Abstract
Renal artery stenosis is a cause of secondary hypertension which can be cured by surgical or radiological intervention such as percutaneous transluminal renal artery stent placement. In this case we present a subcapsular hematoma of the kidney, a complication following percutaneous transluminal stent placement in the renal artery. Reperfusion injury to the kidney may be a possible mechanism of subcapsular hematoma of the kidney. Long standing severe renal artery stenosis and high pre- and post-procedure pressure gradient might contribute to the complication.
Go to : 
Renal artery stenosis is a cause of secondary hypertension which can be cured by surgical or radiological intervention such as percutaneous transluminal renal artery stent placement1). Complications related to the procedure have minimal or no clinical significances. Hyperperfusion syndrome is a rare complication following revascularization of the internal carotid artery2). In case of renal artery stenosis, reperfusion injury may lead to the same complication in the kidney after revascularization.
Subcapsular hematoma of the kidney, an accumulation of blood between the renal parenchymal surface and the surrounding fibrous capsule, occurs most often secondary to post-traumatic bleeding. Although the incidence of subcapsular hematoma following percutaneous transluminal stent placement has been considered rare, we experienced a case whose radiological signs and clinical symptoms were consistent with subcapsular hematoma of the kidney following the procedure. This report is presented to propose the possibility of such a complication associated with the procedure, especially under the state of chronic hypoxia.
Go to : 
A 59-year-old man was admitted for a follow-up evaluation and treatment of his renal artery stenosis, which was diagnosed one year prior to his admission. At that time, narrowing of the proximal portion of the right renal artery was discovered by abdominal magnetic resonance imaging. His hypertension was classified as the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) stage 2. He had been medicated with the following antihypertensive drugs: nifedipine, 90 mg; carvediol, 25 mg; eprosartan, 600 mg; doxazocin, 8 mg; hydralazine, 25 mg; metolazone, 5 mg; and aspirin, 100 mg.
On admission, he complained of intermittent occipital headache and orthopnea. On physical examination, an abdominal bruit was heard at his epigastric area and the rest of the findings were unremarkable. The vital signs on admission were as follows: blood pressure, 150/90 mmHg with medication; temperature, 36.5℃; pulse, 55 bpm; and respiratory rate, 23/min. The laboratory findings on admission are unremarkable except for a 2 positive proteinuria on his urinalysis.
Arteriography of abdominal aorta showed more than 90% narrowing of his right renal artery at the ostium (Fig. 1). Pressure gradient of the aorta and both renal arteries were as follows: aorta, 179/80 mmHg; left renal artery, 153/76 mmHg; and right renal artery, 35/23 mmHg. An 8 Fr guiding catheter was placed at the distal portion of the right renal artery, and a 5 mm×14 mm Corinthian stent (Cordis Endovascular/Johnson & Johnson, Miami, FL, USA) was placed at the stenotic area of the right renal artery (Fig. 2). Pressure gradient of the aorta and right renal artery were reexamined; they were 205/95 mmHg and 192/90 mmHg, respectively.
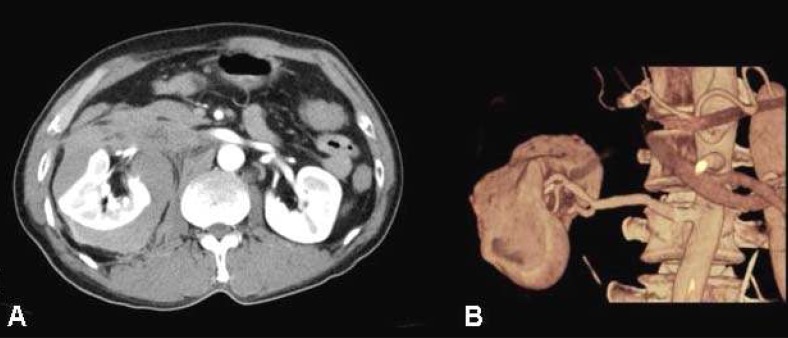
Approximately 2 hours after the procedure, the patient complained of severe pain in his right flank with diaphoresis. His blood pressure was elevated to 190/100 mmHg. An emergency contrast enhanced computed tomography (CT) revealed a large right perirenal subcapsular hematoma and compression of that kidney (Fig. 3A, B). The patient was transferred to the intensive care unit for further treatment. Three hours after the stenting procedure, his hemoglobin level dropped to 7.5 g/dL. Three units of blood were transfused and an angiotensin receptor blocker (eprosartan 600 mg) for hypertension was prescribed. Ten days later, a follow-up contrast enhanced CT examination revealed that the compression of renal parenchyma was much improved. His blood pressure fell to 120/75 mmHg without medication. Following the treatment, the patient's general condition became stable and he was discharged without antihypertensive medication.
Go to : 
Approximately 3-5% of the hypertensive population has renovascular lesions as the etiology. Aging and coexisting atherosclerosis are also known to have significant effects on the prevalence of renovascular hypertension in this population3). Percutaneous transluminal renal artery stent placement, when performed by experienced hands, has been regarded as a safe and effective procedure4). The technical success rate ranges from 96% to 100%, with complications occurring in 13% of the cases5). Mortality related to this procedure is extremely rare, ranging 0-0.5% immediately following the procedure and 1% in the 30-day follow up period1, 3, 5).
Axelrod et al.6) have reported a case of guide wire perforation that led to a fatal perirenal hemorrhage from the transcortical collaterals after renal artery stent placement. Since there was no evidence of injury provoked by the guide wire in this case, the cause for the subcapsular hematoma was postulated to be secondary to the reperfusion injury, such as seen in increased intrarenal pressure. The pressure gradient of right renal artery before and after stenting were 35/23 mmHg and 192/90 mmHg, respectively. The intrarenal pressure was markedly increased after renal artery stent placement.
In case of cerebral hyperperfusion syndrome, the risk factors are considered as long standing high grade carotid artery stenosis, loss of cerebral reserve capacity, and marked increased post-intervention flow velocities in the ipsilateral cerebral artery2). In our case, the patient had long-standing severe renal artery stenosis and high pre- and post-procedure pressure gradient. Subsequent renal subcapsular hematoma, therefore, might have occurred.
In conclusion, this case suggests the possibility of reperfusion injury to the kidney after percutaneous transluminal renal artery stent placement of severe long-standing renal artery stenosis.
Go to : 
References
1. Ivanovic V, McKusick MA, Johnson CM 3rd, Sabater EA, Andrews JC, Breen JF, Bjarnason H, Misra S, Stanson AW. Renal artery stent placement: complications at a single tertiary care center. J Vasc Interv Radiol. 2003; 14:217–225. PMID: 12582190.

