Abstract
Backgrounds/Aims
The impact of pre-operative biliary stenting (PBS) in patients undergoing pancreaticoduodenectomy on post-operative infectious complications is unclear. Therefore, the purpose of this study is to investigate the relationship between PBS and post-operative infectious complications, to determine the effect of PBS on bile bacteriology, and to correlate the bacteriology of bile and bacteria cultured from post-operative infectious complications in our institute.
Methods
Details of 51 patients undergoing pancreaticoduodenectomy January 2011-April 2015 were reviewed. Of 51 patients, 30 patients underwent pre-operative biliary stenting (PBS group) and 21 patients underwent pancreaticoduodenectomy without pre-operative biliary stenting. Post-operative infectious complications were compared between the two groups.
Results
Overall post-operative infectious complication rate was 77% and 67% in the PBS and non-PBS groups respectively. Wound infection was the main infectious complication followed by intraabdominal abscess. The rate of wound infection doubled in the PBS group (50% vs 28%). There was slight increase in incidence of intraabdominal abscess in PBS group (53% vs 46%). 80% of PBS patients had positive intraoperative bile culture as compared to 20% in non-PBS group.
Pancreaticoduodenectomy (PD, Whipple's procedure) is regarded as the standard of care for periampullary and ampullary malignancies. In the past few decades, perioperative morbidity and mortality have improved tremendously with certain centers reporting mortality rates of less than 5%.123 These groups of patients often present with obstructive jaundice, associated with higher morbidity due to impairment of immunity and nutrition.1 From a cellular immunity perspective, obstructive jaundice impairs liver T-lymphocyte and mononuclear cell function in mice models, thereby increasing susceptibility to infection.45 Preoperative biliary drainage by means of endoscopic biliary stenting or percutaneous transhepatic biliary stenting (PTC) is proposed to improve outcomes by re-establishing entero-hepatic circulation prior to surgery.6 Biliary decompression provides symptomatic relief to patients with pruritus and cholangitis, or can serve as a temporizing measure if surgery is delayed or neoadjuvant therapy is considered. However, an opposing body of evidence reports worse outcomes in patients that undergo preoperative biliary decompression.3678910 Infectious complications such as wound infection (WI), intraabdominal abscess (IAA), bactaraemia and urinary tract infection (UTI) are higher with biliary decompression.6 Incidence of morbidity post-PD has been difficult to interpret due to the heterogeneous post-operative parameters analyzed.111121314 Different definitions used for infectious complications have clouded true incidence of individual complications.11
The objectives of this study are to evaluate the relationship between pre-operative biliary stenting (PBS) and post-operative infectious complications, to determine the effect of PBS on intra-operative bile bacteriology, and to correlate the bacteriology of bile and bacteria cultured from post-operative infectious complications.
Ethical approval for this study was obtained from the hospital quality improvement committee. From January 2011–April 2015, 58 PDs were planned in our institute. Seven cases were abandoned intra-operatively due to inoperable disease not detected on pre-operative imaging and were excluded from analysis. All operations were elective, and all patients were free from urinary tract, bowel or skin infections prior to and at time of surgery. PBS was conducted endoscopically in our center using either a plastic (n=48) or metal stent (n=5) with or without sphincterotomy. Antibiotics were not routinely administered before endoscopy. All patients received prophylactic antibiotics perioperatively. Bile cultures (BIC) were collected intra-operatively at discretion of the treating surgeon. All patients had one or more drains placed at the end of procedure. Site-specific microbiological cultures for aerobic, anaerobic and fungal organisms were collected post-operatively if an infection was suspected.
Infectious complications were defined as clinically relevant septic complications occurring with physical signs, fever, leukocytosis and positive microbiological cultures and/or imaging studies. Bacteremia was defined as positive blood culture collected from two separate peripheral sites during the same febrile episode (temperature >38℃). UTI was defined as a positive urine culture with associated urinary tract symptoms (i.e. frequency, dysuria). IAA was defined as a culture-positive collection from percutaneous drainage requiring treatment with intravenous antibiotics and/or prolonged percutaneous drainage. Postoperative WI was defined as culture-positive collection obtained from swabs and requiring either antibiotics or wound dressing.
Details of patient characteristics, reason for PD, pre-operative biochemistry results, pre-operative procedures conducted, details of biliary stenting and stent-related complications, biliary and other microbiology cultures, postoperative imaging and complications, neoadjuvant and adjuvant chemotherapy or radiotherapy, length of stay and post-operative mortality were collected and analyzed.
