Abstract
The Fibrolamellar variant of Hepatocellular Carcinoma (FLHCC) is a rare form of liver cancer that presents in the 3rd decade of life, is rarely associated with cirrhosis or chronic Hepatitis B/C virus infection, and usually presents with normal serum alpha-fetoprotein (AFP) levels. FLHCC presenting during pregnancy is extremely rare, with only 4 cases reported. We present a case of FLHCC in pregnancy and discuss the dilemmas in management. A 26 year-old primigravida, 26 weeks of gestation presented with a month's history of obstructive jaundice secondary. Investigations revealed a mass in the left lateral segment of the liver with extension down the left hepatic duct into the common bile duct. Following an emergency caesarean section at 31 weeks, she underwent a left hepatectomy with extrahepatic bile duct excision. The postoperative course was uneventful. Histopathology showed FLHCC. In conclusion, liver tumors presenting during pregnancy should be managed in a multidisciplinary setup with facilities for neonatal intensive care. Management depends on the presumed pathology, period of gestation and family preferences.
Go to : 
The fibrolamellar variant of Hepatocellular Carcinoma (FLHCC) accounts for 1% of all primary liver cancers.1 Unlike typical hepatocellular Carcinoma (HCC), FHLCC occurs predominantly in the 3rd decade of life, is not associated with chronic Hepatitis B/C virus infection, and 90% exhibit normal serum alpha-fetoprotein (AFP) levels.1 FLHCC presenting during pregnancy is extremely rare.2 We report a case of FLHCC presenting during the second trimester of pregnancy and review the relevant literature.
Go to : 
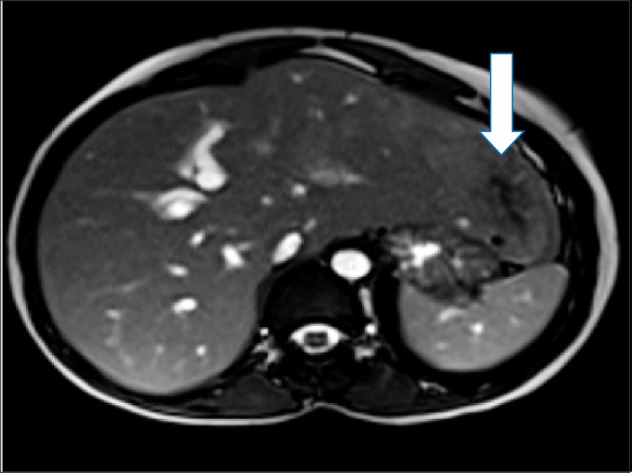
A 26 year-old primigravida, 26 weeks of gestation presented with a month long history suggestive of obstructive jaundice. There was no history of use of hormonal contraceptive pills. Liver Function Tests showed an obstructive picture, a negative viral serology, a serum AFP level of 195.8 IU/ml (normal <5.8 IU/ml), and a cancer antigen level (CA) of 19.9-64.8 U/ml (normal <34 U/ml). Magnetic Resonance Imaging (MRI) showed a 6.4 cm×4.4 cm irregular lesion in segments II and III of the liver with contiguous extension into the common bile duct (CBD) (Fig. 1). The tumor was hyperintense on T2- and hypointense on T1-weighted images.
With a presumptive diagnosis of HCC/hepatocholangiocarcinoma, options offered included continuation of pregnancy to 28 weeks and subsequent surgery or immediate termination of pregnancy with surgery. Due to financial constraints, the family made an informed decision to continue the pregnancy to 32 weeks. A right-sided percutaneous transhepatic biliary drainage (PTBD) was performed. She returned three weeks later with vaginal bleeding and abdominal pain. Investigations revealed anterior placenta previa. A viable baby was delivered by emergency cesarean section at 31 weeks.
