Abstract
Backgrounds/Aims
Liver Transplantation (LT) is a recognized treatment for Hepatocellular Carcinoma (HCC). The role of Bridging Therapies (BT) remains controversial.
Methods
From January 2001 to October 2012, 192 patients were referred to the National University Hospital, Singapore for consideration of LT for HCC. Sixty-five patients (33.8%) were found suitable for transplant and were placed on the waitlist. Analysis was performed in these patients.
Results
The most common etiology of HCC was Hepatitis B (n=28, 43.1%). Thirty-six patients (55.4%) received BT. Seventeen patients (47.2%) received TACE only, while 10 patients (27.8%) received radiofrequency ablation (RFA) only. The remaining patients received a combination of transarterial chemoembolization (TACE) and RFA. Baseline tumor and patient characteristics were comparable between the two groups. The overall dropout rate was 44.4% and 31.0% in the BT and non-BT groups, respectively (p=0.269). The dropout rate due to disease progression beyond criteria was 6.9% (n=2) in the non-bridged group and 22.2% (n=8) in the bridged group (p=0.089). Thirty-nine patients (60%) underwent LT, of which all patients who underwent Living Donor LT did not receive BT (n=4, 21.1%, p=0.030). The median time to LT was 180 days (range, 20–558 days) in the non-BT group and 291 days (range, 17–844 days) in the BT group (p=0.214). There was no difference in survival or recurrence between the BT and non-BT groups (p=0.862).
Liver Transplantation (LT) has become an established treatment for the management of Hepatocellular Carcinoma (HCC). Since Mazzaferro et al.1 reported their experience with the Milan Criteria in 1996, other centers have reported similar outcomes using this criteria. Yao et al.2 at the University of California, San Francisco (UCSF) in 2001 reported an overall survival of 75.2% with the new UCSF Criteria, extended from the Milan Criteria. Our center adopted the UCSF Criteria in 2007, and since then, it has seen a substantial increase in the demand for liver grafts in Singapore over the past 9 years. In 2006, Lim et al.3 reported median wait time for adult recipients of approximately 16.2 months. Since then, the demand for liver grafts has increased and so has the waiting time in a similar proportion. The management of HCC patients while on the waitlist remains controversial. Many centers employ interventional therapy called Bridging Therapy (BT) such as Trans-arterial Chemoembolization (TACE) and/or Radiofrequency Ablation (RFA) to prevent patients from progressing beyond criteria while they await an organ. This paper aims to study the role of BT in patients with HCC needing LT.
In Singapore, LT is one of the accepted modalities for the treatment of HCC, and since 2007, the UCSF Criteria for LT for HCC has been adopted for the purpose of organ allocation (prior to that, the Milan criteria was adopted). HCC is usually treated using a multimodality approach while the patient is on the waitlist. Common BT options include RFA and/or TACE. Other modalities such as Percutaneous Ethanol Injection (PEI) are used selectively if RFA cannot be performed based on the location of the tumor. In addition, Y-90 treatment can also be considered as BT wherever appropriate. Patients with HCC on the waitlist were carefully monitored with 3 monthly quadriphasic CT or MRI scans to assess tumor progression. The decision regarding BT was made at a weekly multidisciplinary tumor board and LT meeting, where surgeons, interventional radiologists, hepatologists, and oncologists are present. In patients who had received BT, pre and post intervention imaging was performed to assess the effect of BT on tumor burden. The effect of BT on tumor burden was classified according to the Response Evaluation Criteria In Solid Tumors (RECIST) Guidelines (Version 1.1).4 In patients who had received multiple BT, RECIST criteria were determined by comparing imaging performed at listing and that performed just prior to the transplant or at the time when they were removed from the waitlist. Patients with HCC who found a suitable living donor and were scheduled to undergo Living Donor Liver Transplantation (LDLT) can avoid BT if the date of transplantation was less than 6 weeks from the time of the most recent scan.
Patients with HCC needing LT who have a natural Modified End-stage Liver Disease (MELD) score of less than 15 are allocated a HCC MELD exception score of 15 points upon enlistment into the national waiting list. The tumor should be Stage II and above with no major vascular invasion or extrahepatic disease. However, unlike the MELD score allocation for HCC in USA (United Network for Organ Sharing, UNOS),5 the score of 15 points for HCC patients in Singapore is considered non-progressive, i.e., no additional points are given for waiting longer on the list.
All patients who were referred to our institution from January 2001 to October 2012 with the diagnosis of HCC for consideration for LT were reviewed. Patients who were not keen to undergo LT or those who were beyond Criteria (Milan Criteria prior to 2007 and UCSF Criteria from 2007 onwards) for LT were excluded from the study. Those who completed the LT workup and were found to be suitable for LT were included in the study. Transplanted patients were followed up for a minimum period of 3 years to assess long-term oncological outcomes.
