Abstract
The relationship between salt and hypertension is well established, and salt restriction is widely recommended in the management of hypertension. However, people living in northeast Asia have consumed large amount of salt, and the prevalence of hypertension and the incidence of stroke have been high in that area. Mechanisms of salt-induced hypertension may be complex, but volume expansion in the presence of impaired natriuretic capacity of the kidney and action on the central nervous system and neurohormoral pathways seem to be important. Salt is also involved in changes in blood pressure (BP) caused by other factors, such as weight gain, stress, exercise, potassium, catecholamines, angiotensin, and aldosterone. The interaction between sodium and aldosterone appears to play a critical role in the development of organ damage. The depressor effect of salt restriction in hypertensive patients is well demonstrated although the response of BP varies widely among individuals. Salt restriction decreases BP throughout 24 hours, and its effect may be greater during night compared to daytime in salt-sensitive nondippers. Although excess salt consumption can cause cardiovascular diseases through its effect on BP, recent studied have shown that the association of salt consumption and cardiovascular diseases, such as stroke and heart failure, is independent of BP. Salt reduction is important in the prevention of cardiovascular diseases, however, the effect and safety of aggressive salt restriction remain to be clarified. It is difficult to accomplish and maintain the salt reduction. Both population strategy and individualized approach are important to reduce salt consumption.
Dietary salt intake is well known to be involved in the regulation of body fluid and cardiovascular system.1,2) As excess consumption of salt elevates blood pressure (BP) and causes hypertension, salt reduction is widely recommended in the management of hypertension.3-5) The amount of salt intake as well as the prevalence of hypertension has been traditionally high in northeast Asia, such as Japan, Korea, and northern China.6,7) It is obvious that restriction of salt intake effectively lowers BP in hypertensive patients, and also in normotensive subjects.8,9) However, many hypertensive patients still consume more salt than the level recommended by guidelines.10) It has also been shown that excess intake of salt exerts adverse effects on the cardiovascular system and may be an independent risk factor for several cardiovascular diseases such as stroke and heart failure.11,12) The reduction in salt intake may prevent the number of cardiovascular events and may save the medical cost effectively,13,14) although the results of observation and intervention studies have not been consistent.15,16)
In this review, I will summarize the role of salt in hypertension and cardiovascular diseases and the effects of salt reduction on those disorders. The main component of this article was presented in the plenary lecture at the Autumn Scientific Meeting of Korean Society of Hypertension in Busan, 2011.
A number of epidemiological, experimental, and clinical studies have clearly demonstrated that excessive salt intake is related to increases in BP and the progression of hypertension. For example, amount of salt intake was positively correlated with the level of BP in the INTERSALT study6) (Fig. 1). In this study, BP was low in groups with very low salt intake, and there was little age-related increase in BP in those groups. In contrast, average level of BP and the prevalence of hypertension were high in groups with high salt consumption.
Many but not all models of experimental hypertension are salt-dependent. The models of salt-dependent hypertension include deoxycorticosterone-salt hypertension in rats, Dahl salt-sensitive rats, and reduced renal mass hypertension. Blunted natriuretic capacity of the kidney in combination with high salt intake appears to be the main mechanism of hypertension in those models, although neurohormonal factors may also play a role in the development of hypertension.1,2)
Clinical studies also have shown the elevation of BP with a high-salt diet and the reduction in BP with salt restriction.3,8,9,12,17) However, the increase in BP due to excessive salt intake varies widely among individuals, and hypertensive patients are often classified as salt-sensitive and non-salt-sensitive patients. Many factors including race, genes, renal function, the rennin-angiotensin-aldosterone system, and the sympathetic nervous system are involved in the salt sensitivity of BP.
As shown in the INTERSALT and other studies, the amount of salt intake has been traditionally high in northeast Asia. In the INTERSALT study, salt consumption in Tianjin (northern China), Korea, and Toyama (northern Japan) were the highest in the world6) (Fig. 1). The high salt consumption in northeast Asia was also observed in the INTERMAP study that collected dietary data from 17 populations in China, Japan, UK, and USA.7) In this study, salt intake was relatively high in China and Japan, and relatively low in UK and USA. It also showed that most dietary sodium was from salt added in home cooking in China, and was from soy sauce, processed seafood, salted soups, and preserved vegetables in Japan.18) Processed foods contributed heavily to sodium intake in UK and USA.