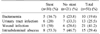
All 51 PDs were conducted successfully. Patient demographics were similar between both groups (Table 1). There were 28 male and 23 female patients with a median age of 66 years. Of 51 patients, 31 (60.8%) and 20 (39.2%) were segregated into the PBS and non-PBS groups respectively.
Of 31 patients that underwent PBSs, 30 were conducted endoscopically, while one patient required assistance by percutaneous transhepatic cholangiography due to difficult anatomy (Table 2). Median time to PD post-PBS was 45 days. Only 3 patients received intravenous antibiotics prior to PBS. Most patients (73%) had sphincterotomy conducted during PBS. Two patients required readmission post-PBS for persistent cholestasis and cholangitis. Complication rate post-PBS was 7% (n=2; one pancreatitis and cholangitis each).
All PDs except one were conducted for malignancy. Majority of tumors were in the pancreas and did not differ between both groups (Table 1).
Intraoperative bile culture results are detailed in Table 3. Twenty-four patients had bile culture collected intra-operatively; 17 in the PBS and 7 in the non-PBS groups respectively. Of 24 BICs, 20 had positive microbiological growths. Majority of these BICs were polymicrobial (65%). The most common cultured BIC was Klebsiella oxytoca (n=7) and Escherichia coli (n=7) followed by Klebsiella pneumoniae (n=6) and Streptococcus anginosus (n=6). Fungal microorganisms were not common in our study (n=3).
Overall incidence of infectious complication was 77% in the PBS group and 67% in the non-PBS group. From all infectious complications, WI was highest (41%), followed by IAA (29%), urinary tract infection (26%) and bacteremia (20%) (Table 4). Most cultures in IAA demonstrated polymicrobial growth, Enterobacter cloacae was the most common microorganism cultured followed by Escherichia coli. Fungal microorganisms again were not commonly cultured.
In evaluating WI, its incidence in the PBS group was almost double (50% vs 28%) compared to the non-PBS group. We observed mild increase in IAA in the PBS group compared to non-PBS group (53% vs 46%). Incidence of other infectious complications (UTI and bactaraemia) were similar in both groups.
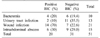
In analyzing microbiological association between BIC and PBS, 80% of patients with PBS had positive BIC. In comparison, 20% of patients in the non-PBS (n=7) group had positive BIC; 70% of patients with WI had positive BICs; no differences between positive and negative BICs were observed in other infectious complication groups (Table 5). There was no correlation between microorganisms of BIC and microorganisms of WI, IAA, UTI and bacteremia.
Median length of stay in this study was 25 days (23 days in the PBS group vs 25 days in the non-PBS group). Approximately half of patients (51.6%) and one third (30%) in the PBS and non-PBS groups respectively received adjuvant chemotherapy. A minority of patients received adjuvant radiotherapy. During median follow-up of 36 months (19–65 months), 16 patients died; 15 cases were secondary to disease progression, and one patient died intra-operatively secondary to distributive shock. Median survival of these patients was 12 months (mean of 14.3 months; 0 day-26 months).
Benefits of preoperative biliary drainage for patients with peri-ampullary and ampullary malignancy undergoing PD remain largely controversial. Several studies question its value given morbidity and complications associated with it.81516 Biliary drainage in earlier studies were conducted via PTC or a mixture of PTC and PBS. Therefore, it may not truly reflect true incidence of complications. This is one center's retrospective study that provides further insight into the relationship between pre-operative biliary stenting and post-operative infectious complications.
Our complication rate post-PBS was low in comparison to recent literature.6161718 Results of our study suggest that pre-PBS prophylactic antibiotics may not be necessary as we demonstrated no increase in infectious complications when antibiotic prophylaxis was not administered.
