Abstract
Background
It is important to understand physicians' awareness and knowledge on hypertension guideline to comprehend physician oriented barrier against proper hypertension management. Current guidelines emphasize on the role of home blood pressure monitoring. The aim of this study is to investigate the level of awareness and knowledge of Korean physicians on home blood pressure monitoring recommended in current guideline.
Methods
A questionnaire survey asking home blood pressure measurement, as well as prehypertension and life style modification, was conducted among 36 primary physicians and 25 residents of a tertiary medical center.
Results
Except the limitation alcohol intake (80.3%), the physicians demonstrated above 90% of agreement with other contents of life style modification recommended by published guidelines (salt restriction, stop smoking, weight loss, and regular aerobic exercise). Majority (77.7%) of primary physicians recommend home blood pressure measurement to their patients. Significantly primary physicians were likely to recommend home blood pressure monitoring than residents (48% vs. 77.7%, p = 0.027). But both physicians and residents show poor compliance to home blood pressure monitoring guideline in the point of blood pressure measuring (12% vs. 19.4%, p > 0.05). But most of participants are aware of adverse effect of prehypertension (88.5%) and the need of its treatment (96.7%).
Proper management of hypertension can reduce the risk of cardiovascular disease and extend life.1) Unfortunately, management of hypertension remains suboptimal leading to higher morbidity and mortality.2) The situation is similar in Korea. The Korea National Health and Nutrition Examination Survey showed that only 42.4% of patients with hypertension archived target blood pressure (BP) in 2008. Recently, studies on barrier against optimal BP control showed that barrier is oriented from not only patient but also physicians. Suggested physician related barriers include non-adherence to published guidelines and failure to emphasized life style modification.2-4) Therefore, it is important to understand physician's attitude and knowledge on the contents from hypertension guideline, which already has been reported insufficient in the previous studies.5,6) Recently, current hypertension guidelines recognized clinical importance of home BP measurement based on the studies indicate prognostic significant of home BP is better than causal office BP measurement.7) In 2007, the Society of Korean Hypertension published BP monitoring guideline regarding home BP measurement. The aim of this study is to investigate the level of awareness and knowledge of Korean physicians on home BP monitoring recommended in current guideline.
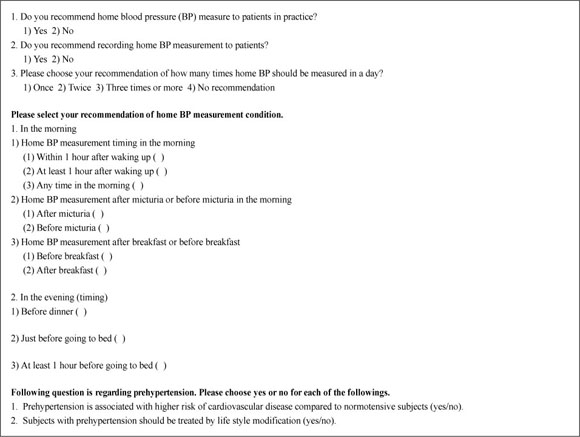
We designed a survey to determine primary physician's knowledge and acceptance of the guidelines. This survey asked about the awareness and the recommendation in real practice on home BP measurement based on the current hypertension guideline. The questionnaires also asked the issues about pre-hypertension and life style modification (Appendix 1).
We conducted a questionnaire survey among 36 primary physicians who attended an internal medicine seminar held in tertiary medical center. The same survey was carried out among 25 residents under training of internal medicine of a tertiary hospital.
The study instrument was a self-administrable questionnaire consisting of multiple choice questions. The questions of this survey assessed the physicians' practice and knowledge on home BP measurement, prehypertension, and life style modification. Questions focused on home BP measurement procedure were made on the basis of home BP measurement guideline8) recommended procedure of home BP monitoring is as follows: measure 2 times a day (in the morning and evening); in the sitting position; measurement 2 to 5 minutes after taking rest; in the morning within 1 hour after waking up, after micturia; in the evening, just before going to bed; and don't take caffeine or smoke within 30 minutes sitting.
All analyses and calculation was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). For categorical variables, counts and percentages are presented. Chi-square test or Fisher's exact test were used to compare categorical variables. To compare tendency of recommendation between questions about non-pharmacologic treatment, Fisher's exact test was used and a p-value < 0.05 was considered to be statically significant.
Total of 61 doctors were enrolled in this survey (Table 1). Among them, 36 doctors (59%) were primary physicians who have treated hypertensive patients more than five years. Fifty-five percent of the primary physicians (n = 20) practiced in the local clinic and 16 physicians practiced in community hospital. Twenty five (40.9%) doctors worked as residents in a tertiary medical center.
Most of primary physicians answer they advised to their patients lifestyle modifications recommended by published guidelines, such as salt restriction, aerobic exercise, stop smoking, weight reduction, and limitation of alcohol intake. But compared to salt restriction, aerobic exercise, and stop smoking, physicians are less likely to recommend the limitation of alcohol intake (80.3%) to their patients (limitation of alcohol vs. stop smoking, p = 0.001; limitation of alcohol vs. exercise, p = 0.005; limitation of alcohol vs. restriction of salt, p = 0.001). But there was no difference between primary physicians in local clinic and in community hospital, also between primary physicians and residents (Table 2).
More than half (65.5%) of the participants recommended home BP to their patients with hypertension (Table 3). More primary physicians were likely to recommend home BP measurement compared to resident group (48% vs. 77.7%, p = 0.027). More primary physicians encouraged their patient to record home BP measurements (12% vs. 69.4%, p < 0.001). More primary physicians practicing in clinics recommended home BP measurement and encourage recording the home BP reading to their patients compared to primary physicians in community hospital. But the tendency was not statically significant.
