Abstract
Gestational choriocarcinoma is a rare and aggressive type of gestational trophoblastic neoplasia, which is characterized by early vascular invasion and widespread metastases. Choriocarcinoma metastasizes hematogenously, and bleeding from metastases is common. Splenic rupture from a metastatic tumour is exceedingly rare, with only a few reports. We report a case of a 41-year-old female presenting with acute abdomen and haemorrhagic shock secondary to splenic rupture from metastatic choriocarcinoma, which was managed with emergency laparoscopic splenectomy.
Metastatic choriocarcinoma is an aggressive disease with a high mortality rate. Metastases from choriocarcinoma are highly vascular and they present with bleeding in the affected area. However, splenic metastases are still very uncommonly observed. This patient presented with features suggestive of a ruptured ectopic pregnancy, necessitating a diagnostic laparoscopy and washout. A computed tomography scan was performed only when she became haemodynamically unstable again, and it revealed ruptured splenic metastases with haemoperitoneum. This is a rare presentation of the disease that was managed successfully with a minimally invasive approach.
A 41-year-old lady presented with sudden onset lower abdominal pain. She had a single episode of vomiting. There was no significant past medical history except for mild intermittent abdominal discomfort. She was married with two children and her last menstrual period was three weeks ago. She was afebrile with systolic blood pressure of 120 mmHg and heart rate of 113 beats per minute. She appeared pale and lethargic. Her abdomen revealed generalised tenderness with guarding over the suprapubic region. A bedside ultrasound revealed free fluid in the abdomen. Blood tests revealed a hemoglobin level of 5.5 g/dl with a normal platelet count, renal function, liver function, amylase and coagulation screen. Her serum human chorionic gonadotropin (hCG) level was 508,017 mIU/ml.
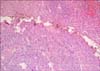
In view of the anemia, tachycardia, abdominal pain, free fluid and raised β-hCG, a ruptured ectopic pregnancy was suspected and an emergency diagnostic laparoscopy with evacuation of the uterus was planned. Intraoperatively, hemoperitoneum and a bleeding left corpus luteum cyst were evident. There was no ectopic pregnancy. Bilateral fallopian tubes appeared normal but were ligated as per the patient's request. The uterus was evacuated and had minimal tissue. Postoperatively, her hemodynamic parameters did not return to normal, and hence, a computed tomography (CT) scan of the thorax, abdomen and pelvis was performed. It showed subcapsular lesions in the spleen with intraperitoneal rupture and hemoperitoneum. CT scan also revealed metastatic nodules in both lungs and liver. Pulmonary embolism was also noted in the right anterior segmental pulmonary artery. An emergency laparoscopic splenectomy was performed (Fig. 1). Histology confirmed splenic metastases secondary to choriocarcinoma (Fig. 2). The tumour infiltrated through the splenic capsule, and immunohistochemistry showed positive stains for cytokeratin (AE1/AE3), hCG and human placental lactogen.
Postoperative day 1 and day 3 drain amylase levels were normal and the abdominal drain was removed on the third day. She was stable and had an uneventful recovery until she suddenly developed melena on the fifth post-operative day. An urgent gastroscopy revealed bleeding from a tumour in the 3rd part of the duodenum, and endoscopic haemostasis was performed (Fig. 3). An urgent CT mesenteric angiogram did not reveal any active bleeding or intra-abdominal collection. CT scan showed a new enhancing mass in the duodenum, proximal jejunum, multiple new liver and lung lesions and right portal vein thrombosis. She was stabilised and transferred to the gynecology-oncology unit for emergency systemic chemotherapy. Her future clinical course was complicated by intraabdominal and intracranial bleeds. Aggressive interventions including multiple endoscopies and CT angioembolization, two exploratory laparotomies including jejunal segmental resection and craniotomy for clot evacuation could not save her.
Ethics Committee approval was not required as the case report included only one case, without any patient identifiers. Informed consent was obtained from the patient.
Choriocarcinoma is gestational trophoblastic neoplasia (GTN) following either a hydatidiform mole or a non-molar pregnancy. It is the most aggressive form of GTN and is associated with a high mortality rate.1 Risk factors include previous molar pregnancy, maternal age more than 40 years and Asian/African descent.1 The incidence of GTN is 5–15% for hydatidiform mole and 5 to 200 per 100,000 normal non-molar pregnancies.2 Choriocarcinoma is associated with early vascular invasion and widespread metastases. Choriocarcinoma frequently metastasizes to the lungs, vagina, central nervous system, liver, kidney, gastrointestinal tract and spleen. The vascular nature of metastatic lesions is due to the angiogenesis stimulated by localised high levels of hCG.3 GTN should be suspected in patients with a larger than gestational age uterus size and hCG level >100,000 mIU/ml. Once GTN is suspected, a staging CT scan should be performed to look for metastatic lesions. A uterine curettage can be performed for histology. Biopsy of metastatic lesions is associated with a risk of bleeding and is not advised. Chemotherapy is the mainstay of treatment with cure rates in excess of 90%.2 The FIGO (The International Federation of Gynecology and Obstetrics): WHO (World Health Organisation) classification is a combination of staging and risk score assigned to predict the potential for developing chemoresistance. According to this classification, our patient would have had a Stage IV:13 choriocarcinoma, predicting a high risk for chemoresistance and mortality.
The spleen is an infrequent site of secondary visceral metastases and an uncommon site of metastatic choriocarcinoma. Spontaneous rupture of splenic metastases with hemoperitoneum is rare and there are only five case reports.12456 Table 1 provides a summary of all five case reports. All patients presented with abdominal pain, and only one patient had per vaginal bleeding.5 Four patients achieved remission after chemotherapy. One patient died due to progression of the disease,6 as he could not tolerate chemotherapy due to his poor physical condition. This patient was similar to our patient as she also was unable to tolerate chemotherapy due to her poor clinical condition after recurrent intra-abdominal and intracranial bleeding, thus illustrating the poor prognosis for such patients who cannot be stabilised adequately for initiating chemotherapy. In general, splenic rupture commonly occurs due to blunt splenic injury and non-operative management is widely established as a therapeutic choice. In patients with splenic rupture due to metastatic lesions, splenectomy not only cures the patient, but it also reduces future risk of rupture and establishes the histological diagnosis. Galazi et al.2 reported successful trans-catheter embolization for bleeding splenic metastasis from choriocarcinoma in a patient undergoing chemotherapy but the patient experienced persistent intraperitoneal hemorrhage. In patients with spontaneous splenic rupture with hemoperitoneum in a background of metastatic disease, splenectomy is undisputed.7 In a stable patient, if expertise is available, minimal access surgery can potentially improve short term outcomes.8 As we had expertise available910 for laparoscopic elective and acute care surgery, we performed a laparoscopic splenectomy successfully in this patient.
Choriocarcinoma with splenic metastases presenting with hemoperitoneum and haemorrhagic shock is rare. Spontaneous splenic rupture secondary to metastatic disease is a rare surgical oncologic emergency and splenectomy is indicated. This is the first reported case of successful management with emergency laparoscopic splenectomy for metastatic choriocarcinoma.
Figures and Tables
ACKNOWLEDGEMENTS
We would like to thank Dr Chuah Khoon Leong from the Department of Pathology (Tan Tock Seng Hospital, Singapore) for his contribution of the pathology slide and report for this case.
References
1. Yürüyen M, Yildiz O, Papila C, Tuzuner N. Gestational choriocarcinoma diagnosed with spontaneous splenic rupture after pregnancy induced by in vitro fertilization: a case report. Cases J. 2009; 2:7518.

