Abstract
Backgrounds/Aims
A residual gallbladder (RGB) following a partial/subtotal cholecystectomy may cause symptoms that require its removal. We present our large study regarding the problem of a RGB over a 15 year period.
Methods
This study involved a retrospective analysis of patients managed for symptomatic RGB from January 2000 to December 2015.
Results
A RGB was observed in 93 patients, who had a median age of 45 (25–70) years, and were comprised of 69 (74.2%) females. The most common presentation was recurrence pain (n=64, 68.8%). Associated choledocholithiasis was present in 23 patients (24.7%). An ultrasonography (USG) failed to diagnose RGB calculi in 10 (11%) patients; whereas, magnetic resonance cholangio-pancreatography (MRCP) accurately diagnosed RGB calculi in all the cases except for 2 (4%) and, additionally, detected common bile duct (CBD) stones in 12 patients. Completion cholecystectomy was performed in all patients (open 45 [48.4%]; laparoscopic 48 [51.6%] and 19 [20.4%] patients required a conversion to open). The RGB pathology included stones in 90 (96.8%), Mirizzi's syndrome in 10 (10.8%) and an internal fistula in 9 (9.7%) patients. Additional procedures included CBD exploration (n=6); Choledocho-duodenostomy (n=4) and Roux-en-Y hepatico-jejunostomy (n=3). The mortality and morbidity were nil and 11% (all wound infection), respectively. Two patients developed incisional hernia during follow up. The mean follow up duration was 23.1 months (3–108) in 65 patients and the outcome was excellent and good in 97% of the patients.
Conclusions
Post-cholecystectomy recurrent biliary colic should raise suspicion of RGB. MRCP is a useful investigation for the diagnosis and assessment of any associated problems and provides a roadmap for surgery. Laparoscopic completion cholecystectomy is feasible, but is technically difficult and has a high conversion rate.
Residual gallbladder (RGB) refers to the remnant part of the gallbladder left behind during partial cholecystectomy in certain situations. It may be done intentionally to prevent injury to important structures in the presence of severe inflammation or portal hypertension, where it is difficult and dangerous to perform a complete cholecystectomy.123 Other times, the RGB may have been left behind unintentionally because of the inaccurate identification of the anatomy, usually in the presence of inflammation and fibrosis.4 In some patients, the RGB may continue to harbor or later develop a pathology like a stone, inflammation or fistula with adjacent structures and give rise to symptoms that require treatment.56789 Presently, there are a few small case studies and case reports in the literature pertaining to the problem of RGB.21011121314 In this retrospective study, we present our substantial experience with the problem of RGB managed over a period of 15 years in a tertiary care hospital in northern India.
A retrospective analysis was conducted from a prospective database of patients managed for symptomatic RGB from January 2000 to December 2015 at the Department of Surgical Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, which is a tertiary care institution in north India. Data was collected and analyzed for the demographics, investigations, and details of the initial and later surgery.
The remnant gallbladder was termed as RGB and the surgical removal of RGB was termed as completion cholecystectomy.
Follow up data was obtained from outpatient follow up cards, postal and telephonic communication. Data was analyzed using the Statistical Package for the Social Sciences (SPSS) software (version 21.0).
There were 93 patients who underwent surgery for RGB. The median age was 45 (25–70) years and 69 (74.2%) patients were females. All patients underwent the initial cholecystectomy at another hospital except for one. The initial cholecystectomy was by an open approach in 72 (77.4%) patients and by laparoscopic approach in the remaining 21 (22.6%) patients, of which 10 were laparoscopy converted to open (10.6%) cholecystectomy.