However, the amount of salt consumption has been decreasing at least in Japan. Fig. 2 shows recent trend of dietary salt intake in Japan according to the national survey of health and nutrition.19) The average salt consumption in Japanese was 11.7 g/day in 2003, but was 10.6 g/day in 2010. Men consumed more salt than women, however, this difference appears to be due to the amount of food intake. It has been shown that the gender difference of salt intake disappears after adjustment for body weight. Although dietary salt intake has decreased in Japan, the average amount still exceeds 10 g/day. Further effort is required to reduce salt intake to the level of the government guidelines for general citizens (less than 9 g/day for men and less than 7.5 g/day for women).
Restriction of salt intake is widely recommended in the management of hypertension, and most hypertensive patients are aware of the importance of the reduction in dietary salt intake. However, adherence to salt reduction in hypertensive patients has been suboptimal and many patients still consume excessive salt in daily life. Fig. 3 shows the distribution of daily salt intake in hypertensive patients treated at the hypertension clinic of our institute in 2007. Salt intake was estimated from sodium and creatinine concentrations in spot urine using a reported formula.20) Average salt intake in our hypertensive patients was 8.8 g/day, that was less than average salt consumption in general Japanese population but was higher than the level recommended by the Japanese Society of Hypertension (less than 6 g/day).5) Only 10% of patients followed the recommended salt restriction.
Ohta et al.10) assessed the amount of salt intake in salt-conscious and non-salt-conscious patients with hypertension using 24-hour urine collection. In their study, average salt intake in salt-conscious patients (9.4 g/day) was lower than that in non-salt-conscious patients (10.6 g/day). However, the difference was not so remarkable, and most salt-conscious patients consumed more than 6 g of salt per day. These results showed that the salt restriction is suboptimal in hypertensive patients regardless of their awareness of the importance of salt reduction to control BP. Because many salt-conscious patients consume excessive amount of salt, assessment of salt intake in each patient is important in the management of hypertension.21)
It is generally considered that salt elevates BP through an increase in blood volume.22) Blood volume expansion associated with high salt intake is caused by an increase in water intake due to the stimulation of thirst center in the brain and the shift of body fluid due to the osmotic gradient (Table 1). The increase in blood volume increases cardiac output and raises BP. The elevated BP acts on the kidney to promote sodium and water excretion, then body fluid homeostasis is restored at a new set point of BP. In animals and humans with normal renal function, the elevation in BP with high salt intake is small. However, higher BP is necessary to maintain body fluid homeostasis in the case of impaired natriuretic capacity of the kidney. The increase in cardiac output is initially responsible for the BP elevation, but the chronic phase of salt-induced hypertension is maintained mostly by the increase in vascular resistance.
Another mechanism of the salt-induced BP elevation is through an increase in sodium concentration in the blood, cerebrospinal fluid (CSF), and brain tissue (Table 1). Intracerebroventricular injection of hypertonic sodium chloride increases BP via activation of the sympathetic nervous system.23) An increase in vasopressin release may also play a role in this hypertensive response. Chronic intracerebroventricular infusion of hypertonic sodium chloride is also able to cause sustained BP elevation, although the hypertensive effect is moderate in animals with intact kidneys.24) Endogenous digitalis like substance(s) that cause vasoconstriction and natriuresis may play an important role in the salt-induced hypertension.25) The changes in sodium concentration in the blood and CSF occur during physiological changes in salt intake. We observed that the levels of serum and CSF sodium were higher during high salt intake than low salt period in hypertensive patients, although the differences were not different between salt-sensitive and non-salt-sensitive patients.26)
Salt plays an important role in the elevation and reduction in BP caused by many other factors (Table 2). Hypertension in renal dysfunction is caused by sodium retention due to impaired natriuretic capacity of the kidney. Angiotensin and aldosterone act on the renal tubules to stimulate sodium reabsorption.27,28) The sympathetic nervous system and catecholamines except dopamine promote sodium retention by actions on the renal vasculature and tubules, and renin release.29) Sodium retention is also involved in the BP elevation by weight gain and stress.30)