2. Galazi M, Tait P, Seckl M, Savage P. Successful embolization of a life threatening bleeding splenic metastasis in a patient with gestational choriocarcinoma. Clin Obstet Gynecol Reprod Med. 2015; 1:16–18.
3. Lam KY, Tang V. Metastatic tumors to the spleen: a 25-year clinicopathologic study. Arch Pathol Lab Med. 2000; 124:526–530.
4. Challis DE, Rew KJ, Steigrad SJ. Choriocarcinoma complicated by splenic rupture: an unusual presentation. J Obstet Gynaecol Res. 1996; 22:395–400.

5. Nethra S, Hawe J, Elder J. Splenic rupture: a rare presentation of metastatic choriocarcinoma. Gynecol Surg. 2011; 8:435–437.

6. Ghinescu C, Sallami Z, Jackson D. Choriocarcinoma of the spleen--a rare cause of atraumatic rupture. Ann R Coll Surg Engl. 2008; 90:W12–W14.
7. Shelat VG, Tan EK, Teo LT, Vijayan A, Chiu MT. Outcomes of non-operative management of blunt splenic injury - An Asian experience. Int Surg. 2015; 100:1281–1286.
8. Musallam KM, Khalife M, Sfeir PM, Faraj W, Safadi B, Abi Saad GS, et al. Postoperative outcomes after laparoscopic splenectomy compared with open splenectomy. Ann Surg. 2013; 257:1116–1123.

9. Shelat VG, Chan CY, Liau KH, Ho CK. Laparoscopic exploration can salvage failed endoscopic bile duct stone extraction. Singapore Med J. 2012; 53:313–317.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download