Abstract
At pancreatic ductal adenocarcinoma is an aggressive malignancy with a high recurrence rate. Due to its high potentials of local invasion and distant metastasis, surgical resection is the only means for possible long-term survival. Surgical treatment comprises a distal pancreatectomy with or without splenectomy. Surgery has been conventionally contraindicated for patients with cirrhosis and portal vein hepato-biliary hypertension. Splenorenal shunt was first described by Warren and colleagues, to prevent death from bleeding esophageal varices in a patient with a patent portal vein hypertension. A 55-year-old Caucasian woman presented with an incidental pancreatic tumor. In our case, the shunt was necessary to complete the corrective oncological surgery for pancreatic ductal adenocarcinoma. The main difficulty was the presence of portal hypertension due to liver cirrhosis Child A; moreover, preservation of the spleen was mandatory in this patient. We successfully performed a distal pancreatectomy without splenectomy through the help of splenorenal shunt to preserve venous circulation.
Pancreatic ductal adenocarcinoma is an aggressive malignancy with a high recurrence rate. Pancreatic ductal adenocarcinoma is a rapidly progressing and late-diagnosed exocrine cancer. Due to its high potentials of local invasion and distant metastasis, surgical resection is the only means for achieving possible long-term survival.1 However, only 5% to 25% of the patients are eligible for resection, and even after R0 resection, median survival is only 12 and 20 months and the 5-year survival does not exceed 20%.23 In case of body and tail cancer, surgical treatment comprises a distal pancreatectomy with or without splenectomy.
In the past few decades, the incidence and prevalence of cirrhosis has been increasing worldwide, due to the increased incidence of alcoholic intake and non-alcohol related fatty liver disease. Traditionally, cirrhosis and portal vein hypertension have been considered a contraindication to major gastrointestinal surgery.4 Nevertheless, due to recent improvements in surgical techniques and perioperative support, some centers have reported cirrhosis as a non-absolute contraindication for pancreatic resection.5
Herein, we reported a case of a body tail pancreatic tumor in a cirrhotic patient.
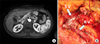
A 55 year-old Caucasian woman was admitted to our hospital due to an incidentaloma pancreatic tumor. The patient had a medical history of breast cancer two years prior and during a radiological follow-up examination, a pancreatic nodule was observed. Furthermore, hepatitis C virus-positivity was known since 1999. Interferon plus ribavirin treatment was administered for 12 weeks at time. Magnetic Resonance Imaging revealed a 4 cm-sized solid mass by the body tail of the pancreas, which was associated with dilation of the upstream Wirsung duct (Fig. 1A). Blood exams were normal excepted for a high CA 19-9 serum level (647 ng/ml). An ultrasonography-guided biopsy indicated an adenocarcinoma. A splenic vein invasion was suspected and based on the underlying hepatitis C virus infection, a portal vein pressure measurement was performed. Portal vein pressure was 22 mmhg and hepatic venous pressure gradient was 12 mmHg. On consulting a multidisciplinary board, a distal pancreatectomy without splenectomy was proposed. To perform an oncological resection considering the splenic vein invasion, a splenorenal shunt described by Warren et al.6 was performed (Fig. 1B). Pathology relieved a PDAC staged G3 (WHO) – UICC 2010: pT3 pN1. Surgery was complicated with a postoperative fluid collection that was treated conservatively. A computed tomography was performed and patency of the Warren shunt was observed (Fig. 2A and B).
We reported a successful distal pancreatectomy with splenorenal shunt in a cirrhotic patient. Pancreatic surgery is performed only in select cirrhotic patients. Nevertheless, an increasing number of case series show good results in select patients.457
A case-control study compared outcomes in 32 cirrhotic patients (30 Child A and Child B) vs. matched controls (non-cirrhotic) undergoing pancreatic resection surgery. The authors concluded that the cirrhotic group required more frequent reoperation (34% vs. 12%, p=0.039 and the rate of complications was higher than the non-cirrhotic group (47% vs. 22%; p=0.035).8
Splenorenal shunt was first described by Warren and colleagues,6 to prevent death from bleeding esophageal varices in a patient with a patent portal vein hypertension. In our case, preservation of the spleen was mandatory and the shunt was necessary to complete corrective oncological surgery for PDAC. The main difficulty was the presence of portal hypertension due to liver cirrhosis Child A. Previous studies indicated poorer outcomes in cirrhotic patients with portal hypertension.79 Transjugular intrahepatic portosystemic shunt before abdominal surgery does not improve postoperative evolution after abdominal surgery in cirrhotic patients.10
In summary, we successfully performed a distal pancreatectomy without splenectomy, through the help of a splenorenal shunt, to preserve venous circulation in a cirrhotic patient.
Figures and Tables
References
1. Zhan Q, Deng X, Weng Y, Jin J, Wu Z, Li H, et al. Outcomes of robotic surgery for pancreatic ductal adenocarcinoma. Chin J Cancer Res. 2015; 27:604–610.
2. Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007; 297:267–277.
3. Wysocka O, Kulbacka J, Saczko J. Adjuvant, neoadjuvant, and experimental regimens in overcoming pancreatic ductal adenocarcinoma. Prz Gastroenterol. 2016; 11:155–162.
4. Regimbeau JM, Rebibo L, Dokmak S, Boher JM, Sauvanet A, Chopin-Laly X, et al. The short- and long-term outcomes of pancreaticoduodenectomy for cancer in child A patients are acceptable: a patient-control study from the Surgical French Association report for pancreatic surgery. J Surg Oncol. 2015; 111:776–783.
5. Fuks D, Sabbagh C, Yzet T, Delcenserie R, Chatelain D, Regimbeau JM. Cirrhosis should not be considered as an absolute contraindication for pancreatoduodenectomy. Hepatogastroenterology. 2012; 59:881–883.
6. Warren WD, Zeppa R, Fomon JJ. Selective trans-splenic decompression of gastroesophageal varices by distal splenorenal shunt. Ann Surg. 1967; 166:437–455.
7. El Nakeeb A, Sultan AM, Salah T, El Hemaly M, Hamdy E, Salem A, et al. Impact of cirrhosis on surgical outcome after pancreaticoduodenectomy. World J Gastroenterol. 2013; 19:7129–7137.
8. Warnick P, Mai I, Klein F, Andreou A, Bahra M, Neuhaus P, et al. Safety of pancreatic surgery in patients with simultaneous liver cirrhosis: a single center experience. Pancreatology. 2011; 11:24–29.
9. Capussotti L, Ferrero A, Viganò L, Muratore A, Polastri R, Bouzari H. Portal hypertension: contraindication to liver surgery? World J Surg. 2006; 30:992–999.
10. Vinet E, Perreault P, Bouchard L, Bernard D, Wassef R, Richard C, et al. Transjugular intrahepatic portosystemic shunt before abdominal surgery in cirrhotic patients: a retrospective, comparative study. Can J Gastroenterol. 2006; 20:401–404.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download