A number of studies have demonstrated that the reduction of salt intake decreases BP in humans.8,9) The depressor effect of salt reduction is greater in hypertensive patients than normotensive subjects. In a meta-analysis of randomized studies of moderate salt reduction, BP in hypertensive patients decreased by 5.0/2.7 mm Hg with restriction of dietary salt from 9.5 g/day to 5.1 g/day8) (Fig. 4). In normotensive subjects, the decrease in BP is about a half of that in hypertensive patients. Therefore, systolic BP decreases about 1 mm Hg in hypertensive patients and about 0.5 mm Hg in normotensive subjects for each 1 g/day of salt reduction.
However, there are large variations in the salt sensitivity of BP among hypertensive patients as well as in normotensive subjects. Many factors, such as race, genes, renal function, the rennin-angiotensin-aldosterone system, and the sympathetic nervous system, are involved in the salt sensitivity of BP.9) Subjects with severe hypertension, older age, black race, renal dysfunction, low plasma rennin activity, and high plasma aldosterone are generally salt sensitive.9,34) The salt sensitivity of Oriental subjects seems to be intermediate between black and white subjects. Recent studies have shown that several genetic variants in the rennin-angiotensin-aldosterone system, CYP 3A5 gene, and ABCB1 gene are involved in the salt sensitivity of BP.35-38)
The depressor effect of salt reduction is apparent throughout the day, and the reductions in BP during daytime and nighttime are usually similar in hypertensive patients.39) However, the effect may be greater during nighttime than during daytime in some hypertensive patients. It was reported that salt reduction converted nondippers to dippers in salt-sensitive patients with hypertension.40) The effect on nighttime BP may have clinical relevance since the nondipping status is associated with poor cardiovascular outcome.41)
Salt reduction is important for both untreated and treated hypertensive patients as well as for subjects with high normal BP. However, effects of salt reduction on BP are different according to administered antihypertensive drugs. The depressor effect is small in patients taking diuretics, moderate in those taking calcium antagonists, greater in those taking sympatholytic agents, and the greatest in patients treated with inhibitors of the renin-angiotensin system. A recent study demonstrated that moderate salt reduction is more effective than an angiotensin receptor blocker in patients treated with an angiotensin converting enzyme inhibitor.42) It has also been shown that salt reduction markedly lowers BP in patients with resistant hypertension.43)
It is obvious that excessive salt intake promotes cardiovascular damage through an increase in BP. However, it has been shown that dietary salt exerts adverse effects on the cardiovascular system independently of BP and is also related to several non-cardiovascular diseases9,12) (Table 3).
Excessive salt intake causes left ventricular hypertrophy and fibrosis, resulting in cardiac dysfunction. An independent association of dietary sodium intake with left ventricular mass index has been observed in epidemiological studies.44,45) In an experimental study, salt loading increased left ventricular mass and caused ventricular fibrosis, systolic and diastolic dysfunction, and heart failure in spontaneously hypertensive rats.46)
Regarding vascular damage, it has been shown that high dietary salt decreases plasma nitrate and nitrite and impairs endothelial function in humans.47,48) The salt-induced endothelial dysfunction and damage may promote structural changes in arteries and kidney disease.49) High sodium intake has been associated with increased carotid intima-media thickness in obese subjects, and with central pulse pressure and augmentation index in hypertensive patients.50,51)
Experimental studies have shown that aldosterone is necessary in salt-induced organ damage.28,52) It has also been shown that salt is necessary in aldosterone-induced organ damage.28,52) Therefore, interaction between salt and aldosterone appears to play an important in the development of organ damage and cardiovascular disease. Although plasma level of aldosterone is suppressed by high salt intake, cardiovascular level of aldosterone may increase with sodium loading.53)
Salt is related to cardiovascular diseases through its BP increasing effect, but the association of dietary salt intake with several cardiovascular diseases has been shown to be independent of BP. In a prospective study in Finland, mortality from ischemic heart disease, stroke, and all cause increased with increases in salt intake after correction of BP and other factors.54) Other studies also showed that salt intake was independent risk factor of heart failure and stroke (Fig. 5).55,56) In a meta-analysis of prospective studies, high salt intake was associated with increased risk of stroke and total cardiovascular disease.16) Therefore, salt excess is considered to confer a greater risk of cardiovascular diseases that would be expected by a mere increase in BP.