The reasons for incomplete cholecystectomy were available for 27 patients (29%). These included frozen Calot's triangle anatomy (14, 15.1%), acute cholecystitis (3, 3.2%), empyema (3, 3.2%), dense adhesions (3, 3.2%), intrahepatic gallbladder (2, 2.2%), iatrogenic duodenal injury (2, 2.2%) and unclear anatomy (1, 1.1%). In the remainder of the patients (n=66; 71%), the indications for incomplete gallbladder removal were not clear from the available records. Intraoperative cholangiogram was not performed in any of these patients.
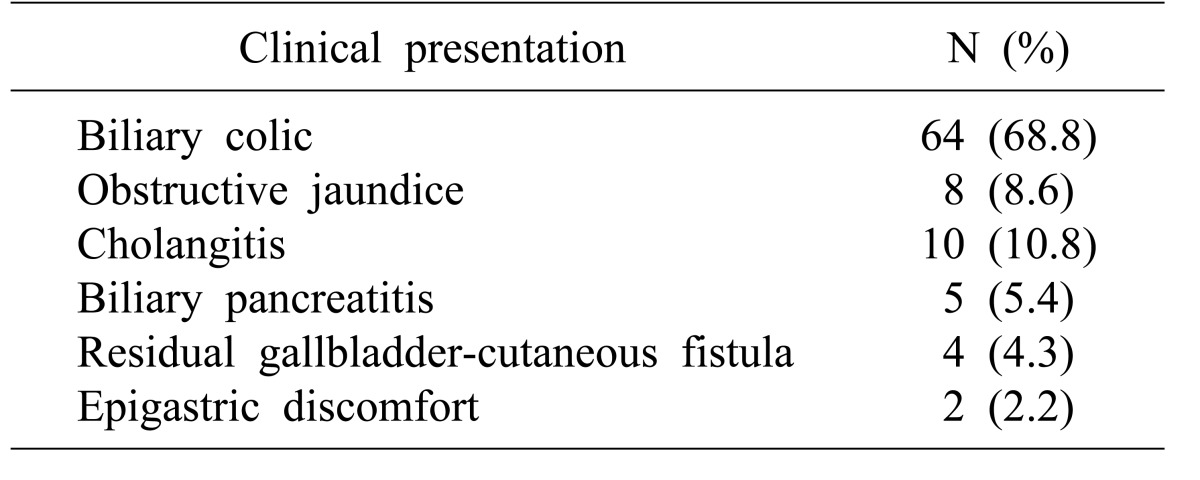
The median time to development of symptoms after the initial subtotal cholecystectomy was 36 months (1 to 252 months). The recurrence of pain, that is reminiscent of biliary colic before the initial cholecystectomy, was the most common presentation in 64 (68.8%) patients. Other presenting symptoms were jaundice with/without cholangitis, acute pancreatitis, cholecysto-cutaneous fistula, and epigastric discomfort (Table 1). The serum bilirubin level increased in 7 (7.5%) patients and alkaline phosphatase increased in 19 (20.4%).
Abdominal ultrasound examination (ultrasonography; USG) was useful to diagnose RGB in 91 patients (97.8%) and to accurately identify RGB calculi in 81 (89%). However, the USG failed to diagnose RGB calculi in 10 (11%) patients. Overall, common bile duct (CBD) stones were associated with RGB in 23 patients (24.7%). Of these, the USG displayed CBD stones in 13 patients and only CBD dilatation in 5 patients. The USG exhibited CBD dilatation in 5 other patients who later did not turn out to have CBD stones. In one patient, the USG misinterpreted stones in a RGB as CBD stones.
Magnetic resonance cholangio-pancreatography (MRCP) was performed in 50 (53.8%) patients and was performed routinely from the year 2008 onwards. The MRCP accurately diagnosed the RGB calculi in all of the cases except for 2 (4%), in whom it was diagnosed during a surgery for CBD stones after a failed endoscopic retrograde cholangiopancreatography (ERCP) clearance. In addition, the MRCP detected CBD stones in all 12 patients, where it was performed (Fig. 1).
Computed tomography (CT) scans were conducted in 15 patients; of these, 7 were performed for the suspicion of gallbladder cancer (none of them turned out to be carcinoma in histopathology), 3 for the evaluation of pancreatitis, 1 for the evaluation of the sinus tract, 1 for the evaluation of pain in the abdomen after USG which could not be RGB, and the reason was not clear in 3 patients. A pre-operative ERCP was done in 25 (26.9%) patients. At ERCP, CBD stones were found in 17 (68%) patients, of whom 10 (58.8%) underwent successful endoscopic clearance.
All 93 patients in the study underwent completion cholecystectomy in our department. The median time interval between initial cholecystectomy and completion cholecystectomy was 60 (3–288) months. Completion cholecystectomy was performed by an open method in 45 (48.4%) patients; whereas, laparoscopic completion cholecystectomy was attempted in 48 (51.6%) patients (conversion to open in 19 [20.4%]) (Fig. 2). The reasons for conversion were as follows: difficulty with identifying the anatomy of the Calot's triangle in 8 (42.1%), dense adhesions in 10 (52.6%) and suspicion of an RGB-duodenal fistula in 1 patient (5.2%). Out of 93 patients, stones in the residual gallbladder were present in 90 (96.8%). Mirizzi's syndrome was associated in 10 patients (10.8%); 9 were just compression and one patient had type 4 Mirizzi's syndrome (fistula with CBD). RGB had a fistulous communication with adjacent structures in 9 (9.7%) patients: duodenum, 4 (4.3%); abdominal wall, 4 (4.3%); and common bile duct, 1 (1%).
Additional biliary procedures were conducted in 13 (14%) patients: CBD exploration, (n=6), CBD exploration with choledocho-duodenostomy, (n=4), and Roux-en-Y hepatico-jejunostomy, (n=3). Two patients had intra-operative complications, namely a duodenal serosal injury and a hepatic sinusoidal bleed, which were addressed during surgery.
At pathology, the median size of the RGB was 3 cm (range: 1–7). Histopathological examinations of the resected RGBs revealed xanthogranulomatous cholecystitis in 9 (9.6%), acute on chronic cholecystitis in 2 (2.2%), follicular cholecystitis in 1 (1%), and the remaining patients had features of chronic cholecystitis.
