by post-hoc comparisons with Tukey's HSD test (SPSS 12.0K, SPSS Inc., Chicago, IL, USA). After this, one-way ANOVA and Tukey's HSD test were employed to compare all groups.
Power densities through 0.5 mm resin wafers of each shade are shown in Figure 2. The two-way ANOVA showed a significant effect for both the main factors (shades, p < 0.001; LCUs, p < 0.001) and their interaction (p < 0.001). The power densities through the translucent, enamel, and dentin shades decreased significantly in that order.
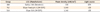
The power densities of LCUs through variations of layer thickness of the d2e2t1 shade are shown in Tables 2 and 3. The two-way ANOVA showed a significant effect for both the main factors (shades, p < 0.001; LCUs, p < 0.001) and their interaction (p < 0.001). In all LCUs, the power densities through the resin inlays were generally increased as the thickness of the dentin layer was decreased. The maximum power density of 360 LCU was 142 mW/cm2 and was measured through the d1e5t9 combination and 141 mW/cm2 through d2e5t8 combination which showed no statistical difference. The power densities of FL2 LCU through the d2e5t8, d1e9t5 and d1e5t9 combinations were more than 300 mW/cm2. The power densities of S10 LCU through every specimen of the dentin layer from 0.5 to 0.1 mm in thickness were more than 300 mW/cm2. When the dentin layer thickness was kept unchanged, an increase in the thickness of the translucent layer rather than the enamel layer resulted in enhanced curing light penetration. Especially, when the thickness of the dentin layer was decreased to 0.2 and 0.1 mm, the power density through resin inlays with increased translucent layer thickness was significantly higher than that through resin inlays with increased enamel layer thickness (p < 0.05).
The composite resin used in the present study was a microhybrid material marketed for inlays, onlays, veneers, and crowns (Sinfony indirect lab composite, 3M ESPE). It is composed of 50 to 55% aliphatic (mainly HEMA) and cycloaliphatic monomers by weight as well as 45 to 50% borosilicate glass and quartz (particle size distribution of 0.5 to 1.0 µm). In our previous study, power densities of LCUs were measured through 1.5 mm thick resin inlays fabricated with direct and indirect composite resins of Z350 A3, Supreme XT A3B + A3E, and Sinfony A3 + E3 + T1 (3M ESPE).20 The power density through resin inlays could be enhanced by using indirect composite resin with multiple shade layers. To further enhance the power density of LCUs through resin inlays, the same kind of indirect composite resin was used as in the previous study.
The power density through each shade of 0.5 mm thickness was measured to investigate the effect of shades on light penetration. The power density of all LCUs through the dentin shade was significantly lower than that through the enamel and translucent shades. It is assumed that the pigments used for the dentin shade affected the curing light penetration more than the other shades.21 Although the resin wafers were as thin as 0.5 mm, the power density through the dentin shade was decreased by 61, 58, and 55% of the original power densities in 360, FL2, and S10 LCUs. The power density through the enamel shade was decreased by 40, 35, and 31%, and that through the translucent shade was decreased by 32, 28, and 24%. This was in accordance with the other studies. Rasetto et al. measured curing light penetration through all-ceramic dental materials and reported that the power density of the conventional halogen LCU (660 mW/cm2) and high-intensity halogen LCU (1,050 mW/cm2) through 0.4 mm thick Procera coping was decreased to 230 mW/cm2 and 345 mW/cm2 respectively which corresponds to 35 and 33% of the original power density.13 Also, Prati et al. reported that composite resin caused a dramatic reduction in power density.17
As the dentin layer of the resin inlays had the greatest effect on the reduction of power density, we reduced the thickness of the dentin layer and increased the thickness of either the enamel layer or the translucent layer in order to increase the curing light penetration. The power density of 360 LCU through the resin inlays with dentin layer of 0.5 mm thickness was measured 103 mW/cm2. Through reduction of the dentin layer to 0.1 mm thickness, the power density was enhanced to 142 mW/cm2. However, to properly light cure the resin cement under the resin inlay, power density of minimum 300 mW/cm2 is required.22 Therefore, low-power density LCUs would be inappropriate for proper light activation of resin cements through resin inlays. The power density of FL2 LCU was measured significantly higher than that of 360 LCU through resin inlays of every thickness combination (p < 0.05). The power density through the resin inlays with dentin layer of 0.5 mm thickness was measured 239 mW/cm2, and the power density could be enhanced by reducing the dentin layer thickness. The power densities through the d2e5t8, d1e9t5, and d1e5t9 combinations were more than 300 mW/cm2 thereby indicating its light activation capability. The power density of S10 LCU through every thickness combination was more than 300 mW/cm2. Therefore, it can be assumed that when the LCUs with irradiance more than 1,340 mW/cm2 are used, the power density through the resin inlays with dentin shades of 0.5 mm thickness will be sufficient for light activation of resin cement.