However, several studies did not support the beneficial effect of low salt intake in the prevention of cardiovascular diseases. Alderman et al.57) observed an association of low urinary sodium with greater risk of myocardial infarction among treated hypertensive patients. In a combined analysis of two population-based cohort in Europe, low sodium excretion was associated with higher cardiovascular mortality.11) In an observational analyses of two cohort included in Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial and Telmisartan Randomized Assessment Study in Angiotensin-converting Enzyme Intolerant Subjects with Cardiovascular Disease Trial, the association between estimated sodium excretion and cardiovascular events was J-shaped with a nadir of 4 to 6 g/day.58)
There are few randomized clinical trials that examined the effect of salt reduction on cardiovascular morbidity and mortality as primary end points. In an observational follow-up study of the trials of hypertension prevention, risk of a cardiovascular event was lower in salt reduction intervention group than control group.13) In a recent meta-analysis of randomized trials, the beneficial effect of salt restriction on cardiovascular morbidity or all-cause mortality was not significant, and salt restriction increased the risk of all-cause mortality in those with heart failure.59) However, He and MacGregor60) criticized this meta-analysis and showed significant reduction in the risk of cardiovascular events with salt reduction in combining hypertensive and normotensive subjects.61)
Taken together, it is obvious that excessive dietary salt intake increases the risk of cardiovascular diseases and salt reduction may decrease cardiovascular morbidity and mortality. However, the effect and safety of aggressive salt restriction remain to be clarified.
Dietary salt intake is closely related to hypertension, and salt reduction is important in the prevention and management of hypertension. However, people living in northeast Asia traditionally consumed large amount of salt, and the prevalence of hypertension has been high in that area. The depressor effect of salt restriction is well demonstrated although the response of BP varies among individuals. Salt restriction decreases BP throughout 24 hours, and its effect may be greater during night compared to daytime in salt-sensitive nondippers. Mechanisms of salt-induced hypertension include blood volume expansion and action on the central nervous system. The impairment of natriuretic capacity of the kidney may play a critical role in salt-induced hypertension. Salt is also involved in increase or decrease in BP caused by other factors, such as weight gain, stress, exercise, potassium, catecholamines, angiotensin, and aldosterone. The interaction between sodium and aldosterone appears to be important in the development of organ damage. Although excess salt consumption can cause cardiovascular diseases through its effect on BP, the association of salt and cardiovascular diseases, such as stroke and heart failure, may be independent of BP. Therefore, salt reduction is important in the prevention of cardiovascular diseases, however, the effect and safety of aggressive salt restriction remain to be clarified.
It has been suggested that population-wide reduction in salt intake prevents a number of cardiovascular events and saves quite large amount of medical cost.14) To reduce salt consumption at the population level, strategies targeting government, industry, general persons, and whole hypertensive patients are primarily important. Activities such as World Action on Salt and Health will help to reduce dietary salt worldwide.61) However, there are difficulties to accomplish and maintain salt reduction in hypertensive patients. One reason is the lack of assessment of individual salt intake in usual hypertension care. The individual assessment of salt intake may be helpful to both hypertensive patients and their physicians for effective salt reduction. The Salt Reduction Working Group of the Japanese Society of Hypertension published a report regarding assessment of salt intake in the management of hypertension.21) With both population strategy and individualized approach, salt consumption in northeast Asia will decrease further, resulting in BP reduction in normotensive subjects and hypertensive patients, and the decrease in cardiovascular diseases in that area.
Figures and Tables
Fig. 1
Relationship between salt intake and systolic blood pressure (BP) (Modified from Intersalt Cooperative Research Group. BMJ. 1988;297:319-28).6)
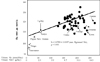
Fig. 2
Recent trend of salt consumption in Japan (Modified from Anderson, et al. J Am Diet Assoc. 2010;110:736-45, with permission from).18)
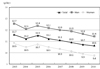
Fig. 3
Distribution of estimated salt intake in treated hypertensive patients at the Hypertension Clinic of National Cerebral and Cardiovascular Center in 2007.
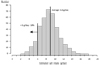
Fig. 4
Effects of moderate salt reduction on blood pressureBP according to a meta-analysis of randomized clinical trials (From He and MacGregor. J Hum Hypertens. 2002;16:761-70, with permission from).8)