There was no mortality and the postoperative morbidity was 11% (n=10): all patients had a wound infection and 2 patients among them developed incisional hernia during follow up. Follow up was available for 65 patients (70%), with an average duration of 23.1 months (from 3–108 months). Of these, 56 patients (86.15%) had complete symptom resolution (excellent outcome), and 8 (12.3%) had minimal symptoms with occasional dyspepsia and upper abdominal discomfort after surgery (good outcome). One patient had persistent pain that, on further evaluation, was found to have a right renal pelvis stone, and had symptom relief after a session of percutaneous nephrolithotomy. Thus, 64 out of the 65 (97%) patients with available follow up data had excellent or good outcome after surgery.
In this study, we described the presentation, evaluation and surgical management of 93 patients with symptomatic RGB at our center with good to excellent outcomes in 97% of the patients after completion cholecystectomy. To the best of our knowledge, this study is the largest investigation of the management of such cases published to date (Table 2).
Following an incomplete gallbladder removal, the remnant, which may comprise of a cystic duct with variable amounts of gallbladder, has been addressed by several names including cystic duct stump, gallbladder stump, gallbladder remnant or residual gallbladder.215161718 As it is difficult to differentiate a grossly dilated cystic duct stump from a true gallbladder remnant on the basis of imaging or even histological findings,1219 we believe that the term, residual gallbladder, appropriately describes the remnant of the gallbladder.
Incomplete removal of the gallbladder, also known as subtotal cholecystectomy, may be done intentionally in situations of severe inflammation, unclear anatomy or risk of hemorrhage as in portal hypertension. A subtotal cholecystectomy is required in about 3 to 8% of patients undergoing surgery for gallstone disease202122 and has proven to be a safe and effective option in such patients with gall stone disease to avoid iatrogenic complications.20 In the current study, we observed that among the RGBs, 29% were intentional subtotal cholecystectomy. In the remaining 71% patients, where the initial operating surgeon did not document an incomplete gallbladder removal, we assumed that the RGB was left behind unintentionally. RGB may be left behind unintentionally if the cystic duct - gallbladder junction is not identified correctly.423 The incidence of unintentional incomplete removal of the gallbladder is unknown. Though some authors have suggested that it may be higher following a laparoscopic cholecystectomy,415171823 but in our experience, 77.4% of the patients had index surgery via an open technique, and additionally, 10 patients (10.8%) had RGB after laparoscopy converted to open cholecystectomy. This outcome is similar to that reported by the small case studies by Tantia et al. (6 out of 7) and Rozsos et al. (5 out of 8).1213
The incidence of stones in RGB varies widely (0%–13%).112024 The incidence can be quite low if the remnant is opened, all of the stones and debris are meticulously removed, and the mucosa of the remaining gall bladder is cauterized.1120 The true incidence of symptomatic RGB after subtotal cholecystectomy is unknown, usually because the initial surgery was performed elsewhere.1012