Data collected included basic demographics, disease and tumor characteristics at various time points including at the time of listing and post-BT. Data on clinical outcomes such as BT-related complications, duration of stay post-transplant, and long term outcomes such as recurrence data and overall survival was also collected. Statistical analysis was performed using IBM SPSS software version 22 (SPSS, Chicago, IL, USA). Continuous data was expressed as median values (range) while categorical data was expressed as a number with percentages. A two-tailed p-value <0.05 was considered statistically significant.
This was a retrospective study performed at the National University Hospital, Singapore. The study did not require formal Domain Specific Review Board (DSRB) Review as it was classified as a Quality Improvement/Quality Assessment project (NHG DSRB Ref: 2013/00734).
A total of 192 consecutive patients were referred to the National University Center for Organ Transplantation with the diagnosis of HCC, needing LT, from January 2001 to October 2012. Those who were not keen to undergo LT after counselling (n=50) or those who were beyond criteria (n=37) were excluded. The remaining patients went on to complete the pre-LT work-up. Forty patients were found unsuitable for LT or did not complete the work-up. The remaining 65 patients were placed on the national waitlist for LT and were included in our study. Flowchart for referral and study inclusion is appended in Fig. 1. Baseline patient demographics and disease characteristics were comparable between the two groups and are detailed in Table 1. Given the multi-modality approach to the management of HCC, patients could be treated with RFA, TACE, PEI or a combination of these treatments prior to LT. Data regarding the various prelisting treatments received by patients are presented in Table 2.
In our cohort, 36 patients (55.4%) received BT while on the waitlist. Baseline patient and tumor characteristics were similar between the two groups as shown in Tables 1 and 2. There was a significantly larger group of patients in the BT group with compensated liver cirrhosis (n=26, 72.2%) compared to the non-BT group (n=10, 34.5%) (p=0.007). The majority of patients received a single BT (n=19, 52.8%). Out of the remaining 17 patients, 9 received BT twice (25.0%) and 5 patients underwent at least 4 interventions before LT (13.9%). In terms of the BT modality, 17 patients (47.2%) received TACE only, while 10 patients (27.8%) received RFA only. Nine patients (25%) received a combination of TACE and RFA. While there was no mortality following BT, 3 patients suffered morbidity from BT. One patient developed right-sided pneumothorax following RFA which did not require any intervention and resolved spontaneously and 2 patients developed groin hematomas post TACE. There were no cases of irreversible hepatic decompensation requiring urgent LT. In the cohort that received BT, eleven patients (30.6%) achieved a Completed Response (CR), 3 patients (8.3%) achieved a Partial Response (PR), 11 patients (30.6%) had Stable Disease (SD), and 11 patients (30.6%) had Progressive Disease (PD) in response to BT.
In the non-BT group, 65.5% of patients (19/29) eventually received LT compared to 55.6% of patients (20/36) in the BT group (p=0.415). These 39 patients (60%) successfully underwent LT at a median of 157 days (range, 17–844 days) from the time of listing. Of the 26 patients who were not transplanted, 10 patients (15.4%) had disease progression beyond criteria. Two of them did not receive BT while 8 patients received BT, although the difference was not statistically significant (p=0.089). The remaining 15 patients were removed from the waitlist for reasons mentioned in Table 3.
Among the patients who received LT, a significantly higher proportion of patients who underwent LDLT did not receive BT (n=4, 21.1%, p=0.030). None of the patients who received BT underwent LDLT. The median time from waitlist to LT was 180 days (range, 20–558 days) in the non-BT group and 291 days (range, 17–844 days) in the BT group (p=0.214).
In our cohort, the overall dropout rate at 6 months was 18.4%, while the dropout rate due to tumor progression beyond criteria was 6.2%. The percentage rose to 29.2% and 12.3%, respectively at 12 months. Subgroup analysis did not reveal any significant difference in dropout rates (both overall and tumor progression beyond criteria) between patients in the BT and non-BT groups. Results are presented in Table 4. The histopathology reports from the explanted liver showed that patients in the non-BT group had a greater burden of viable tumor with larger combined tumor size as well as a greater number of tumors, although statistical significance was only demonstrated in the latter. The median combined tumor size in the non-BT group was 40 mm (range, 3–105 mm) compared to 26 mm (range, 0–70 mm) (p=0.365), while the median number of tumors in the non-BT group was 2 (range, 1–6) as compared to 1 (range, 0–4) in the BT group (p=0.03). Two patients who achieved a CR to BT on pretransplant imaging scans had no evidence of tumour in explanted liver specimens. On assessing Alpha-fetoprotein (AFP) trends, 5 patients had a AFP slope of >15 ng/ml/month, of which 4 patients were in the BT group, and 1 patient was in the non-BT group (p=0.249).