In response to the question about the frequency of home BP measure in a day, 58.3% of primary physicians answer 'once a day' and only 36.1% 'twice a day.'
Only 16.4% of the physicians answered correctly to all the items asking the procedure of home BP measurement (Table 4). But there was no difference between primary physicians in local clinic and in community hospital (27% vs. 12.5%, p = 0.412), also between physicians and residents (12% vs. 19.4%, p > 0.05). No significant difference was shown between groups according to the period of practice years (5-9 years vs. 10-19 years vs. ≥20 years; 12.5% vs. 11.1% vs. 36%; p = 0.234).
Majority of physicians answered correctly to the questions about adverse outcome of prehypertension (88.5%) and the need of treatment of prehypertension (96.7%). There were no significant differences between primary physicians in local clinic and in community hospital, also between primary physicians and residents.
Our survey showed that physicians have acceptable knowledge and attitude on the contents of published guidelines on prehypertension, life style modification, and recommendation of home BP measurement, but low consistency with the details of BP measuring.
Most of the physicians advised to their patient the principles of life modification such as sodium restriction, weight loss, regular aerobic exercise, and stop smoking with acceptable level. But physicians recommended significantly less the limitation of alcohol consumption compared to the other contents (sodium restriction, regular aerobic exercise, and stop smoking). This relative reluctance is thought to be originated from the generous Korean culture to alcohol intake. Actually, excessive alcohol intake is becoming a major health problem in Korea. According to the World Health Organization report, Korea ranks 2nd in alcohol consumption per capita and the prevalence of at risk alcohol intake has increased from 14.9% in 2005 to 19.7% in 2008.9-11) Unlike moderate alcohol intake lowering the risk of cardiovascular events among healthy adults, excessive or binge drinking is associated with higher cardiovascular disease risk.12) Fortunately, the movement to change this generous Korean culture is rising in recent. According, physicians have to take more effort to be sensitive to the risk of alcohol and to teach the correct habit of alcohol intake in hypertensive patients.
Another reason of reluctance may be physician's doubt about the efficacy of brief alcohol counseling in clinics on patient's behavior. But there are two randomized controlled trials, which showed that regular 10 to 15 minutes brief physician advice decreased alcohol use in the problem alcohol drinkers.13,14) Thus screening alcohol use disorder and brief counseling by physicians as a part of hypertension management should be encouraged.
Recent several hypertension guidelines recognized clinical implication of home BP measurements as a optional tool for diagnosis hypertension and long term managements of hypertension.7) As BP is continuously changing and influenced by many factors, a single reading of office BP doesn't represent patient's BP exactly.15) Home BP measurement provides multiple measurements under relatively controlled condition over long term period. Therefore, multiple home BP measurements represent true BP statue with high reproducibility and predict clinical outcome of hypertension better than office BP measurement and comparable to 24-hour ambulatory BP.7,16) In this survey majority (77.7%) of primary physicians recognized the role of home BP measurement and recommend it in practice. But significantly residents were less likely to recommend, which is thought to originate from their lack of practice.
Several recent studies suggests that high reproducibility of home BP is originated from not only the greater number of measurements but also fixed conditions for home BP measurements such as time of day, resting condition, and constant position. Therefore, encouraging measurement under the fixed condition would improve the reproducibility of home BP.17) However, in our study, only 16.5% of physicians followed home BP measure condition which was recommended by Korean and National Institute of Clinical Excellence guideline of home BP monitoring. Participants agreed with the recommended procedure fairly well except items about how many times should be measured and home BP should be measured just before going to bed. More than half (58.3%) of primary physicians preferred measurements only once a day and less than 20% recommended home BP measurement just before going to bed.
It's necessary to share a standardized home BP procedure among physicians to increase clinical significance and comparability of home BP monitoring.18) But this result indicates discrepancies between guideline and practice in home BP monitoring despite majority primary physicians recommend home BP measurement. Therefore, the promotion of physicians to equip the detail knowledge on the standard procedure is warranted.
There are several limitations in our study including selection bias, relative small number, and the verification of questionnaires. But considering that the subjects of our study were physicians attending educational program with eager interest on hypertension, it is thought to be meaningful that awareness of home BP guideline is poor in this group.
In conclusion, the practice pattern of physicians is consistent with current hypertension guideline except encouraging the limitation of alcohol intake and home BP measurement, although majority of primary physicians recommend home BP measurement. This suggests that the screening on alcohol use and brief counseling by physicians should be encouraged and promoting physicians to know home BP measurement in detail as guideline recommend is needed.
Figures and Tables
References
1. Collins R, Peto R, MacMahon S, Hebert P, Fiebach NH, Eberlein KA, et al. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990. 335:827–838.
2. Trilling JS, Froom J. The urgent need to improve hypertension care. Arch Fam Med. 2000. 9:794–801.

