Abstract
Spontaneous renal hematoma is rare. We report a 43-year-old man presented with sudden left flank pain and severe hypertension. Renal hematoma was confirmed on computed tomography. Renal angiography showed no active bleeding or vascular malformation. Echocardiography showed severe concentric left ventricular hypertrophy. Hypertension was the only cause for the condition. Symptoms and size of the hematoma decreased on antihypertensive medication and conservative treatment. Severe hypertension might have a role for developing renal hematoma.
Spontaneous renal hematoma (SRH) or Wunderlich syndrome is rare condition that perirenal and/or renal subcapsular bleeding without trauma.1,2) Renal neoplasm, such as angiomyolipoma, fibroma, renal cell carcinoma, and metastasis, are one of the most common causes of SRH.3,4) For diagnosis and management of SRH, ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI) are helpful.5) We report a one case of SRH with severe hypertension which was diagnosed 10 years earlier.
A 43-year-old man was admitted to the hospital via emergency department because of sudden left flank pain and severe hypertension without trauma. He had a previous history of hypertension around 10 years earlier, but he had not received further evaluation and treatment. No previous history of renal disease was found. He had a family history of essential hypertension. He did not have fever, hematuria, and trauma recently.
Blood pressure was 250/120 mm Hg on arrival at emergency room. A physical examination showed severe tenderness in the left flank without organomegaly.
Chest radiography showed cardiomegaly and mediastinal widening, however chest CT scan showed severe left ventricular hypertrophy without aortic aneurysm or dissection. An electrocardiogram showed left ventricular hypertrophy. Echocardiogram showed severe left ventricular hypertrophy with borderline left ventricular systolic function (Fig. 1). The left ventricular ejection fraction was 52%.
Ultrasonography demonstrated a fluid collection on the left kidney. CT showed this lesion to be consistent with renal hematoma and small amount of hemoretroperitoneum in left perirenal space with suspicious contrast acute extravasation in lower pole of left kidney (Fig. 2A, B). Urgent renal angiography showed no active bleeding from left kidney.
Laboratory values showed urea 30.5 mg/dL, creatinine 2.04 mg/dL, sodium 139 mmol/L, potassium 2.8 mmol/L, hematocrit 38.5%, hemoglobin 13.0 g/dL, and 18,000 leukocytes/mm3. Coagulation profile was normal. Urine analysis showed microscopic hematuria and proteinuria (4+ and 3+, respectively). Oral antihypertensive therapy was initiated (nifedipine 66 mg/12 hr, bisoprolol 5 mg/day, hydrochlorthiazide 12.5 mg/day, and furosemide 40 mg/day) and blood pressure was normalized. The lowest hemoglobin level was 10.2 g/dL during hospitalization after 3 days from admission. Twenty-four-hour urine collection showed overt proteinuria (700 mg/day) and creatinine clearance was 77.1mL/min. Renal MRI after 7 days to rule out other renal disease showed improved hemoretroperitoneum in left perirenal space without contrast extravasation (Fig. 3).
Plasma cortisol, aldosterone, catecholamine concentration, and plasma renin activity were normal. The 24-hour urinary epinephrine and norepinephrine, and vanillylmandelic acid were also normal. Two month later, his flank pain was reduced much and blood pressure was controlled well with nifedipine 66 mg/12 hr, losartan 50 mg/day, and carvedilol 12.5 mg/day.
Carl Wunderlich is credited with the first clinical description of Wunderlich syndrome in 1856 as spontaneous renal hemorrhage confined to the subcapsular and perinephric space in patients without history of trauma.6) Underlying causes are various, such as tumors, vascular disease, cystic renal disease, infection, nephritis, hematologic disease.2,7) Renal tumors and vascular diseases of the kidney are the most common causes of this syndrome.3,4) Yu et al.2) reported 12 cases of SRH in patients with chronic hemodialysis. Most patients were genetic or acquired cystic disease of kidney in this study. But, other 2 patients were confirmed with renal cell carcinoma.8) Therefore, malignant tumor should be considered in SRH patients. Renal hypertension after SRH has been reported in some cases,9,10) but hypertension itself was very rare for SRH.11,12) Our case showed SRH probably due to severe hypertension with concentric left ventricular hypertrophy. Renal complicated cyst was not found on CT scan, but it was confirmed by MRI without any evidence of malignancy. Katabathina et al.13) reported that MRI may be performed in whom the bleeding source is not identified on initial CT examination. Greater intrinsic soft tissue resolution of MRI allows the detection of perirenal hemorrhage and the underlying cause.13) The bleeding of this case is not related with renal neoplasm or vascular disease of kidney. Left ventricular hypertrophy and renal dysfunction are well known target organ damage for chronic hypertension.14) Our patient has a history of long standing hypertension and a family history of hypertension. The laboratory results of secondary hypertension revealed no abnormal findings. Therefore, this patient could be an essential hypertension with renal dysfunction. However, glomerulonephritis was also considered because of overt proteinuria with renal dysfunction. It was uncertain because renal biopsy was not done. In the acute setting, renal angiography and embolization may be needed to stop active bleeding.15) SRH has been managed successfully with conservative treatment in several studies.11,12) In this case, we performed renal angiography to manage active bleeding, but it was not active and managed well conservatively.
In conclusion, we report one SRH case with severe concentric left ventricular hypertrophy. Severe hypertension could have a role for developing SRH. MRI can be used as an alternative diagnostic tool to differentiate a cause of SRH.
Figures and Tables
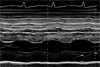 | Fig. 1
M-mode echocardiography at the papillary muscle level. Dilated left ventricular dimension with underlying marked hypertrophy and borderline systolic function (ejection fraction was 52%). Left ventricular end-diastolic dimension was 64 mm. Septal and posterior wall thickness was 22 and 21 mm, respectively. |
 | Fig. 2
Abdominal computed tomography. (A) Transverse plane. (B) Coronal plane. Huge subcapsular hematoma (*) in left kidney with small amount of hemoretroperitoneum (small arrows). Extravasation of contrast at the lower pole (big arrow). |
 | Fig. 3
Contrast enhanced renal magnetic resonance imaging after 7 days. (A) Coronal plane. (B) Magnification of left kidney. Complicated cyst (1.2 × 0.7 cm) with low signal intensity is noted in lower pole without enhancement (big arrow). No change in subcapsular hematoma (*) and decrease in amount of hemoretroperitoneum (small arrows). No evidence of contrast extravasation. |
References
1. Brkovic D, Moehring K, Doersam J, Pomer S, Kaelble T, Riedasch G, et al. Aetiology, diagnosis and management of spontaneous perirenal haematomas. Eur Urol. 1996. 29:302–307.
2. Yu ZX, Xia GP, Hu WH, Chen W, Li XB, Chen HD, et al. Etiology, diagnosis and management of spontaneous per renal hemorrhage. Zhonghua Yi Xue Za Zhi. 2006. 86:39–41.
3. Daskalopoulos G, Karyotis I, Heretis I, Anezinis P, Mavromanolakis E, Delakas D. Spontaneous perirenal hemorrhage: a 10-year experience at our institution. Int Urol Nephrol. 2004. 36:15–19.

