Abstract
Gastrointestinal tumors (GISTs) of the pancreas are extremely rare with limited individual case reports and small number of case series. Herein, we report a case of pancreatic extragastrointestinal stromal tumor (EGIST) along with literature review. A 64-year-old female patient was referred to us for treatment of an abdominal mass detected by ultrasonographic examination. The tumor was located in the periamullary region. Under a preoperative diagnosis of a duodenal GIST, we performed a pylorus preserving pancreatoduodenectomy for this lesion. Laboratory examination results were within normal ranges. On pathologic gross examination, the tumor measured at 7 cm in its greatest dimension almost entirely involved the pancreatic head. Its cut surface was rubbery and white. It was surrounded by a thin pseudocapsule and well demarcated. Histopathological examination of the specimen showed a cellular lesion with compressed pancreatic tissue at peripheral. Mitotic count was 5 per 50 high-power fields. Immunohistochemically, neoplastic cells were positive for antibodies against C-KIT (CD117), CD 34, and vimentin. However, smooth-muscle actin reactions with antibodies against S-100 or desmin were negative. Based on above findings, the tumor was finally diagnosed as GISTs originating from the pancreas. The patient has been followed up postoperatively for 72 months. There is no evidence of recurrence. Here we report this case of pancreatic EGIST presenting as a solid neoplasm along with literature review of cases previously described. Our review on pancreatic EGISTs is limited and insufficient to make a conclusion regarding its clinical features. Those manifested large masses tended to have an aggressive biological and clinical behavior. Thus, pancreatic EGISTs need to be carefully differentiated. Adequate surgical intervention is necessary for pancreatic EGISTs.
GISTs are the most common primary mesenchymal tumors originated from the gastrointestinal tract. These tumors occur mainly in the stomach (50–60%), small bowel (20-30%), large bowel (10%), and esophagus (5%).1 In rare cases, these tumors are found as primary tumors outside the GI tract, such as the omentum, mesentery, retroperitoneum, and gallbladder.23 These tumors have been designated as “extra-gastrointestinal stromal tumors” (EGISTs). EGISTs arising in the pancreas are extremely rare with limited individual case reports and small numbers of case series. Herein, we report a case of a pancreatic extra-gastrointestinal stromal tumor in a 64-year-old female patient along with a review of literature.
A 64-year-old woman was referred to our department for treatment of an abdominal mass incidentally detected by ultrasonographic examination during health screening in August 2010. She had no clinical symptom related to this tumor. She had no remarkable history. Physical examination revealed no specific findings. Laboratory data were within normal limits. Tumor markers were also within normal limits. Abdominal computed tomography (CT) showed a well enhanced mass measuring 6.5×6.5 cm with central low dense lesion (Fig. 1A and B). Endoscopic ultrasonography (EUS) revealed a well-defined homogenous hypoechoic mass like lesion without posterior acoustic shadowing at the pancreatic head. The main pancreatic duct was mildly dilated (Fig. 1C). EUS guided biopsy was performed, yielding pathological diagnosis of gastrointestinal stromal tumor. Positron emission tomography (PET) detected hypermetabolic lesion measured at 7 cm (SUVmax 4.0) in the pancreatic head without evidence of abnormal hypermetabolic lesion, suggesting LN or distant metastasis (Fig. 1D).
Under a preoperative diagnosis of a duodenal GIST or pancreatic neuroendocrine tumor, we performed a pylorus preserving pancreatoduodenectomy for this lesion. On pathologic gross examination, the tumor measured at 7 cm in its greatest dimension almost entirely involved the pancreatic head. It was easily separated from duodenum. Its cut surface was rubbery and white. Surrounded by a thin pseudocapsule, it was well-demarcated (Fig. 2A). Microscopically, the tumor was composed of spindle cells (Fig. 2B). Mitotic count was 5/50 high-power fields (HPF). Immunohistochemically, neoplastic cells were diffuse. They were weakly positive for antibodies against C-KIT(CD117) but positive for CD 34 and vimentin (Fig. 2C and D). However, smooth-muscle actin reactions with antibodies against S-100 or desmin were negative. Based on above findings, the tumor was finally diagnosed as EGIST originating from the pancreas.
She had an uneventful postoperative course. The patient was discharged home on postoperative day 20. Adjuvant therapy was not started due to the low mitotic rate of the tumor and its intermediate size. She is free of recurrence of EGIST after the surgery.
EGISTs arising in the pancreas are extremely rare. Reports of pancreatic EGISTs are limited to individual case reports and small number of case series. A total of 17 patients who were confirmed as pancreatic GISTs after resection were collected in this study.456789101112131415161718 The clinicopathological features and outcomes of these cases are summarized in Table 1. Age of these patients ranged from 30 to 74 years (median, 54.7 years; mean, 53.1 years). Eight patients were males and nine were females. Most clinical presentations included vague abdominal pain or discomfort, weight loss, and fatigue. However, seven (41.2%) cases were found incidentally during a workup for unrelated conditions. These tumors ranged from 6 to 35 cm in maximum diameter (median, 10.0 cm; mean, 11.9 cm). These tumors could occur in any part of the pancreas. Their most common location was head (6/17, 35.3%) and tail (6/17, 35.3%), followed by body & tail (3/17, 17.6%) and head & body (2/17, 11.8%) in the pancreas.
