Abstract
Backgrounds/Aims
Standard pancreatic resections are the current approach for patients with resectable, isolated pancreatic metastases of other neoplasms. However, the role of parenchyma-sparing pancreatectomies for such pathology is poorly investigated. The aim of the present study is to assess the oncological safety of central pancreatectomies for pancreatic metastases of other neoplasms.
Methods
A literature search was performed in order to identify patients with central pancreatectomies for pancreatic metastases of other neoplasms. The available data of the patients were extracted and analyzed.
Results
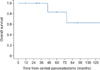
A total number of 16 patients were identified. Renal carcinoma was the primary origin for the largest number of these patients (11 patients - 69%). The mean overall survival time was 109 months, with 1-, 5- and 10-year survival rates of 100%, 84%, and 60%, respectively.
Conclusions
Although not often performed, a central pancreatectomy appears to be an oncologically safe surgical procedure in select patients with pancreatic metastases of other neoplasms of the pancreatic body and isthmus. However, no definitive conclusions should be drawn, based on the data provided in the present study, due to the limited number and heterogeneity of the patients.
A central pancreatectomy is a conservative surgical procedure that preserves the spleen and pancreatic parenchyma. It was proposed as alternative to distal/extended distal pancreatectomies.12 The advantage of a central pancreatectomy is better preservation of both endocrine and exocrine pancreatic function, compared with a distal pancreatectomy,2 an extended distal pancreatectomy,3 and a spleen-preserving distal pancreatectomy.4 The major drawbacks of a central pancreatectomy are high morbidity and non-nil mortality rates,156 particularly in aged and obese patients with diabetes.7 Pancreatic fistulae represent the main source of morbidity after a central pancreatectomy, being reported in up to 63% of the patients.1
The majority of the reported central pancreatectomies worldwide were performed for a benign/low-grade malignant tumor of the mid-portion of the pancreas.12 Thus, cystadenomas and pancreatic neuroendocrine tumors were the main indications for a central pancreatectomy.12 However, the role of a central pancreatectomy for pancreatic malignancies, such as pancreatic metastases of other neoplasms, is poorly investigated.
The aim of the present study is to assess the oncological safety of central pancreatectomies for pancreatic metastases of other neoplasms, based on data reported in the literature.
Patients were extracted from articles identified by electronic searching in PubMed-Medline and Google Scholar and by reviewing the references of the identified articles. The searched words were “central pancreatectomy”, “medial pancreatectomy”, “median pancreatectomy”, “meso-pancreatectomy”, “middle pancreatectomy”, “segmental resection of the pancreas”, “middle segmental resection of the pancreas”, “intermediate pancreatectomy”, and “isthmectomy”. No language restrictions were made. The available survival data of patients with a central pancreatectomy for metastases of other neoplasms were extracted. The study was approved by the Ethics Committee at our institution.
A total number of 16 patients with central pancreatectomies for pancreatic metastases of other neoplasms were identified worldwide,368910111213141516 as shown in Table 1. Renal carcinoma was the primary origin for the largest number of patients (11 patients - 69%). The mean overall survival time of the patients was 109 months, with 1-, 5- and 10-year survival rates of 100%, 84%, and 60%, respectively (Fig. 1).
Isolated pancreatic metastases of other neoplasms represent an uncommon pathology and accounts for 2%-5% of all pancreatic malignancies.1718 Thus, the reported series includes a relatively small number of patients;18192021 with most of the patients having had a renal carcinoma as the primary tumor,171821 as was the case in the present cohort of patients. Furthermore, pancreatic metastases of other neoplasms represent only 0.01%-1.8% of the indications for pancreatic resections.2223
Given the rarity of such pathology, an evidence-based surgical approach is not available. Standard pancreatic resections (i.e., pancreaticoduodenectomy, distal spleno-pancreatectomy, total pancreatectomy) are the common approaches for patients with a resectable disease.171821 However, it is not clear if pancreatic metastases of other neoplasms should share the same oncological principles as ductal adenocarcinoma of the pancreas. Negative resection margins can be achieved in some patients with central pancreatectomies for pancreatic metastases of other neoplasms but a standard lymph node dissection cannot be accomplished with this conservative surgical procedure.
The role of a systematic, loco-regional lymph node dissection for pancreatic metastases of other neoplasms remains controversial. Some studies did not find any survival differences between the standard pancreatic resections and atypical pancreatectomies for pancreatic metastases of other neoplasms and, thus, these studies do not support the routine use of systematic, loco-regional lymph node dissection.222425 However, there is a study showing that atypical pancreatic resections are associated with high recurrence rates.26 Nevertheless, there are also studies that identified metastatic lymph nodes in patients with standard pancreatectomies for isolated pancreatic metastases of other neoplasms in up to 35% of the cases.202227
After standard pancreatic resections for isolated pancreatic metastases of other neoplasms the reported median/mean survival time varied between 19 to 119 months, with 5-year survival rates between 36.2% and 88%.171819202123 These results are comparable with those reported in the present study. Consequently, a central pancreatectomy appears to have similar oncological outcomes to standard pancreatic resections.