4. Zhang JQ, Fielding JR, Zou KH. Etiology of spontaneous perirenal hemorrhage: a meta-analysis. J Urol. 2002. 167:1593–1596.
5. Yip KH, Peh WC, Tam PC. Spontaneous rupture of renal tumours: the role of imaging in diagnosis and management. Br J Radiol. 1998. 71:146–154.

6. Wunderlich CA. Handbuch der pathologie und therapie. 1856. 2nd ed. Stuttgart: Ebner & Seubert.
7. Albi G, del Campo L, Tagarro D. Wunderlich's syndrome: causes, diagnosis and radiological management. Clin Radiol. 2002. 57:840–845.
8. You HY, Song SW, Han CH, Kim JW, Kim YO, Yoon JM, et al. Spontaneous renal rupture in patients on chronic hemodialysis. Korean J Nephrol. 2004. 23:453–458.
9. Boggi U, Berchiolli R, Ferrari M, Di Candio G, Campatelli A, Mosca F. Renal hypertension due to giant perirenal haematoma: permanent resolution by percutaneous ultrasound-guided drainage. Scand J Urol Nephrol. 1998. 32:64–66.
10. Sterns RH, Rabinowitz R, Segal AJ, Spitzer RM. 'Page kidney': hypertension caused by chronic subcapsular hematoma. Arch Intern Med. 1985. 145:169–171.

11. Calvo-Romero JM, Ramos-Salado JL. Spontaneous renal hematoma (Wunderlich syndrome) associated with severe hypertension. J Clin Hypertens (Greenwich). 2003. 5:76–77.
12. Baishya RK, Dhawan DR, Sabnis RB, Desai MR. Spontaneous subcapsular renal hematoma: a case report and review of literature. Urol Ann. 2011. 3:44–46.

13. Katabathina VS, Katre R, Prasad SR, Surabhi VR, Shanbhogue AK, Sunnapwar A. Wunderlich syndrome: cross-sectional imaging review. J Comput Assist Tomogr. 2011. 35:425–433.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download