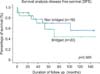
On comparing the BT and non-BT groups that successfully underwent LT, there was no difference in Overall Survival (OS) or Disease-Free Survival (DFS), as shown in Figs. 2 and 3 and Table 4. Five patients (12.8%) had recurrence of disease; 4 patients (11.4%) in the Deceased Donor LT (DDLT) group and 1 patient (25%) in the LDLT group. Recurrence occurred at a median of 32 months (range, 23–71 months) and 31 months in the DDLT and LDLT groups, respectively (p=0.999).
Among the patients who received BT, it was found that the proportion of patients who achieved a combined CR/PR response to BT was more than double in the multiple BT group (10/17, 58.8%) as compared to that in patients who received only a single BT intervention (4/19, 21.2%) (p=0.070). The multiplicity of the BT did not show a statistically significant effect on either success in bridging to transplant or the progression beyond criteria rate, as shown in Tables 3 and 5.
HCC is currently being treated with use of a multimodality approach. While LT for a selected group of patients has been proven to provide the best outcome, the role of BT in waitlisted patients with HCC remains controversial.678 The theoretical advantages of BT in patients with HCC on the waitlist are multifold. Firstly, proponents of BT believe that it will reduce dropout rates due to tumor progression beyond criteria.91011 Secondly, they also propose that by reducing tumor burden, it may improve post-transplant oncological results including lower tumor recurrence rates.121314 Lastly, BT can play a role in identifying candidates with poor tumor biology who might not be ideal candidates for LT.15161718
When LT began to be performed more widely as a definitive treatment for patients with HCC, there was also a concurrent increase in the number of patients with active HCC on the waitlist. A significant proportion of patients subsequently dropped out of the waitlist due to progression of tumor beyond criteria. In 1999, Llovet et al.19 reported a dropout rate of 23% within 6 months without BT for patients with HCC on the waitlist. Since then, Ashoori et al.20 reported dropout rates of 2.8% and 5.5% at 6 and 12 months, respectively with the use of RFA and TACE in a multi-modality approach. Both the Barcelona Group and Majno et al. found BT to have a clinical benefit after 6 months on the waitlist.2122 Variable dropout rates have been reported in the literature, but heterogeneous patient cohorts and varying BT protocols make it difficult to ascertain the definitive role of BT in reducing the dropout rates.2324 Within our cohort of 65 patients, the overall 6 month waitlist dropout rate was 18.4% and the 12 month dropout rate was 29.2%. These numbers are comparable with the recent experiences of other centers. While our study did not show a significant difference in the dropout rate between the BT and non-BT groups, the median time from listing to transplant was longer in patients who received BT. Hence, patients who received BT were able to stay on the waitlist for a longer period of time.
The initial results of LT for HCC were affected by high rates of tumour recurrence. Mazzaferro and colleagues showed that in patients with limited tumor burden, good long-term survival can be achieved. Therefore, it is clear that tumor burden at the time of LT has an impact on oncologic results. This has led transplant clinicians to suggest that BT could potentially reduce tumor burden and provide a survival advantage to patients with HCC needing LT. In 2003, Graziadei et al.24 reported a 5-year survival rate of 93% in patients treated with TACE or BT, with a recurrence rate of 2.4% in a cohort of 48 patients. He also did not report any cases of dropout due to tumor progression despite a mean wait time of 178 days. Two years later, a French multi-center case control study which included 200 patients, failed to show any difference in 5 year survival between patients who received TACE as BT and those who did not receive TACE as BT.25 In our series, both RFA and TACE were found to be safe and effective. Low morbidity rates and no mortality, coupled with high CR/PR rates in our cohort demonstrated effective reduction in tumor burden. Among all transplanted patients who received RFA, there were no cases of needle tract tumor or RFA site seeding on explant histology. In spite of this, our study did not demonstrate an effect on OS or DFS, even in patients who achieved ah CR on imaging. While the delta slope of AFP has been shown to be a good predictor of tumor-related drop out and recurrence post-transplant,1526 the small number of patients with an AFP slope >15 ng/ml/month in our cohort does not allow us to derive conclusions regarding its predictive value. However, it is worth noting that out of the 5 patients with a positive AFP slope, 4 patients received BT, a likely result of prescribing preferences in which a patient with a rising AFP is more likely to receive BT, as suggested by Sariano and colleagues.27