The diagnosis of RGB remains difficult and an unaware clinician may fail to diagnose the condition and may subject the patient to a battery of unnecessary investigations. The most common presentation of patients with RGB is recurrent typical biliary colic that is reminiscent of the pain before the initial cholecystectomy (Table 2).2101112 Therefore, a history of recurrent biliary colic similar to the pain for which the initial cholecystectomy was performed should raise the suspicion of RGB.10 The operative records of the initial cholecystectomy should be reviewed to ascertain whether the entire gallbladder was removed. However, as demonstrated by this study, an absence of documentation of incomplete gallbladder removal at the initial surgery does not rule out the possibility of RGB. The liver function tests are usually normal; any derangement points towards a pathology co-existing with RGB, like CBD stones or pancreatitis. The diagnosis can be made with the help of an USG, MRCP, CT and ERCP.25 At our institution presently, USG is the initial investigation if RGB is suspected and can diagnose stones in the RGB as well. However, the USG may miss stones in the RGB in some patients (11% in this study) and CBD stones in others (18% in this study). In addition, RGB is often associated with other pathologies like Mirizzi syndrome, internal fistula, etc., that may be missed by an USG. In this study, the MRCP detected associated pathology like CBD stones (24.7%), Mirizzi's syndrome (10.8%) and internal biliary fistula (9.7%). MRCP was the investigation of choice for the diagnosis of RGB and to demonstrate biliary anatomy and any associated pathology. Most studies on RGB have not provided information on these aspects. Palanivelu et al also found MRCP to be better than USG (accuracy - 92% and 60% respectively) in diagnosing cystic duct remnant calculi.2 MRCP is now routine at our institution after USG in cases wherein RGB is suspected.
The treatment of symptomatic RGB is completion cholecystectomy of the remnant gallbladder. Although there are a few case reports of management of RGB stones with ERCP/extracorporeal shockwave lithotripsy,1026272829 we believe that it does not treat the cause of the pathology, i.e., the RGB. The surgical removal of a RGB can be technically demanding since these patients usually have a history of difficult gallbladder pathology that is further compounded by adhesions due to the initial surgery. Rozsos et al considered laparoscopic surgery to be risky and demonstrated the feasibility of completion cholecystectomy by microlaparotomy incisions.1330 Recently, some studies from institutions with advanced laparoscopic experience have reported successful laparoscopic removal of a RGB.21112 We performed completion cholecystectomy by both laparoscopic and open techniques. The laparoscopic approach was feasible (completion in 31.2%), but was associated with a higher conversion rate of nearly 40%, due to a difficult cholecystectomy. In the literature, there are a few case reports and small studies that primarily demonstrated successful laparoscopic completion cholecystectomy, with 0% conversion rates.211121415 In experienced surgical units, completion cholecystectomy can be safely performed with low morbidity and mortality. We found preoperative MRCP to be good road map to a safe completion cholecystectomy and recommend it in all patients with a suspected RGB. Interestingly, the histopathological examination of a resected RGB revealed a high incidence (9.6%) of xanthogranulomatous inflammation.
Ninety-eight percent (n=64) of the 65 patients that had available data for follow up (70%) reported complete resolution of symptoms after completion cholecystectomy at an average duration of follow-up of 23.1 months. Other studies in the literature have similarly reported excellent results after completion cholecystectomy.21011121314
In conclusion, after a cholecystectomy, a clinical history of recurrent biliary colic that is reminiscent of the pain for which the initial cholecystectomy was performed should strongly raise the suspicion of an RGB. MRCP is a useful investigation for establishing the diagnosis, diagnosing any associated problems, and providing a roadmap for further surgery. Completion cholecystectomy for symptomatic RGB can be performed safely at specialist centers with low morbidity rates and excellent relief of symptoms. Laparoscopic completion cholecystectomy is feasible, but is technically difficult and associated with a high conversion rate.
References
1. Philips JA, Lawes DA, Cook AJ, Arulampalam TH, Zaborsky A, Menzies D, et al. The use of laparoscopic subtotal cholecystectomy for complicated cholelithiasis. Surg Endosc. 2008; 22:1697–1700. PMID: 18071804.