Characteristic immunohistochemical profile of GIST has been proven to be very helpful in its diagnosis. On immunohistochemistry, positivity of c-Kit (CD117) confirms the diagnosis of GIST. C-kit gene is expressed in 95% of cases. CD 34 is also expressed in 60-70% of GIST cases. The frequency of CD 34 positivity depends on the location of GISTs. The frequency of positive CD34 is high in GISTs of the esophagus and colon (95%). However, it is relatively low in small bowel and extra-gastrointestinal sites. GISTs may also show variable positivities for other immune markers, such as SMA (30–40%), S-100 (5%), and desmin (1–25%).19 In our review, 14 (82.4%) of 17 pancreatic EGISTs showed positivity for CD117 while 9 (52.9%) cases were positive for CD 34.
GIST exhibits a broad spectrum of clinical behaviors. The prognosis of patients with GIST depends on the biological behavior of GIST. Fletcher et al.1 have defined the criteria to estimate risks of aggressive behavior and metastasis of GIST using tumor dimension (cm) and mitotic count (/50 HPF). According to their criteria, GISTs are divided into risk categories of very low (<2 cm, <5/50 HPF), low (2–5 cm, <5/50 HPF), intermediate (<5 cm, 6–10/50 HPF or 5–10 cm, <5/50 HPF), and high risk (>5 cm, >5/50 HPF or >10 cm, any mitotic count) of metastasis.1 In our review, the risk of aggressive behavior according to Fletcher criteria was high in 13 (76.5%) cases. The remaining three (11.8%) cases had intermediate risk. The frequency of high risk aggressive behavior tended to be high for GIST.
It is well-known that resection should be considered as the first treatment choice for resectable localized GIST because high potential of malignancy is associated with cases of GIST. Complete surgical resection with negative microscopic margins is the standard treatment for GISTs.20 Systemic regional lymphadenectomy is not generally considered because lymph node metastasis is rare (prevalence of about 1%).21
Response rates of GISTs to conventional chemotherapy and radiotherapy are 10% and 5%, respectively.913 Adjuvant treatment with imatinib can be provided in order to enhance the possibility of curing the cancer by eradicating microscopic lesions that might remain after complete resection of visual tumors.19
DeMattero et al.22 have reported that most recurrence of GIST will occur within 24 months after resection, with liver and peritoneum being the most common site of recurrence. Reith et al.23 reported that 39% of patients with EGIST developed metastatic disease or died from tumors within a short period, suggesting that EGIST was an aggressive type of stromal tumor. In our review, majority (76.5%) of pancreatic EGISTs are classified to the high risk category at the time of diagnosis. Within 30 months after resection, recurrence occurred in 7 (7/17, 41.2%) patients, with hepatic metastasis being more frequent (6/7, 85.7%) than other sites.
Thus, complete surgical resection with negative microscopic margin should be considered as first-line treatment for pancreatic EGIST. Intense surveillance after surgical treatment is advocated. Adjuvant treatment following surgical treatment should be considered to enhance the possibility of curing the cancer. It can prevent recurrences or metastasis because pancreatic EGIST has high potential for malignancy or recurrence.
Our review on pancreatic EGISTs is limited and insufficient to make a conclusion regarding their clinical features. These manifested large masses tended to have aggressive biological and clinical behavior. Therefore, pancreatic EGISTs need to be carefully differentiated from their gastrointestinal counterparts. Adequate surgical intervention and postoperative adjuvant treatment are necessary for EGISTs.
Figures and Tables
Fig. 1
Imaging study findings. (A and B) An abdominal computed tomography (CT) scan showing a well-enhanced mass measuring at 6.5 cm×6.5 cm with central low dense lesion appearing as necrosis (axial & coronal). (C) Positron emission tomography (PET) showing a hypermetabolic lesion measured at 7 cm (SUVmax 4.0) in the pancreatic head without evidence of abnormal hypermetabolic lesion, suggesting lymph node or distant metastasis. (D) Endoscopic ultrasonography (EUS) revealing a well-defined homogenous hypoechoic mass like lesion (EUS-guided biopsy was done) without posterior acoustic shadowing at the pancreatic head. The main pancreatic duct was mildly dilated.
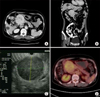
Fig. 2
Pathologic study findings. (A) On pathologic gross examination, the tumor measured at 7 cm in its greatest dimension involving the pancreatic head. Its cut surface was rubbery and white. Surrounded by a thin pseudocapsule, it was well-demarcated, infiltrating the duodenal wall. (B) The tumor was composed of spindle cells (H&E, ×200). (C) Immunohistochemical examination revealing diffuse and weak CD 117 positivity. (D) Tumor cells showing positive immunoreactivity for CD 34.