A international consensus conference held in 2010 could not make recommendations with respect to the use of BT in UNOS T1 tumors, or with respect to the use of one type of BT over another due to a lack of evidence.28 The group recommended that BT may be appropriate in patients with UNOS T2 tumors with an expected wait time of more than 6 months. In a clinical setting, with often unpredictable wait times, BT has been widely adopted. The current evidence shows that ablative techniques achieved higher rates of complete necrosis in lesions less than 3 cm, compared to TACE,1029 complete necrosis being a strong marker for long term survival. Agopian showed in 501 consecutive patients that a complete pathological response to BT strongly predicted long term tumor-free survival, with 5 year disease specific survival of 87%.30 Kornberg et al.31 obtained similar results in their study, leading Cescon and colleagues to recommend ablation for lesions <3 cm and TACE for larger tumors, in line with the Barcelona clinic liver cancer (BCLC) scoring system.32 In our cohort, only 2 patients had a complete pathological response to BT. Both of them were free of HCC at 3 years post-LT.
The selective use of BT in our study is the likely reason for the discrepancy between the BT and non-BT groups in terms of Child Pugh Classification. It is known that therapies such as TACE can result in hepatic decompensation and liver failure in a Child Pugh C liver cirrhosis patient. Garwood and colleagues33 reported a reversible and irreversible hepatotoxicity rate of 11% and 9%, respectively, in a cohort of 251 patients with HCC and concurrent synthetic hepatic dysfunction. Notably, 6 patients (2%) required urgent LT, and 11 patients (4%) passed away within 6 weeks of TACE. Other studies have also shown significant rates of post-TACE liver failure and 30 day mortality.3435 In our cohort, there were no cases of post-TACE liver failure necessitating urgent LT. We suggest that the decision regarding BT should be made after careful discussion with hepatologists, surgeons, and interventional radiologists to weigh the risks and benefits involved.
LDLT has become an acceptable alternative to DDLT for patients with HCC. Initial experiences suggested that compared to DDLT, patients who underwent LDLT had shorter wait times but an increased rate of recurrence.36 Both Lo et al. and Fisher et al. reproduced similar results, showing a significantly increased recurrence rate after LDLT in their studies.3738 In one of the largest studies to date, Kulik et al.,39 in a cohort of 229 patients, reported a hazard ratio of 2.35 for recurrence in LDLT patients compared to DDLT patients (p=0.0408). A proposed explanation for the results is that fast tracking results in an inability to assess a patient's tumor biology, resulting in successful LT even for patients with more aggressive HCCs.40 However, more recent papers have shown that recurrence rates are not increased after LDLT.41 The topic continues to cause controversy, with two meta-analysis, by Liang et al.42 in 2012 and Grant et al.43 in 2013 deriving conflicting conclusions. The low frequency of recurrence in our cohort makes analysis between DDLT and LDLT difficult. In the same study by Kulik mentioned above, despite having more advanced tumours in the LDLT cohort, patients were less likely to receive BT, and they received a reduced number of BT when rendered, leaving observers unable to assess the tumor response to BT.39 This has led to suggestions such as an “ablate and wait” strategy, or even a “bridge and wait” strategy to fully assess tumor biology prior to LT.44 Further studies are required to assess the role of BT in such a setting. In our cohort, none of our patients who underwent LDLT received BT. Despite the possible increased recurrence rates, the scarcity of deceased donor organs and the ever expanding waitlist necessitates the use of LDLT to augment the pool of donor organs. We suggest that all patients placed on the national waitlist should explore the option of LDLT.
In conclusion, BT remains controversial in the management of patients with HCC on the waitlist. Our study did not show any evidence regarding the use of BT to reduce dropout rates or improvement of oncological outcomes; however, we were able to maintain our group of patients on the waitlist for longer periods of time with selective use of BT. We advocate selective use of BT in patients who are at low risk for hepatic decompensation, in those who are at risk for progressing beyond criteria, and in those who will remain on the waitlist for a period of more than 6 months. Also, all patients who are listed should be counseled for possible LDLT.
Figures and Tables
Fig. 2
Comparison of Overall Survival (OS) after liver transplantation between BT and Non-BT groups.
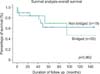
Fig. 3
Comparison of Disease Free Survival (DFS) after liver transplantation between BT and Non-BT groups.
References
1. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996; 334:693–699.

2. Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001; 33:1394–1403.

3. Lim SG, Wai CT, Da Costa M, Sutedja DS, Lee YM, Lee KH, et al. Referral patterns and waiting times for liver transplantation in Singapore. Singapore Med J. 2006; 47:599–603.
4. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247.

5. OPTN. Organ Procurement and Transplantation Network Policies. Richmond: OPTN;2016. cited 2016 Mar 26. Available from: https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf#nameddest=Policy_09.
6. Terzi E, Ray Kim W, Sanchez W, Charlton MR, Schmeltzer P, Gores GJ, et al. Impact of multiple transarterial chemoembolization treatments on hepatocellular carcinoma for patients awaiting liver transplantation. Liver Transpl. 2015; 21:248–257.

7. Lesurtel M, Müllhaupt B, Pestalozzi BC, Pfammatter T, Clavien PA. Transarterial chemoembolization as a bridge to liver transplantation for hepatocellular carcinoma: an evidence-based analysis. Am J Transplant. 2006; 6:2644–2650.

8. Fujiki M, Aucejo F, Choi M, Kim R. Neo-adjuvant therapy for hepatocellular carcinoma before liver transplantation: where do we stand? World J Gastroenterol. 2014; 20:5308–5319.

9. Alba E, Valls C, Dominguez J, Martinez L, Escalante E, Lladó L, et al. Transcatheter arterial chemoembolization in patients with hepatocellular carcinoma on the waiting list for orthotopic liver transplantation. AJR Am J Roentgenol. 2008; 190:1341–1348.