2. Palanivelu C, Rangarajan M, Jategaonkar PA, Madankumar MV, Anand NV. Laparoscopic management of remnant cystic duct calculi: a retrospective study. Ann R Coll Surg Engl. 2009; 91:25–29. PMID: 18990269.

3. Michalowski K, Bornman PC, Krige JE, Gallagher PJ, Terblanche J. Laparoscopic subtotal cholecystectomy in patients with complicated acute cholecystitis or fibrosis. Br J Surg. 1998; 85:904–906. PMID: 9692560.

4. Walsh RM, Chung RS, Grundfest-Broniatowski S. Incomplete excision of the gallbladder during laparoscopic cholecystectomy. Surg Endosc. 1995; 9:67–70. PMID: 7725219.

5. Womack NA, Crider RL. The persistence of symptoms following cholecystectomy. Ann Surg. 1947; 126:31–55. PMID: 17858976.

6. Lum YW, House MG, Hayanga AJ, Schweitzer M. Postcholecystectomy syndrome in the laparoscopic era. J Laparoendosc Adv Surg Tech A. 2006; 16:482–485. PMID: 17004873.

7. Chow M, von Waldenfels A, Pace R. An unusual case of a retained stone following laparoscopic cholecystectomy. J Laparoendosc Surg. 1993; 3:513–518. PMID: 8251670.

8. Woods MS, Farha GJ, Street DE. Cystic duct remnant fistulization to the gastrointestinal tract. Surgery. 1992; 111:101–104. PMID: 1728064.
9. Satorras AM, Villanueva L, Vázquez J, Pigni L, Salem AM, Ramos A. Acute cholecystitis secondary to recurrent cholelithiasis after subtotal cholecystectomy. Cir Esp. 2005; 77:51–53. PMID: 16420885.
10. Walsh RM, Ponsky JL, Dumot J. Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surg Endosc. 2002; 16:981–984. PMID: 12163968.

11. Chowbey PK, Bandyopadhyay SK, Sharma A, Khullar R, Soni V, Baijal M. Laparoscopic reintervention for residual gallstone disease. Surg Laparosc Endosc Percutan Tech. 2003; 13:31–35. PMID: 12598755.

12. Tantia O, Jain M, Khanna S, Sen B. Post cholecystectomy syndrome: Role of cystic duct stump and re-intervention by laparoscopic surgery. J Minim Access Surg. 2008; 4:71–75. PMID: 19547688.

13. Rozsos I, Magyaródi Z, Orbán P. Cystic duct syndrome and minimally invasive surgery. Orv Hetil. 1997; 138:2397–2401. PMID: 9380377.
14. Chowbey P, Soni V, Sharma A, Khullar R, Baijal M. Residual gallstone disease - Laparoscopic management. Indian J Surg. 2010; 72:220–225. PMID: 23133251.

15. Pernice LM, Andreoli F. Laparoscopic treatment of stone recurrence in a gallbladder remnant: report of an additional case and literature review. J Gastrointest Surg. 2009; 13:2084–2091. PMID: 19415394.