References
1. Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002; 33:459–465.
2. Agaimy A, Wünsch PH. Gastrointestinal stromal tumours: a regular origin in the muscularis propria, but an extremely diverse gross presentation. A review of 200 cases to critically re-evaluate the concept of so-called extra-gastrointestinal stromal tumours. Langenbecks Arch Surg. 2006; 391:322–329.
3. Park JK, Choi SH, Lee S, Min KO, Yun SS, Jeon HM. Malignant gastrointestinal stromal tumor of the gallbladder. J Korean Med Sci. 2004; 19:763–767.
4. Neto MR, Machuca TN, Pinho RV, Yuasa LD, Bleggi-Torres LF. Gastrointestinal stromal tumor: report of two unusual cases. Virchows Arch. 2004; 444:594–596.
5. Yamaura K, Kato K, Miyazawa M, Haba Y, Muramatsu A, Miyata K, et al. Stromal tumor of the pancreas with expression of c-kit protein: report of a case. J Gastroenterol Hepatol. 2004; 19:467–470.
6. Krska Z, Pesková M, Povýsil C, Horejs J, Sedlácková E, Kudrnová Z. GIST of pancreas. Prague Med Rep. 2005; 106:201–208.
7. Daum O, Klecka J, Ferda J, Treska V, Vanecek T, Sima R, et al. Gastrointestinal stromal tumor of the pancreas: case report with documentation of KIT gene mutation. Virchows Arch. 2005; 446:470–472.
8. Showalter SL, Lloyd JM, Glassman DT, Berger AC. Extra-gastrointestinal stromal tumor of the pancreas: case report and a review of the literature. Arch Surg. 2008; 143:305–308.
9. Trabelsi A, Yacoub-Abid LB, Mtimet A, Abdelkrim SB, Hammedi F, Ali AB, et al. Gastrointestinal stromal tumor of the pancreas: a case report and review of the literature. N Am J Med Sci. 2009; 1:324–326.
10. Padhi S, Kongara R, Uppin SG, Uppin MS, Prayaga AK, Challa S, et al. Extragastrointestinal stromal tumor arising in the pancreas: a case report with a review of the literature. JOP. 2010; 11:244–248.
11. Saif MW, Hotchkiss S, Kaley K. Gastrointestinal stromal tumors of the pancreas. JOP. 2010; 11:405–406. author reply 412.
12. Rao RN, Vij M, Singla N, Kumar A. Malignant pancreatic extra-gastrointestinal stromal tumor diagnosed by ultrasound guided fine needle aspiration cytology. A case report with a review of the literature. JOP. 2011; 12:283–286.
13. Čečka F, Jon B, Ferko A, Šubrt Z, Nikolov DH, Tyčová V. Long-term survival of a patient after resection of a gastrointestinal stromal tumor arising from the pancreas. Hepatobiliary Pancreat Dis Int. 2011; 10:330–332.
14. Vij M, Agrawal V, Pandey R. Malignant extra-gastrointestinal stromal tumor of the pancreas. A case report and review of literature. JOP. 2011; 12:200–204.
15. Yang F, Jin C, Fu D, Ni Q. Extra-gastrointestinal stromal tumor of the pancreas: clinical characteristics, diagnosis, treatment, and outcome. J Surg Oncol. 2011; 103:739–740.
16. Kim HH, Koh YS, Park EK, Seoung JS, Hur YH, Kim JC, et al. Primary extragastrointestinal stromal tumor arising in the pancreas: report of a case. Surg Today. 2012; 42:386–390.
17. Tian YT, Liu H, Shi SS, Xie YB, Xu Q, Zhang JW, et al. Malignant extra-gastrointestinal stromal tumor of the pancreas: Report of two cases and review of the literature. World J Gastroenterol. 2014; 20:863–868.
18. Elgeidie A, El-Magd EA, El-Maaty SRA, El-Hawary AK. Pancreatic gastrointestinal stromal tumor: a case report. Int J Surg Case Rep. 2016; 29:67–70.
19. Kang YK, Kang HJ, Kim KM, Sohn T, Choi D, Ryu MH, et al. Clinical practice guideline for accurate diagnosis and effective treatment of gastrointestinal stromal tumor in Korea. Cancer Res Treat. 2012; 44:85–96.
20. Valsangkar N, Sehdev A, Misra S, Zimmers TA, O'Neil BH, Koniaris LG. Current management of gastrointestinal stromal tumors: surgery, current biomarkers, mutations, and therapy. Surgery. 2015; 158:1149–1164.
21. Joensuu H, Hohenberger P, Corless CL. Gastrointestinal stromal tumour. Lancet. 2013; 382:973–983.
22. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000; 231:51–58.
23. Reith JD, Goldblum JR, Lyles RH, Weiss SW. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol. 2000; 13:577–585.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download