Pancreatic metastases of other neoplasms are widely considered to be a part of a systemic oncological disease.18 These patients are likely to receive chemotherapy. Chemotherapy in a patient with diabetes can be challenging because some chemotherapeutic agents can lead to or exacerbate potential renal, cardiac or neuropathic complications complications.28 Thus, sparing the pancreatic parenchyma represents an important issue in these patients and has the potential to mitigate the complications of chemotherapy by reducing the risk of postoperative diabetes.2124 It is widely accepted that a central pancreatectomy, of all of the pancreatic resections, has the lowest potential of developing postoperative diabetes.12 Nevertheless, corticosteroids, that are often used to prevent chemotherapy-induced nausea and vomiting, may also induce diabetes in approximately 20% of the non-diabetic patients.2829
The results of this study should be regarded with caution because there are important limitations. The study includes a small number of patients, coming from many surgical centers, with different approaches and criteria selection, for a parenchyma-sparing surgical procedure. Furthermore, the group included patients with different primary tumors, and no data are available for the adjuvant/neoadjuvant treatments. It is worth mentioning that a recent multicenter study has shown no survival benefit of pancreatectomies for isolated metastases from renal carcinoma, compared with chemotherapy with tyrosine kinase inhibitors.30
In conclusion, although rarely performed, a central pancreatectomy appears to be an oncologically safe surgical procedure in select patients with pancreatic metastases of other neoplasms of the pancreatic body and isthmus. Sparing the pancreatic parenchyma represents an important issue in patients with such pathology because they are likely to receive chemotherapy. A conservative pancreatectomy has the potential to mitigate the complications of chemotherapy by reducing the risk of postoperative diabetes, which is the lowest after a central pancreatectomy, compared with standard pancreatic resections. However, no definitive conclusions should be drawn based on the data provided in the present study due to the limited number and heterogeneity of the patients.
Figures and Tables
ACKNOWLEDGEMENTS
An early version of the manuscript was presented at the 44th Congress of the Korean Association of HBP Surgery (April 1-2, 2016, Seoul, Korea). Traian Dumitrascu received a travel grant from the Korean Association of HBP Surgery.
References
1. Dumitrascu T, Popescu I. Central pancreatectomy revisited. J Transl Med Res. 2015; 20:185–194.
2. Iacono C, Verlato G, Ruzzenente A, Campagnaro T, Bacchelli C, Valdegamberi A, et al. Systematic review of central pancreatectomy and meta-analysis of central versus distal pancreatectomy. Br J Surg. 2013; 100:873–885.
3. Cataldegirmen G, Schneider CG, Bogoevski D, Koenig A, Kaifi JT, Bockhorn M, et al. Extended central pancreatic resection as an alternative for extended left or extended right resection for appropriate pancreatic neoplasms. Surgery. 2010; 147:331–338.
4. Dumitrascu T, Scarlat A, Ionescu M, Popescu I. Central pancreatectomy versus spleen-preserving distal pancreatectomy: a comparative analysis of early and late postoperative outcomes. Dig Surg. 2012; 29:400–407.
5. Dumitraşcu T, Barbu ST, Ionescu M, Popescu I. POSSUM, a potentially useful tool for prediction of morbidity in patients undergoing central pancreatectomy. Chirurgia (Bucur). 2012; 107:447–453.
6. Goudard Y, Gaujoux S, Dokmak S, Cros J, Couvelard A, Palazzo M, et al. Reappraisal of central pancreatectomy a 12-year single-center experience. JAMA Surg. 2014; 149:356–363.
7. Dumitrascu T, Barbu ST, Purnichescu-Purtan R, Ionescu M, Popescu I. Risk factors for surgical complications after central pancreatectomy. Hepatogastroenterology. 2012; 59:592–598.
8. Crippa S, Bassi C, Warshaw AL, Falconi M, Partelli S, Thayer SP, et al. Middle pancreatectomy: indications, short- and long-term operative outcomes. Ann Surg. 2007; 246:69–76.
9. de Clavière G, Paye F, Fteriche S, Terris B, Belghiti J, Sauvanet A. Medial pancreatectomy: results of a series of 11 patients. Ann Chir. 2002; 127:48–54.
10. Deguchi Y, Shimada K, Nara S, Esaki M, Sakamoto Y, Kosuge T, et al. Pancreaticojejunostomy with invagination of the punched pancreatic remnant after medial pancreatectomy and enucleation for multiple metastases of renal cell carcinoma: report of a case. Surg Today. 2009; 39:1086–1090.