Fig. 5
Salt intake and stroke mortality in Japanese men and women (From Nagata, et al. Stroke. 2004;35:1543-7, with permission from).56)

References
1. Hamlyn JM, Blaustein MP. Sodium chloride, extracellular fluid volume, and blood pressure regulation. Am J Physiol. 1986. 251(4 Pt 2):F563–F575.

2. Folkow B, Ely DL. Dietary sodium effects on cardiovascular and sympathetic neuroeffector functions as studied in various rat models. J Hypertens. 1987. 5:383–395.

3. Adrogue HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007. 356:1966–1978.

4. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007. 25:1105–1187.
5. Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res. 2009. 32:3–107.
6. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988. 297:319–328.
7. Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, et al. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003. 17:623–630.

8. He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials: implications for public health. J Hum Hypertens. 2002. 16:761–770.

9. Kawano Y, Ando K, Matsuura H, Tsuchihashi T, Fujita T, Ueshima H, et al. Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: (1) Rationale for salt restriction and salt-restriction target level for the management of hypertension. Hypertens Res. 2007. 30:879–886.

10. Ohta Y, Tsuchihashi T, Ueno M, Kajioka T, Onaka U, Tominaga M, et al. Relationship between the awareness of salt restriction and the actual salt intake in hypertensive patients. Hypertens Res. 2004. 27:243–246.

11. Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009. 339:b4567.

12. He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009. 23:363–384.

13. Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007. 334:885–888.

14. Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010. 362:590–599.

15. Alderman MH, Cohen H, Madhavan S. Dietary sodium intake and mortality: the National Health and Nutrition Examination Survey (NHANES I). Lancet. 1998. 351:781–785.

16. Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerova J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011. 305:1777–1785.

17. Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med. 1978. 64:193–198.

18. Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010. 110:736–745.

19. Ministry of Health, Labor, and Welfare. Summary of the national survey of health and nutrition in 2010 [Internet]. 2012. cited 2012 Jun 4. Tokyo: Ministry of Health, Labor, and Welfare;Available from: http://www.mhlw.go.jp/stf/houdou/2r98520000020qbb-att/2r98520000021c0o.pdf.
20. Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002. 16:97–103.

21. Kawano Y, Tsuchihashi T, Matsuura H, Ando K, Fujita T, Ueshima H, et al. Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: (2) Assessment of salt intake in the management of hypertension. Hypertens Res. 2007. 30:887–893.

22. Guyton AC. Arterial pressure and hypertension. Circulatory physiology, 3. 1980. Philadelphia: Saunders.
23. Kawano Y, Ferrario CM. Neurohormonal characteristics of cardiovascular response due to intraventricular hypertonic NaCl. Am J Physiol. 1984. 247(3 Pt 2):H422–H428.

24. Kawano Y, Sudo RT, Ferrario CM. Effects of chronic intraventricular sodium on blood pressure and fluid balance. Hypertension. 1991. 17:28–35.

25. de Wardener HE, MacGregor GA. Dahl's hypothesis that a salureic substance may be responsible for a sustained rise in arterial pressure: its possible role in essential hypertension. Kidney Int. 1980. 18:1–9.
26. Kawano Y, Yoshida K, Kawamura M, Yoshimi H, Ashida T, Abe H, et al. Sodium and noradrenaline in cerebrospinal fluid and blood in salt-sensitive and non-salt-sensitive essential hypertension. Clin Exp Pharmacol Physiol. 1992. 19:235–241.

27. Hall JE. Control of sodium excretion by angiotensin II: intrarenal mechanisms and blood pressure regulation. Am J Physiol. 1986. 250(6 Pt 2):R960–R972.

28. Briet M, Schiffrin EL. Aldosterone: effects on the kidney and cardiovascular system. Nat Rev Nephrol. 2010. 6:261–273.

29. DiBona GF. Sympathetic nervous system influences on the kidney: role in hypertension. Am J Hypertens. 1989. 2(3 Pt 2):119S–124S.
32. Fujita T, Sato Y. Natriuretic and antihypertensive effects of potassium in DOCA-salt hypertensive rats. Kidney Int. 1983. 24:731–739.

33. Luft FC. Putative mechanism of blood pressure reduction induced by increases in dietary calcium intake. Am J Hypertens. 1990. 3(8 Pt 2):156S–160S.

34. Weinberger MH. Sodium sensitivity of blood pressure. Curr Opin Nephrol Hypertens. 1993. 2:935–939.

35. Yamagishi K, Tanigawa T, Cui R, Tabata M, Ikeda A, Yao M, et al. High sodium intake strengthens the association of ACE I/D polymorphism with blood pressure in a community. Am J Hypertens. 2007. 20:751–757.

