Abstract
Roux-en-Y (RY) hepaticojejunostomy (HJ) is a critical component of complex hepatobiliary operations, and it is the treatment of choice for post-cholecystectomy biliary strictures (PCBS). Complications related to the Roux limb, particularly those leading to cholangitis, can severely compromise outcomes. We present a case of a 54-year-old lady who had previously undergone two HJ procedures for recurrent PCBS. The same Roux limb had been used in each of the operations. Short Roux/Roux reflux syndrome led to recurrent cholangitis in this patient, as proven by the reflux of oral contrast into the biliary tree on imaging. This was effectively treated by lengthening the Roux limb (60 cm) with a redo-jejunojejunostomy, and creation of a Nakajo type valve. One-year post surgery, the patient remains well at follow-up. Enteric reflux into the biliary tree may lead to refractory cholangitis. We present the first ever case in an adult, where a simple and effective modification to the HJ obviated this complication.
The creation of a Roux-en-Y hepaticojejunostomy (RYHJ) is an integral component of most hepatobiliary operations. Tenets of this procedure include the creation of a durable jejunojejunostomy and a tension-free anastomosis using a long hepatic limb of up to 75 cm.1 While this surgery remains the gold standard for biliary anastomoses, its associated morbidities include biliary leak, cholangitis, bleeding, anastomotic strictures and biliary cirrhosis.1 A long hepatic limb has been recommended purportedly to decrease the risk for enterobiliary reflux–causing cholangitis, but has been found to be ineffective in various reports.1
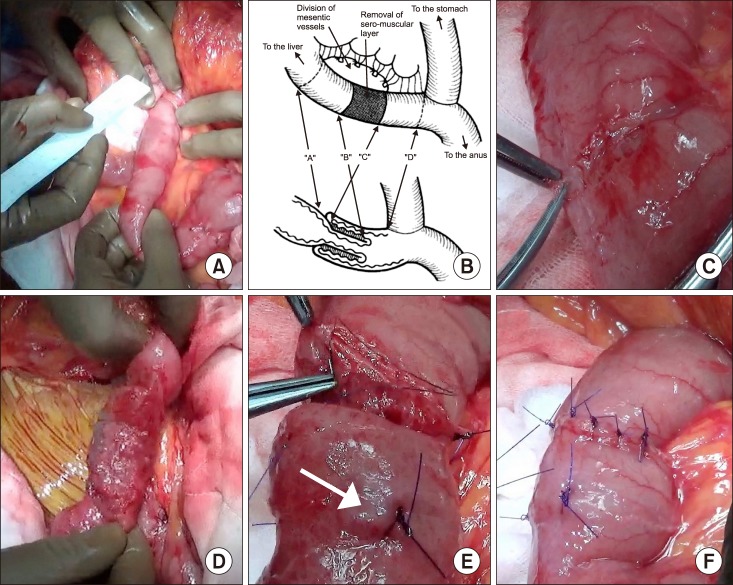
A 54-year-old lady presented to our unit with recurrent episodes of fever and jaundice over a 3-year period. She had previously undergone laparoscopic cholecystectomy in 2013, and developed a bile leak in the postoperative period which evolved into a biliary stricture. Following a failed endoscopic retrograde cholangiopancreatography (ERCP), and with a diagnosis of Strasberg Type E2 injury, she underwent a RYHJ. One year after the biliary anastomosis, she developed a recurrence of the stricture, and underwent a re-HJ using the same Roux loop. On further follow-up, she had progressively worsening liver function tests. Magnetic resonance cholangiopancreatography (MRCP) did not show any ductal dilatation. At presentation, her liver function tests were remarkable for a marginally elevated gamma glutamyl transpeptidase (γGGT) (160 IU/L). MRCP was unremarkable with no evidence of ductal dilatation. Abdominal computed tomography (CT) with oral contrast showed a reflux of the contrast into the biliary tree across a patent HJ anastomosis (Fig. 1). At laparotomy, the hepatic limb of the RYHJ was found to be 25 cm (Fig. 2A). The previous jejunojejunostomy (JJ) was taken down and a new JJ was fashioned to achieve a hepatic limb length of 60 cm. A Nakajo type valve was formed by creating an artificial intussusception in the hepatic limb (Fig. 2B-F) to prevent retrograde flow of enteric contents.2 Her postoperative course was uneventful, and she was discharged home on the 5th day. On follow-up, one year after the surgery, she has been well with normal liver function tests.
In the presence of a patent RYHJ anastomosis, the precise mechanism through which cholangitis occurs has not been established.1 The “ascending theory” is supported by the presence of identical organisms in the liver and intestinal conduits on percutaneous transhepatic drainage, and hence the premise of an enteric reflux across the hepatic limb of the RYHJ.23 The assumption that a longer limb would prevent this phenomenon led to lengthening of the Roux limb to 60–75 cm as one of the techniques to reduce the risk of reflux; this has resulted in disparate results.1 The first reports of antireflux valves to prevent cholangitis resulted from the experience with cholangitis after the Kasai procedure, several modifications have been made to the technique of portoenterostomy to incorporate the antireflux valve.2345 Nakajo et al. first advocated the addition of an intussusception-type antireflux valve into the bilioenteric conduit, and they were able to demonstrate a reduction in the incidence of cholangitis.23
Several experimental studies have shown that intussusception type valves and mucosal-flap valves prevent reflux of intestinal contents into the RY limb.2 Clinical studies using barium found no reflux of contrast material into the hepatic hilum in patients with these valves, as compared to reflux of contrast material in over half of the patients who did not have them.3 Unfortunately, these antireflux valves are not infallible; few reports in the paediatric population suggest failure of the valves and no decrease in the incidence of cholangitis.45
We performed both above mentioned measures to avoid reflux; lengthening of the hepatic limb and an antireflux valve. While the patient is symptom free and has had no further episodes of cholangitis over the past one year, we cannot confirm which of the two measures were actually responsible for the effect. It may likely be that both measures contributed to the patient's recovery and wellbeing.
We report the first ever case of successful use of an antireflux valve to prevent enteric reflux and hence cholangitis in a post RYHJ adult patient. Further, studies on this aspect will shed more light and help support/refute our findings.
References
1. Felder SI, Menon VG, Nissen NN, Margulies DR, Lo S, Colquhoun SD. Hepaticojejunostomy using short-limb Roux-en-Y reconstruction. JAMA Surg. 2013; 148:253–257. discussion 257-258. PMID: 23553273.