10. Mazzaferro V, Battiston C, Perrone S, Pulvirenti A, Regalia E, Romito R, et al. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg. 2004; 240:900–909.
11. Lu DS, Yu NC, Raman SS, Lassman C, Tong MJ, Britten C, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology. 2005; 41:1130–1137.

12. Tsochatzis E, Garcovich M, Marelli L, Papastergiou V, Fatourou E, Rodriguez-Peralvarez ML, et al. Transarterial embolization as neo-adjuvant therapy pretransplantation in patients with hepatocellular carcinoma. Liver Int. 2013; 33:944–949.

13. Freeman RB Jr, Steffick DE, Guidinger MK, Farmer DG, Berg CL, Merion RM. Liver and intestine transplantation in the United States, 1997-2006. Am J Transplant. 2008; 8:958–976.

14. Majno PE, Adam R, Bismuth H, Castaing D, Ariche A, Krissat J, et al. Influence of preoperative transarterial lipiodol chemoembolization on resection and transplantation for hepatocellular carcinoma in patients with cirrhosis. Ann Surg. 1997; 226:688–701. discussion 701-703.

15. Lai Q, Avolio AW, Graziadei I, Otto G, Rossi M, Tisone G, et al. Alpha-fetoprotein and modified response evaluation criteria in solid tumors progression after locoregional therapy as predictors of hepatocellular cancer recurrence and death after transplantation. Liver Transpl. 2013; 19:1108–1118.

16. Yao FY, Kerlan RK Jr, Hirose R, Davern TJ 3rd, Bass NM, Feng S, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology. 2008; 48:819–827.

17. De Carlis L, Di Sandro S, Giacomoni A, Slim A, Lauterio A, Mangoni I, et al. Beyond the Milan criteria: what risks for patients with hepatocellular carcinoma progression before liver transplantation? J Clin Gastroenterol. 2012; 46:78–86.
18. Otto G, Herber S, Heise M, Lohse AW, Mönch C, Bittinger F, et al. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 2006; 12:1260–1267.

19. Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology. 1999; 30:1434–1440.

20. Ashoori N, Bamberg F, Paprottka P, Rentsch M, Kolligs FT, Siegert S, et al. Multimodality treatment for early-stage hepatocellular carcinoma: a bridging therapy for liver transplantation. Digestion. 2012; 86:338–348.

21. Llovet JM, Mas X, Aponte JJ, Fuster J, Navasa M, Christensen E, et al. Cost effectiveness of adjuvant therapy for hepatocellular carcinoma during the waiting list for liver transplantation. Gut. 2002; 50:123–128.

22. Majno P, Lencioni R, Mornex F, Girard N, Poon RT, Cherqui D. Is the treatment of hepatocellular carcinoma on the waiting list necessary? Liver Transpl. 2011; 17:Suppl 2. S98–S108.

23. Yao FY, Bass NM, Nikolai B, Merriman R, Davern TJ, Kerlan R, et al. A follow-up analysis of the pattern and predictors of dropout from the waiting list for liver transplantation in patients with hepatocellular carcinoma: implications for the current organ allocation policy. Liver Transpl. 2003; 9:684–692.

24. Graziadei IW, Sandmueller H, Waldenberger P, Koenigsrainer A, Nachbaur K, Jaschke W, et al. Chemoembolization followed by liver transplantation for hepatocellular carcinoma impedes tumor progression while on the waiting list and leads to excellent outcome. Liver Transpl. 2003; 9:557–563.

25. Decaens T, Roudot-Thoraval F, Bresson-Hadni S, Meyer C, Gugenheim J, Durand F, et al. Impact of pretransplantation transarterial chemoembolization on survival and recurrence after liver transplantation for hepatocellular carcinoma. Liver Transpl. 2005; 11:767–775.

