Abstract
Background
Methods
Results
Figures and Tables
 | Fig. 1
Plasma concentration-time curves. Valsartan mean plasma concentration versus time profile of response group, non-response group and reverse response group. Values are presented as mean ± standard error of mean. |
Table 3
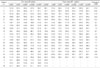
Blood pressure (BP) data of subjects 2, 7, and 16 were lossed during trial.
mSBP, mean systolic blood pressure; mDBP, mean diastolic blood pressure; mdSBP, mean daytime systolic blood pressure; mdDBP, mean daytime diastolic blood pressure; mnSBP, mean nighttime systolic blood pressure; mnDBP, mean nighttime diastolic blood pressure.
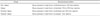
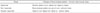
Table 4

Table 5

Diurnal BP pattern, 1 = non dipper (with a BP drop at night time of less than 10%); 2 = dipper (with a BP drop at night time of 10% to 20%); 3 = extreme dipper (with a BP drop at night time of more than 20%); 4 = reverse dipper (with a BP increase at night time).
AUCt, area under the plasma concentration versus time curve from 0 hour to the last measurable concentration; AUCinf, area under the plasma concentration versus time curve extrapolated to infinity; Cmax, maximum plasma concentration; Tmax, time required to reach maximum plasma concentration; BP, blood pressure; SD, standard deviation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download