36. Gu D, Kelly TN, Hixson JE, Chen J, Liu D, Chen JC, et al. Genetic variants in the renin-angiotensin-aldosterone system and salt sensitivity of blood pressure. J Hypertens. 2010. 28:1210–1220.

37. Iwai N, Kajimoto K, Tomoike H, Takashima N. Polymorphism of CYP11B2 determines salt sensitivity in Japanese. Hypertension. 2007. 49:825–831.
38. Eap CB, Bochud M, Elston RC, Bovet P, Maillard MP, Nussberger J, et al. CYP3A5 and ABCB1 genes influence blood pressure and response to treatment, and their effect is modified by salt. Hypertension. 2007. 49:1007–1014.
39. Kawano Y, Abe H, Kojima S, Yoshimi H, Sanai T, Kimura G, et al. Different effects of alcohol and salt on 24-hour blood pressure and heart rate in hypertensive patients. Hypertens Res. 1996. 19:255–261.

40. Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1997. 96:1859–1862.

41. Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension. 1994. 24:793–801.

42. Slagman MC, Waanders F, Hemmelder MH, Woittiez AJ, Janssen WM, Lambers Heerspink HJ, et al. Moderate dietary sodium restriction added to angiotensin converting enzyme inhibition compared with dual blockade in lowering proteinuria and blood pressure: randomised controlled trial. BMJ. 2011. 343:d4366.

43. Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009. 54:475–481.
44. du Cailar G, Ribstein J, Mimran A. Dietary sodium and target organ damage in essential hypertension. Am J Hypertens. 2002. 15:222–229.

45. Jin Y, Kuznetsova T, Maillard M, Richart T, Thijs L, Bochud M, et al. Independent relations of left ventricular structure with the 24-hour urinary excretion of sodium and aldosterone. Hypertension. 2009. 54:489–495.

46. Ahn J, Varagic J, Slama M, Susic D, Frohlich ED. Cardiac structural and functional responses to salt loading in SHR. Am J Physiol Heart Circ Physiol. 2004. 287:H767–H772.

47. Bragulat E, de la Sierra A, Antonio MT, Jimenez W, Urbano-Marquez A, Coca A. Effect of salt intake on endothelium-derived factors in a group of patients with essential hypertension. Clin Sci (Lond). 2001. 101:73–78.

48. Dickinson KM, Clifton PM, Keogh JB. Endothelial function is impaired after a high-salt meal in healthy subjects. Am J Clin Nutr. 2011. 93:500–505.

49. Sanders PW. Salt intake, endothelial cell signaling, and progression of kidney disease. Hypertension. 2004. 43:142–146.

50. Njoroge JN, El Khoudary SR, Fried LF, Barinas-Mitchell E, Sutton-Tyrrell K. High urinary sodium is associated with increased carotid intima-media thickness in normotensive overweight and obese adults. Am J Hypertens. 2011. 24:70–76.

51. Park S, Park JB, Lakatta EG. Association of central hemodynamics with estimated 24-h urinary sodium in patients with hypertension. J Hypertens. 2011. 29:1502–1507.

52. Blasi ER, Rocha R, Rudolph AE, Blomme EA, Polly ML, McMahon EG. Aldosterone/salt induces renal inflammation and fibrosis in hypertensive rats. Kidney Int. 2003. 63:1791–1800.

53. Takeda Y, Yoneda T, Demura M, Furukawa K, Miyamori I, Mabuchi H. Effects of high sodium intake on cardiovascular aldosterone synthesis in stroke-prone spontaneously hypertensive rats. J Hypertens. 2001. 19(3 Pt 2):635–639.

54. Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P, et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001. 357:848–851.

55. He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Dietary sodium intake and incidence of congestive heart failure in overweight US men and women: first National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Arch Intern Med. 2002. 162:1619–1624.
56. Nagata C, Takatsuka N, Shimizu N, Shimizu H. Sodium intake and risk of death from stroke in Japanese men and women. Stroke. 2004. 35:1543–1547.

57. Alderman MH, Madhavan S, Cohen H, Sealey JE, Laragh JH. Low urinary sodium is associated with greater risk of myocardial infarction among treated hypertensive men. Hypertension. 1995. 25:1144–1152.

58. O'Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011. 306:2229–2238.
59. Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease: a meta-analysis of randomized controlled trials (Cochrane review). Am J Hypertens. 2011. 24:843–853.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download