26. Han K, Tzimas GN, Barkun JS, Metrakos P, Tchervenkov JL, Hilzenrat N, et al. Preoperative alpha-fetoprotein slope is predictive of hepatocellular carcinoma recurrence after liver transplantation. Can J Gastroenterol. 2007; 21:39–45.

27. Soriano A, Varona A, Gianchandani R, Moneva ME, Arranz J, Gonzalez A, et al. Selection of patients with hepatocellular carcinoma for liver transplantation: Past and future. World J Hepatol. 2016; 8:58–68.

28. Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012; 13:e11–e22.

29. Lu DS, Yu NC, Raman SS, Limanond P, Lassman C, Murray K, et al. Radiofrequency ablation of hepatocellular carcinoma: treatment success as defined by histologic examination of the explanted liver. Radiology. 2005; 234:954–960.

30. Agopian VG, Morshedi MM, McWilliams J, Harlander-Locke MP, Markovic D, Zarrinpar A, et al. Complete pathologic response to pretransplant locoregional therapy for hepatocellular carcinoma defines cancer cure after liver transplantation: analysis of 501 consecutively treated patients. Ann Surg. 2015; 262:536–545. discussion 543-545.
31. Kornberg A, Witt U, Matevossian E, Küpper B, Assfalg V, Drzezga A, et al. Extended postinterventional tumor necrosis-implication for outcome in liver transplant patients with advanced HCC. PLoS One. 2013; 8:e53960.

32. Cescon M, Cucchetti A, Ravaioli M, Pinna AD. Hepatocellular carcinoma locoregional therapies for patients in the waiting list. Impact on transplantability and recurrence rate. J Hepatol. 2013; 58:609–618.

33. Garwood ER, Fidelman N, Hoch SE, Kerlan RK Jr, Yao FY. Morbidity and mortality following transarterial liver chemoembolization in patients with hepatocellular carcinoma and synthetic hepatic dysfunction. Liver Transpl. 2013; 19:164–173.

34. Hsin IF, Hsu CY, Huang HC, Huang YH, Lin HC, Lee RC, et al. Liver failure after transarterial chemoembolization for patients with hepatocellular carcinoma and ascites: incidence, risk factors, and prognostic prediction. J Clin Gastroenterol. 2011; 45:556–562.
35. Kothary N, Weintraub JL, Susman J, Rundback JH. Transarterial chemoembolization for primary hepatocellular carcinoma in patients at high risk. J Vasc Interv Radiol. 2007; 18:1517–1526. quiz 1527.

36. Park MS, Lee KW, Suh SW, You T, Choi Y, Kim H, et al. Living-donor liver transplantation associated with higher incidence of hepatocellular carcinoma recurrence than deceased-donor liver transplantation. Transplantation. 2014; 97:71–77.

37. Fisher RA, Kulik LM, Freise CE, Lok AS, Shearon TH, Brown RS Jr, et al. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant. 2007; 7:1601–1608.

38. Lo CM, Fan ST, Liu CL, Chan SC, Ng IO, Wong J. Living donor versus deceased donor liver transplantation for early irresectable hepatocellular carcinoma. Br J Surg. 2007; 94:78–86.

39. Kulik LM, Fisher RA, Rodrigo DR, Brown RS Jr, Freise CE, Shaked A, et al. Outcomes of living and deceased donor liver transplant recipients with hepatocellular carcinoma: results of the A2ALL cohort. Am J Transplant. 2012; 12:2997–3007.

40. Chan SC. Section 2. Small-for-size liver graft and hepatocellular carcinoma recurrence. Transplantation. 2014; 97:Suppl 8. S7–S10.

41. Ninomiya M, Shirabe K, Facciuto ME, Schwartz ME, Florman SS, Yoshizumi T, et al. Comparative study of living and deceased donor liver transplantation as a treatment for hepatocellular carcinoma. J Am Coll Surg. 2015; 220:297–304.e3.

42. Liang W, Wu L, Ling X, Schroder PM, Ju W, Wang D, et al. Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: a meta-analysis. Liver Transpl. 2012; 18:1226–1236.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download