For light curing the resin cement beneath the resin inlay, the original power density of the LCUs as well as the curing light penetration through resin inlays should be considered. Since previous studies on the curing efficiency of halogen and LED LCUs showed that the power density of LCUs rather than the source of the light had the major effect on the degree of conversion of composite resin, a low-power density halogen LCU of 530 mW/cm2 and two high-power density LED LCUs of 1,040 mW/cm2 and 1,340 mW/cm2 respectively were used in this study.23,24 The results showed that the power density of the low-power density LCU was insufficient to light cure the resin cement beneath the resin inlay even if the curing light penetration was enhanced with reduced dentin layer thickness. The power density of LED LCU of 1,040 mW/cm2 through the resin inlays was sufficient for light curing the resin cement if the dentin layer thickness was reduced to 0.2 mm or less. When using more powerful LED LCU of 1,340 mW/cm2, the power density through the resin inlays was sufficient even with dentin layer thickness of 0.5 mm to light cure the resin cement under the resin inlays. Therefore, in the aspect of light curing the resin cement beneath the resin inlays, high-power density LCUs would be recommendable.
Interactions between the shade of the layer and LCUs were observed in the statistical analyses of power densities through resin wafers and inlays. These interactions could be explained by the curing light diffusion of LCUs. In our previous study, curing light diffusion of LED LCUs was measured as 75.0 ± 0.8 degrees, whereas that of halogen LCUs was measured as 48.3 ± 3.1 degrees.15 It could be possible that the difference in curing light diffusion affected the curing light transmission through resin inlays and caused the interaction between the layer shades and the LCUs.
In this study, we only considered the light penetration through the resin inlays and the esthetics of the resin inlays due to decreased dentin shade thickness and increased translucent shade thickness was not taken into account since esthetics is not an important factor in posterior restorations. We only tried not to omit either of the dentin, enamel, and translucent shades while maintaining the resin inlay thickness of 1.5 mm. Also, the axial wall of the peripheral box is in similar or even inferior situation as the pulpal floor of the prepared tooth for curing light penetration. To enhance the curing light penetration into the axial wall, light curing procedure at the facial and lingual aspect as well as the occusal aspect seems to be inevitable.
Within the limitations of this study, the dentin layer affected the curing light penetration through resin wafers more than the enamel and translucent layers. Therefore, dentin layer thickness was reduced to enhance the power density of LCUs penetrating the resin inlays. However, when low-power density LCU of 530 mW/cm2 is used, reducing the dentin layer thickness could not enhance the power density over 300 mW/cm2 through the resin inlay. With high-power density LCU of 1,040 mW/cm2, reducing the dentin layer thickness to 0.2 mm would be recommendable. With another high-power density LCU of 1,340 mW/cm2, there was no need of reducing the dentin layer thickness as the power density was measured more than 300 mW/cm2 through every resin inlay. Therefore, when light curing the resin cements under the resin inlays, the resin inlays should be fabricated with dentin layer thickness of 0.2 mm or less, and high-power density LCUs of 1,040 mW/cm2 or more should be used for light curing the resin cements.
Figures and Tables
 | Figure 2Power densities of light curing units measured through 0.5 mm resin wafers. The power densities through the dentin, enamel, and translucent shades showed statistically significant differences (n = 7, p < 0.001). D2, dentin shade A2; E2, enamel shade E2; T1, translucent shade T1; 360, Optilux 360; FL2, Elipar FreeLight 2; S10, Elipar S10. |
Table 2
Summary of two-way ANOVA of main factors (light curing units and layer thicknesses) and their interaction for power density
Table 3
Power densities (mW/cm2 ± SD, n = 7) of light curing units through 1.5 mm d2e2t1 shade with different dentin layer thicknesses