3. Mehta SS, Wilcox CS, Schulman KA. Treatment of hypertension in patients with comorbidities: results from the study of hypertensive prescribing practices (SHyPP). Am J Hypertens. 1999. 12(4 Pt 1):333–340.

4. Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998. 339:1957–1963.

5. Hobbs FD, Erhardt L. Acceptance of guideline recommendations and perceived implementation of coronary heart disease prevention among primary care physicians in five European countries: the Reassessing European Attitudes about Cardiovascular Treatment (REACT) survey. Fam Pract. 2002. 19:596–604.

6. Lee KN, Park CG, Choi CU, Lim HE, Kim EJ, Rha SW, et al. Gap between guideline and real primary practice: treatment in patients with hypertension. J Korean Soc Hypertens. 2010. 16:43–50.
7. Imai Y. Clinical significance of home blood pressure and its possible practical application. J Korean Soc Hypertens. 2012. 18:1–16.

8. The Korean Society of Hypertension. Blood pressure monitoring guidelines [Internet]. 2007. cited 2012 Aug 20. Seoul: The Korean Society of Hypertension;Available from: http://www.koreanhypertension.org/board/list.html?num=280&start=0&sort=top%20desc,reg_dt%20desc&code=info02&key=&keyword=.
10. Ministry of Health and Welfare. The 3rd national health and nutritional survey [Internet]. 2005. cited 2012 Aug 20. Seoul: Ministry of Health and Welfare;Available from: http://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.
11. Ministry of Health and Welfare. The 4th national health and nutritional survey [Internet]. 2008. cited 2012 Aug 20. Seoul: Ministry of Health and Welfare;Available from: http://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.
12. Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation. 2010. 121:1951–1959.

13. Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997. 277:1039–1045.

14. Rubio G, Jimenez-Arriero MA, Martinez I, Ponce G, Palomo T. Efficacy of physician-delivered brief counseling intervention for binge drinkers. Am J Med. 2010. 123:72–78.

15. Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008. 26:1505–1526.

16. Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005. 19:801–807.

17. Imai Y, Ohkubo T, Hozawa A, Tsuji I, Matsubara M, Araki T, et al. Usefulness of home blood pressure measurements in assessing the effect of treatment in a single-blind placebo-controlled open trial. J Hypertens. 2001. 19:179–185.

18. Imai Y, Otsuka K, Kawano Y, Shimada K, Hayashi H, Tochikubo O, et al. Japanese society of hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res. 2003. 26:771–782.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download