2. Nikolsky E, Patil CV, Beyar R. Ipsilateral intracerebral hemorrhage following carotid stent-assisted angioplasty: a manifestation of hyperperfusion syndrome-a case report. Angiology. 2002; 53:217–223. PMID: 11952114.
3. Martin LG, Rundback JH, Sacks D, Cardella JF, Rees CR, Matsumoto AH, Meranze SG, Schwartzberg MS, Silverstein MI, Lewis CA. Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for angiography, angioplasty, and stent placement in the diagnosis and treatment of renal artery stenosis in adults. J Vasc Interv Radiol. 2002; 13:1069–1083. PMID: 12427805.

4. Perkovic V, Thomson KR, Mitchell PJ, Gibson RN, Atkinson N, Field PL, Becker GJ. Treatment of renovascular disease with percutaneous stent insertion: long-term outcomes. Australas Radiol. 2001; 45:438–443. PMID: 11903175.

5. Isles CG, Robertson S, Hill D. Management of renovascular disease: a review of renal artery stenting in ten studies. QJM. 1999; 92:159–167. PMID: 10326075.

6. Axelrod DJ, Freeman H, Pukin L, Guller J, Mitty HA. Guide wire perforation leading to fatal perirenal hemorrhage from transcortical collaterals after renal artery stent placement. J Vasc Interv Radiol. 2004; 15:985–987. PMID: 15361567.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download