Values having the same superscript letters are not significantly different at α = 0.05. Uppercase letters were used to compare groups in the rows; lowercase letters were used to compare groups in the columns.
d5, d4, d3, d2, d1, dentin layer thicknesses of 0.5 mm, 0.4 mm, 0.3 mm, 0.2 mm, 0.1 mm; e9, e8, e7, e6, e5, enamel layer thicknesses of 0.9 mm, 0.8 mm, 0.7 mm, 0.6 mm, 0.5 mm; t9, t8, t7, t6, t5, translucent layer thicknesses of 0.9 mm, 0.8 mm, 0.7 mm, 0.6 mm, 0.5 mm; 360, Optilux 360; FL2, Elipar FreeLight 2; S10. Elipar S10.
Notes
References
1. Sheth PJ, Jensen ME, Sheth JJ. Comparative evaluation of three resin inlay techniques: microleakage studies. Quintessence Int. 1989. 20:831–836.
2. Bausch JR, de Lange K, Davidson CL, Peters A, de Gee AJ. Clinical significance of polymerization shrinkage of composite resins. J Prosthet Dent. 1982. 48:59–67.

3. Eick JD, Welch FH. Polymerization shrinkage of posterior composite resins and its possible influence on postoperative sensitivity. Quintessence Int. 1986. 17:103–111.
4. Robinson PB, Moore BK, Swartz ML. Comparison of microleakage in direct and indirect composite resin restorations in vitro. Oper Dent. 1987. 12:113–116.
5. Roberson TM, Heymann HO, Swift EJ. Sturdevant's art & science of operative dentistry. 2002. 4th ed. St. Louis: Mosby Inc.;580.
6. el-Mowafy O. The use of resin cements in restorative dentistry to overcome retention problems. J Can Dent Assoc. 2001. 67:97–102.
7. Sorensen JA, Kang SK, Avera SP. Porcelain-composite interface microleakage with various porcelain surface treatments. Dent Mater. 1991. 7:118–123.

8. Jensen ME, Sheth JJ, Tolliver D. Etched-porcelain resin-bonded full-veneer crowns: in vitro fracture resistance. Compendium. 1989. 10:336–338. 340–341. 344–347.
9. Krämer N, Lohbauer U, Frankenberger R. Adhesive luting of indirect restorations. Am J Dent. 2000. 13(Spec No):60D–76D.
10. el-Badrawy WA, el-Mowafy OM. Chemical versus dual curing of resin inlay cements. J Prosthet Dent. 1995. 73:515–524.

11. Hasegawa EA, Boyer DB, Chan DC. Hardening of dual-cured cements under composite resin inlays. J Prosthet Dent. 1991. 66:187–192.

12. Chan KC, Boyer DB. Curing light-activated composite cement through porcelain. J Dent Res. 1989. 68:476–480.

13. Rasetto FH, Driscoll CF, von Fraunhofer JA. Effect of light source and time on the polymerization of resin cement through ceramic veneers. J Prosthodont. 2001. 10:133–139.

14. Rueggeberg FA, Jordan DM. Effect of light-tip distance on polymerization of resin composite. Int J Prosthodont. 1993. 6:364–370.
15. Chang HS, Lee SR, Hong SO, Ryu HW, Song CK, Min KS. Effect of infection control barrier thickness on light curing units. J Korean Acad Conserv Dent. 2010. 35:368–373.

16. Blackman R, Barghi N, Duke E. Influence of ceramic thickness on the polymerization of light-cured resin cement. J Prosthet Dent. 1990. 63:295–300.

17. Prati C, Chersoni S, Montebugnoli L, Montanari G. Effect of air, dentin and resin-based composite thickness on light intensity reduction. Am J Dent. 1999. 12:231–234.
18. dos Santos GB, Alto RV, Filho HR, da Silva EM, Fellows CE. Light transmission on dental resin composites. Dent Mater. 2008. 24:571–576.

19. Kim SS, Cho SS, Um CM. The microhardness and the degree of conversion of light cured composite resin and dual cured resin cements under porcelain inlay. J Korean Acad Conserv Dent. 2000. 25:17–40.
20. Chang HS, Lim YJ, Kim JM, Hong SO. Power density of light curing units through resin inlays fabricated with direct and indirect composites. J Korean Acad Conserv Dent. 2010. 35:353–358.

21. Taira M, Okazaki M, Takahashi J. Studies on optical properties of two commercial visible-light-cured composite resins by diffuse reflectance measurements. J Oral Rehabil. 1999. 26:329–337.

22. Chang HS. Infection control of light curing units. J Korean Acad Conserv Dent. 2010. 35:235–237.

23. Rueggeberg FA, Caughman WF, Curtis JW Jr. Effect of light intensity and exposure duration on cure of resin composite. Oper Dent. 1994. 19:26–32.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download