11. Dumitrascu T, Scarlat A, Ciurea S, Popescu I. Central pancreatectomy for a pancreatic metastasis of colon cancer - a case report. J Transl Med Res. 2015; 20:153–156.
12. Dumitraşcu T, Dima S, Popescu C, Gheonea DI, Ciurea T, Saftoiu A, et al. An unusual indication for central pancreatectomy--late pancreatic metastasis of ocular malignant melanoma. Chirurgia (Bucur). 2008; 103:479–485.
13. Hirono S, Tani M, Kawai M, Ina S, Nishioka R, Miyazawa M, et al. A central pancreatectomy for benign or low-grade malignant neoplasms. J Gastrointest Surg. 2009; 13:1659–1665.
14. Müller MW, Friess H, Kleeff J, Hinz U, Wente MN, Paramythiotis D, et al. Middle segmental pancreatic resection: An option to treat benign pancreatic body lesions. Ann Surg. 2006; 244:909–918.
15. Sauvanet A, Partensky C, Sastre B, Gigot JF, Fagniez PL, Tuech JJ, et al. Medial pancreatectomy: a multi-institutional retrospective study of 53 patients by the French Pancreas Club. Surgery. 2002; 132:836–843.
16. Shikano T, Nakao A, Kodera Y, Yamada S, Fujii T, Sugimoto H, et al. Middle pancreatectomy: safety and long-term results. Surgery. 2010; 147:21–29.
17. Adler H, Redmond CE, Heneghan HM, Swan N, Maguire D, Traynor O, et al. Pancreatectomy for metastatic disease: a systematic review. Eur J Surg Oncol. 2014; 40:379–386.
18. Reddy S, Wolfgang CL. The role of surgery in the management of isolated metastases to the pancreas. Lancet Oncol. 2009; 10:287–293.
19. Crippa S, Angelini C, Mussi C, Bonardi C, Romano F, Sartori P, et al. Surgical treatment of metastatic tumors to the pancreas: a single center experience and review of the literature. World J Surg. 2006; 30:1536–1542.
20. Strobel O, Hackert T, Hartwig W, Bergmann F, Hinz U, Wente MN, et al. Survival data justifies resection for pancreatic metastases. Ann Surg Oncol. 2009; 16:3340–3349.
21. Untch BR, Allen PJ. Pancreatic metastasectomy: the Memorial Sloan-Kettering experience and a review of the literature. J Surg Oncol. 2014; 109:28–30.
22. Konstantinidis IT, Dursun A, Zheng H, Wargo JA, Thayer SP, Fernandez-del Castillo C, et al. Metastatic tumors in the pancreas in the modern era. J Am Coll Surg. 2010; 211:749–753.
23. Kwak JH, Heo JS, Park JY, Choi DW, Choi SH, Lee HS. Outcomes of pancreaticoduodenectomy in patients with metastatic cancer. Korean J Hepatobiliary Pancreat Surg. 2014; 18:147–151.
24. Yazbek T, Gayet B. The place of enucleation and enucleo-resection in the treatment of pancreatic metastasis of renal cell carcinoma. JOP. 2012; 13:433–438.
25. Zerbi A, Ortolano E, Balzano G, Borri A, Beneduce AA, Di Carlo V. Pancreatic metastasis from renal cell carcinoma: which patients benefit from surgical resection? Ann Surg Oncol. 2008; 15:1161–1168.
26. Bassi C, Butturini G, Falconi M, Sargenti M, Mantovani W, Pederzoli P. High recurrence rate after atypical resection for pancreatic metastases from renal cell carcinoma. Br J Surg. 2003; 90:555–559.
27. Reddy S, Edil BH, Cameron JL, Pawlik TM, Herman JM, Gilson MM, et al. Pancreatic resection of isolated metastases from non-pancreatic primary cancers. Ann Surg Oncol. 2008; 15:3199–3206.
28. Psarakis HM. Clinical challenges in caring for patients with diabetes and cancer. Diabetes Spectr. 2006; 19:157–162.
29. Jeong Y, Han HS, Lee HD, Yang J, Jeong J, Choi MK, et al. A Pilot Study evaluating steroid-induced diabetes after antiemetic dexamethasone therapy in chemotherapy-treated cancer patients. Cancer Res Treat. 2016; 48:1429–1437.
30. Santoni M, Conti A, Partelli S, Porta C, Sternberg CN, Procopio G, et al. Surgical resection does not improve survival in patients with renal metastases to the pancreas in the era of tyrosine kinase inhibitors. Ann Surg Oncol. 2015; 22:2094–2100.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download