16. Rogy MA, Függer R, Herbst F, Schulz F. Reoperation after cholecystectomy. The role of the cystic duct stump. HPB Surg. 1991; 4:129–134. PMID: 1931779.
17. Daly TD, Martin CJ, Cox MR. Residual gallbladder and cystic duct stones after laparoscopic cholecystectomy. ANZ J Surg. 2002; 72:375–377. PMID: 12028103.

18. Rieger R, Wayand W. Gallbladder remnant after laparoscopic cholecystectomy. Surg Endosc. 1995; 9:844. PMID: 7482201.

19. Mergener K, Clavien PA, Branch MS, Baillie J. A stone in a grossly dilated cystic duct stump: a rare cause of postcholecystectomy pain. Am J Gastroenterol. 1999; 94:229–231. PMID: 9934761.

20. Ibrarullah MD, Kacker LK, Sikora SS, Saxena R, Kapoor VK, Kaushik SP. Partial cholecystectomy--safe and effective. HPB Surg. 1993; 7:61–65. PMID: 8260436.
21. Chowbey PK, Sharma A, Khullar R, Mann V, Baijal M, Vashistha A. Laparoscopic subtotal cholecystectomy: a review of 56 procedures. J Laparoendosc Adv Surg Tech A. 2000; 10:31–34. PMID: 10706300.

22. Ji W, Li LT, Li JS. Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat Dis Int. 2006; 5:584–589. PMID: 17085347.
23. Blackard WG Jr, Baron TH. Leaking gallbladder remnant with cholelithiasis complicating laparoscopic cholecystectomy. South Med J. 1995; 88:1166–1168. PMID: 7481995.

24. Beldi G, Glättli A. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Endosc. 2003; 17:1437–1439. PMID: 12799885.

25. Kim JY, Kim KW, Ahn CS, Hwang S, Lee YJ, Shin YM, et al. Spectrum of biliary and nonbiliary complications after laparoscopic cholecystectomy: radiologic findings. AJR Am J Roentgenol. 2008; 191:783–789. PMID: 18716110.

26. Wani NA, Khan NA, Shah AI, Khan AQ. Post-cholecystectomy Mirizzi's syndrome: magnetic resonance cholangiopancreatography demonstration. Saudi J Gastroenterol. 2010; 16:295–298. PMID: 20871198.

27. Shelton JH, Mallat DB. Endoscopic retrograde removal of gallbladder remnant calculus. Gastrointest Endosc. 2006; 64:272–273. PMID: 16860084.

28. Kodali VP, Petersen BT. Endoscopic therapy of postcholecystectomy Mirizzi syndrome. Gastrointest Endosc. 1996; 44:86–90. PMID: 8836726.

29. Benninger J, Rabenstein T, Farnbacher M, Keppler J, Hahn EG, Schneider HT. Extracorporeal shockwave lithotripsy of gallstones in cystic duct remnants and Mirizzi syndrome. Gastrointest Endosc. 2004; 60:454–459. PMID: 15332046.

30. Rozsos I, Magyaródi Z, Orbán P. The removal of cystic duct and gallbladder remnant by microlaparotomy. Acta Chir Hung. 1997; 36:297–298. PMID: 9408381.
Fig. 1
MRC reconstruction displays a residual gallbladder with a stone (marked with solid arrow), as well as choledocholithiasis (marked with hollow arrow).