2. Nakajo T, Hashizume K, Saeki M, Tsuchida Y. Intussusceptiontype antireflux valve in the Roux-en-Y loop to prevent ascending cholangitis after hepatic portojejunostomy. J Pediatr Surg. 1990; 25:311–314. PMID: 2313499.

3. Honna T, Tsuchida Y, Kawarasaki H, Utsuki T, Mizuta K. Further experience with the antireflux valve to prevent ascending cholangitis in biliary atresia. J Pediatr Surg. 1997; 32:1450–1452. PMID: 9349766.

4. Sartorelli KH, Holland RM, Allshouse MJ, Karrer FM, Lilly JR. The intussusception antireflux valve is ineffective in preventing cholangitis in biliary atresia. J Pediatr Surg. 1996; 31:403–406. PMID: 8708912.

5. Ogasawara Y, Yamataka A, Tsukamoto K, Okada Y, Lane GJ, Kobayashi H, et al. The intussusception antireflux valve is ineffective for preventing cholangitis in biliary atresia: a prospective study. J Pediatr Surg. 2003; 38:1826–1829. PMID: 14666478.

Fig. 1
Abdominal CT with oral contrast showing biliary reflux of contrast across the hepatic limb of Roux-en-Y hepaticojejunostomy.

Fig. 2
Operative findings. (A) Excessively shortened Roux limb (25 cm) from the previous two biliary reconstructive surgeries. (B) Schematic representation of the construction of Nakajo antireflux valve. (C and D) Intraoperative images showing creation of the antireflux valve. A segment of the bowel is denuded of its serosa. (E) Downstream invagination of the bowel to form the antireflux valve. An arrow indicates the full thickness stitch holding the intussusception in place, and (F) The completed antireflux valve.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download