Abstract
Background
This study was performed to evaluate the associations between sleep duration and smoked cigarettes per day, prevalence of heavy smoking.
Methods
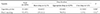
This study was based on the data of 9,893 subjects who are currently smoking, from the 4th to 6th Korea National Health and Nutrition Examination Survey. Based on appropriate sleep duration from National Sleep Foundation, study subjects were categorized into short, appropriate and over sleep group. Multiple regression analysis was performed to evaluate the association between sleep duration and smoked cigarettes per day, prevalence of heavy smoking. Age, gender, household income, education, marital status, occupation, alcohol use, body weight, hypertension, diabetes mellitus, depression, and level of stress were controlled.
Figures and Tables
References
1. OECD. Daily smokers 2017 [Internet]. Paris: OECD;2017. Accessed Jan 2, 2018. Available from: https://data.oecd.org/healthrisk/daily-smokers.htm#indicator-chart.
3. Lim MT, Sung HN, Seo HJ, Kim SG, Chang DM, Pack HJ, et al. Smoking and health-related quality of life among Korean adults. Korean J Fam Pract. 2015; 5(2):135–142.
4. Wetter DW, Young TB. The relation between cigarette smoking and sleep disturbance. Prev Med. 1994; 23(3):328–334.

5. Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Arch Intern Med. 1995; 155(7):734–737.

6. McNamara JP, Wang J, Holiday DB, Warren JY, Paradoa M, Balkhi AM, et al. Sleep disturbances associated with cigarette smoking. Psychol Health Med. 2014; 19(4):410–419.

7. Cohrs S, Rodenbeck A, Riemann D, Szagun B, Jaehne A, Brinkmeyer J, et al. Impaired sleep quality and sleep duration in smokers-results from the German Multicenter Study on Nicotine Dependence. Addict Biol. 2014; 19(3):486–496.

8. Sabanayagam C, Shankar A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011; 12(1):7–11.

9. Palmer CD, Harrison GA, Hiorns RW. Association between smoking and drinking and sleep duration. Ann Hum Biol. 1980; 7(2):103–107.

10. Riedel BW, Durrence HH, Lichstein KL, Taylor DJ, Bush AJ. The relation between smoking and sleep: the influence of smoking level, health, and psychological variables. Behav Sleep Med. 2004; 2(1):63–78.

11. Suratt P, Enfield K, Brown CD. Cigarette smoking is associated with short sleep duration in healthy adults. Am J Respir Crit Care Med. 2014; 189:A4091.
12. Mehari A, Weir NA, Gillum RF. Gender and the association of smoking with sleep quantity and quality in American adults. Women Health. 2014; 54(1):1–14.

13. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015; 1(1):40–43.

14. Wilson D, Wakefield M, Owen N, Roberts L. Characteristics of heavy smokers. Prev Med. 1992; 21(3):311–319.

15. Centers for Disease Control and Prevention (CDC). Decrease in smoking prevalence-Minnesota, 1999–2010. MMWR Morb Mortal Wkly Rep. 2011; 60(5):138–141.
16. Rosenberg L, Palmer JR, Rao RS, Shapiro S. Low-dose oral contraceptive use and the risk of myocardial infarction. Arch Intern Med. 2001; 161(8):1065–1070.

17. Pack HJ, Kim JS, Kim KM, Kim SM, Lee DH, Kim SS, et al. Nicotine dependence and internal response to stress in male smokers. J Korean Acad Fam Med. 2007; 28(8):604–609.
18. Bae JM, Ahn YO, Park BJ. Association of stress level with smoking amounts among university students. Korean J Prev Med. 1994; 27(1):1–10.
19. Lee KH, Chung WJ, Lee SM. Association of stress level with smoking. J Korean Acad Fam Med. 2006; 27(1):42–48.
20. Kim HS, Bae SS. Factors associated with relapse to smoking behavior using health belief model. J Agric Med Community Health. 2011; 36(2):87–100.

21. Carey MP, Kalra DL, Carey KB, Halperin S, Richards CS. Stress and unaided smoking cessation: a prospective investigation. J Consult Clin Psychol. 1993; 61(5):831–838.

22. Hamidovic A, de Wit H. Sleep deprivation increases cigarette smoking. Pharmacol Biochem Behav. 2009; 93(3):263–269.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download