A subsequent computed tomography (CT) scan confirmed the MRI findings but also suggested that the tumor might be extending up to the suprapancreatic margin of the CBD (Fig. 2). Intraoperatively, the tumor was found to be confined to segments II and III of the liver (Fig. 3). Palpation of the right hepatic duct (RHD) identified no tumor while the entire left hepatic duct (LHD) and CBD, up to the suprapancreatic portion, seemed to contain tumor. A cholangiogram performed through the right PTBD confirmed the findings. A standard left hepatectomy was performed. Upon transecting the RHD, Soft, pulp-like material was extruded from the LHD and CBD. The CBD was transected above the duodenum. The distal ends of the CBD and RHD were free of tumor on the frozen section margins. The extruded material showed cancer cells, suggestive of tumor thrombus. A Roux-en-Y ductojejunostomy was fashioned.
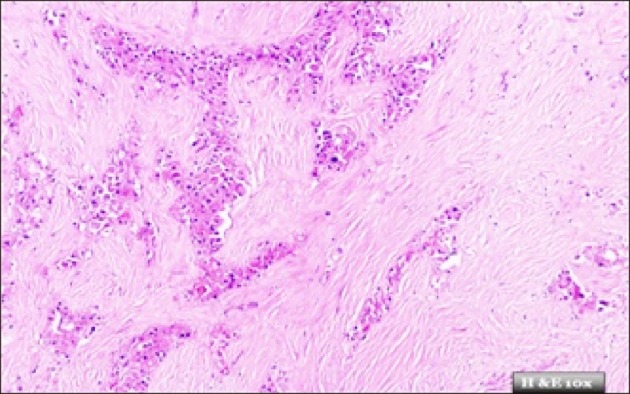
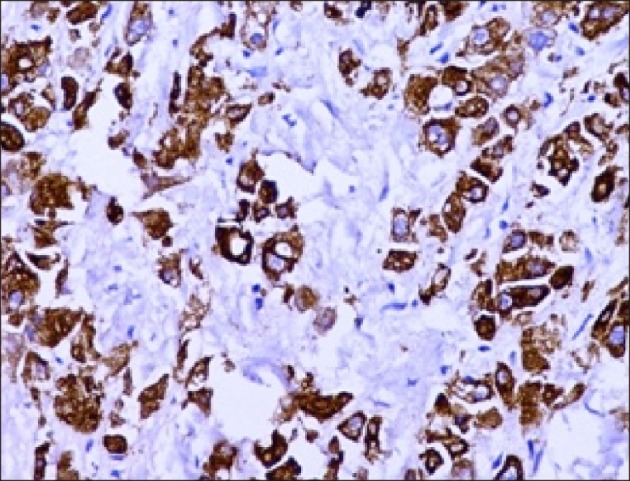
The resected specimen showed features consistent with FLHCC (Figs. 4 and 5). The resection margins were free of tumor. The postoperative course was uneventful and she was discharged after a week, along with her healthy baby. The patient is presently healthy, with no signs of recurrence at a nine-month follow up.
Go to : 
FLHCC occurs in younger patients during the second or third decade of life.1 Female gender predilection and association with oral contraceptive pills, although reported, has not been substantiated.1 Jaundice, as an initial presentation, is extremely rare. Patients usually present with vague abdominal pains. FLHCC presents as large, heterogeneous, lobulated lesions with calcification (40-68%) and central scarring (65-70%). Scarring of more than 2 cms in size with radiating fibrotic bands is characteristic. While CT arterial phase images show heterogeneous enhancement, venous and delayed phases show variable enhancement with 50% being isoattenuating and the rest hypo- or hyperattenuating.3 On MRIs, lesions generally appear as hypointense T1- and hyperintense T2-weighted images. Unlike focal nodular hyperplasia, where the central scar is hyperattenuating in T2-images, the central scar in FLHCC is hypointense in both T1 and T2 phases.3 Gadolinium contrast images mimic the CT findings, being hyperintense in the arterial phase and hypo- or isoattenuating in the venous phases.3 In our case, there was extension of the tumor into the segmental ducts, along with the LHD and CBD. There was also the presence of persistent enhancement on the delayed phase imaging suggesting cholangiocarcinoma/hepatocholangiocarcinoma.