Fig. 2
Intraoperative picture during laparoscopic completion cholecystectomy that displays residual gallbladder with a triangle of safety after Calot's triangle dissection.
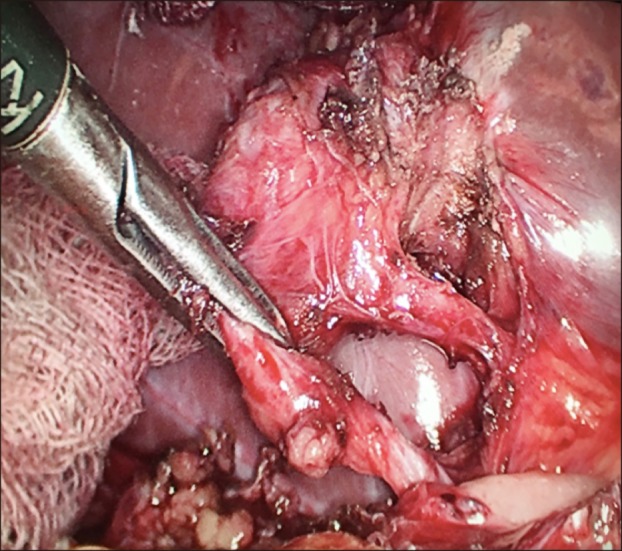
Table 2
Literature on the surgical management of the residual gallbladder
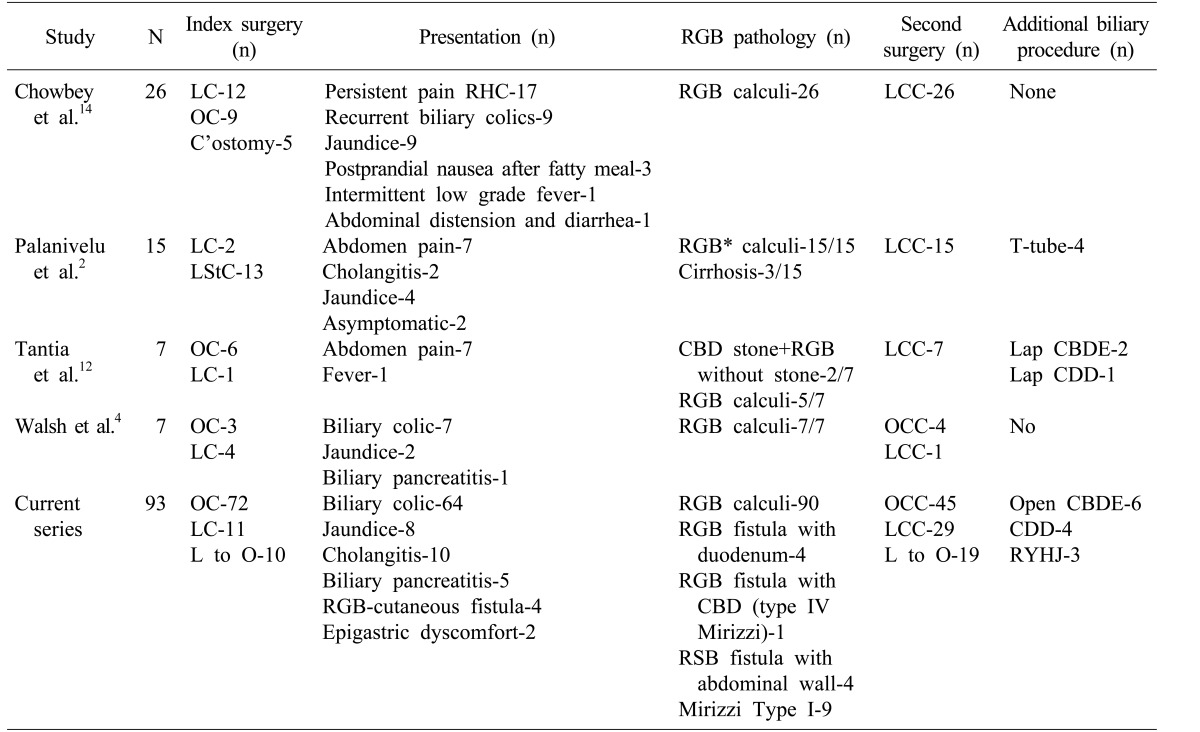
*The authors referred to RGBs as cystic duct stumps
LC, Laparoscopic cholecystectomy; OC, Open cholecystectomy; C'ostomy, Cholecystostomy; LStC, Laparoscopic subtotal cholecystectomy; LCC, Laparoscopic completion cholecystectomy; OCC, Open completion cholecystectomy; L to O, Laparoscopic converted to open; CBD, Common bile duct; CDD, Choledochoduodenostomy; RGB, Residual gallbladder; CBDE, Common bile duct exploration; RYHJ, Roux-en-Y Hepaticojejunostomy




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download