The histopathological diagnosis of FLHCC is based on: the presence of large, polygonal cells with abundant eosinophilic cytoplasm; vesicular nuclei and large nucleoli; abundant, fibrous stroma arranged in thin, parallel lamellae around tumor cells; and tumor cells arranged in sheets or small trabeculae.2 The presence of HCC foci denotes a mixed variant with a poorer prognosis than the pure form. FLHCC stains positive with Hep-Par, Arginase-1, and CK-7 and is negative for chromogranin.2
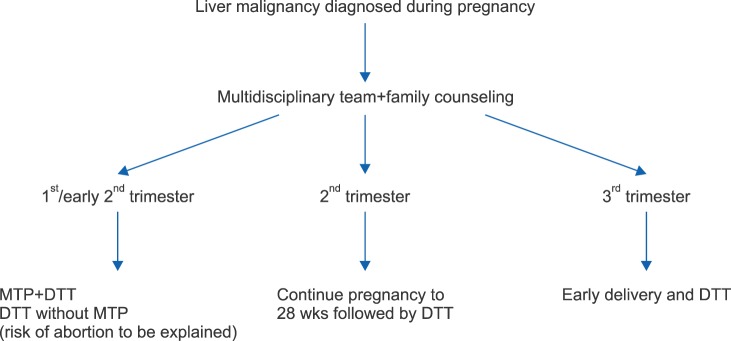
Management of liver malignancy during pregnancy depends on the nature of the disease, period of pregnancy, and family preferences. Lesions detected in the first trimester or early second trimester are best managed by immediate counseling, termination of pregnancy and definitive tumor therapy. However, immediate surgery without termination, with the risk of abortion, and adjuvant chemotherapy may be offered. For patients in the late second trimester, continuation to 28 weeks may be recommended, provided neonatal intensive care unit facilities are available and affordable. Pregnancies advanced to the third trimester are managed by early delivery and definitive tumor management. If liver resection is primarily indicated, this may be performed along with the caesarean section or subsequently (Fig. 6).
Complete surgical resection of the tumor with negative margins and hilar lymphadenectomy is the gold standard.124 Five-year survival rates of 30-75% with recurrence rates of 36-100% (10-33 months median survival) have been reported. Factors associated with poor outcome include: multiple tumors, regional lymph nodal positivity, positive margins, old age, presence of mixed FLCC/HCC variant, and macrovascular invasion.124 Local or distant recurrence should be considered for re-resection. Three year survival rates of 76% have been reported when performing liver transplantation for unresectable liver lesions.4 Although transplantation survival rates are significantly lower than the corresponding resection group, the option should be considered for good, prognostic tumors in the young.
The influence of pregnancy on tumor behavior in FLCC is unknown with conflicting reports.12 No deleterious, adverse effects have been observed in patients undergoing pregnancy following treatment of either FLHCC or non-FLHCC in the absence of recurrent disease.12 Liver masses presenting during pregnancy are usually benign. MRI is usually confirmatory and biopsy rarely essential. Patients with a history of resected liver malignancy, cirrhotics, or chronic Hepatitis B/C should have a liver ultrasound during the routine fetal screening to rule out recurrence.
Our case is unique in that FLHCC presented as obstructive jaundice during pregnancy. FLHCC should be considered as a differential diagnosis in non-cirrhotic, pregnant patients presenting with obstructive jaundice and a liver lesion. Treatment of liver tumors during pregnancy must be individualized based on the diagnosis a patient and family preferences.
Go to : 
References
1. El-Serag HB, Davila JA. Is fibrolamellar carcinoma different from hepatocellular carcinoma? A US population-based study. Hepatology. 2004; 39:798–803. PMID: 14999699.

2. Stipa F, Yoon SS, Liau KH, Fong Y, Jarnagin WR, D'Angelica M, et al. Outcome of patients with fibrolamellar hepatocellular carcinoma. Cancer. 2006; 106:1331–1338. PMID: 16475212.

3. Ganeshan D, Szklaruk J, Kundra V, Kaseb A, Rashid A, Elsayes KM. Imaging features of fibrolamellar hepatocellular carcinoma. AJR Am J Roentgenol. 2014; 202:544–552. PMID: 24555590.

4. El-Gazzaz G, Wong W, El-Hadary MK, Gunson BK, Mirza DF, Mayer AD, et al. Outcome of liver resection and transplantation for fibrolamellar hepatocellular carcinoma. Transpl Int. 2000; 13(Suppl 1):S406–S409. PMID: 11112043.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download