As clearly summarized in Velanovich and colleagues' work, various definitions for complications have an impact on the ultimate reported incidence of outcomes.11 Significant findings of this study concur with literature. Wound infection was highest reported complication post-PD in our series, higher than the reported average in literature (5.5% to 21.5%).12369121920 When assessed for its relationship with PBS, we observed significantly higher wound infection rate in the PBS group compared to the non-PBS group, and overall was higher than other reported series (8–29%).611121419212223 IAA was second most encountered complication. Our rate of IAA was higher compared to current literature.123111219 This disparity in results may be explained by diagnostic criteria used, with several studies defining IAA based on a radiologically proven collection with documented febrile episodes; in our study positive microbiological culture via percutaneous drainage was required for IAA to be diagnosed in addition. Like WI, we observed that IAA rates were higher in the PBS group compared to the non-PBS group. This positive association between PBS and IAA was reported in other series.122224 Rates of UTI and bacteremia were low in PBS and non-PBS groups. We postulate that high WI and IAA rates in the PBS group is due to direct contamination by colonized bile (bactobilia) on superficial and deep tissues when the common bile duct is transected during PD.
We observed that PBS increased likelihood of bactobilia (80% vs 20%). A large percentage of cultured organisms were polymicrobial, as observed in other studies.3623 Klebsiella oxytoca was the most commonly grown microorganism. Escherichia coli and Klebsiella pneumoniae were commonly observed in our series, and reflects microbiological trends of other series.2362023 Fungal growth was considerably low in our cohort, in line with findings from other authors. Only one study reported 23% fungal growth.3 Due to its low incidence, we do not recommend pre-operative administration of anti-fungal therapy.
This study demonstrates that positive BIC was associated with higher incidence of WI. This finding is in line with several published studies.323 We were unable to demonstrate similar relationship between positive BIC and IAA (Table 5). Other studies however, demonstrate this relationship.3
We acknowledge limitations of this non-randomized study, including the small sample size, reflective of a disease that has low resectability. Statistical analysis could not be conducted due to sample sizes.
In conclusion, our single-center study provides further evidence that patients that undergo PBS prior to PD are more likely to be associated with bactobilia, with Klebsiella oxytoca, Escherichia coli and Klebsiella pneumoniae as the most common microorganisms. The latter two organisms are widely recognized organisms in post-PBS infections. This study demonstrates that patients that receive PBS prior to pancreaticoduodenectomy are at higher risk of developing post-operative wound infections and intra-abdominal collections. Microbiological analysis of intra-operative bile culture is unlikely to offer additional useful information in post-operative infectious complications.
References
1. Sahora K, Morales-Oyarvide V, Ferrone C, Fong ZV, Warshaw AL, Lillemoe KD, et al. Preoperative biliary drainage does not increase major complications in pancreaticoduodenectomy: a large single center experience from the Massachusetts General Hospital. J Hepatobiliary Pancreat Sci. 2016; 23:181–187.
2. Gavazzi F, Ridolfi C, Capretti G, Angiolini MR, Morelli P, Casari E, et al. Role of preoperative biliary stents, bile contamination and antibiotic prophylaxis in surgical site infections after pancreaticoduodenectomy. BMC Gastroenterol. 2016; 16:43.
3. Povoski SP, Karpeh MS Jr, Conlon KC, Blumgart LH, Brennan MF. Preoperative biliary drainage: impact on intraoperative bile cultures and infectious morbidity and mortality after pancreaticoduodenectomy. J Gastrointest Surg. 1999; 3:496–505.
4. Kawarabayashi N, Seki S, Hatsuse K, Kinoshita M, Takigawa T, Tsujimoto H, et al. Immunosuppression in the livers of mice with obstructive jaundice participates in their susceptibility to bacterial infection and tumor metastasis. Shock. 2010; 33:500–506.
5. Katz SC, Ryan K, Ahmed N, Plitas G, Chaudhry UI, Kingham TP, et al. Obstructive jaundice expands intrahepatic regulatory T cells, which impair liver T lymphocyte function but modulate liver cholestasis and fibrosis. J Immunol. 2011; 187:1150–1156.
6. Jagannath P, Dhir V, Shrikhande S, Shah RC, Mullerpatan P, Mohandas KM. Effect of preoperative biliary stenting on immediate outcome after pancreaticoduodenectomy. Br J Surg. 2005; 92:356–361.
7. van der Gaag NA, de Castro SM, Rauws EA, Bruno MJ, van Eijck CH, Kuipers EJ, et al. Preoperative biliary drainage for periampullary tumors causing obstructive jaundice; DRainage vs. (direct) OPeration (DROP-trial). BMC Surg. 2007; 7:3.
8. Ngu W, Jones M, Neal CP, Dennison AR, Metcalfe MS, Garcea G. Preoperative biliary drainage for distal biliary obstruction and post-operative infectious complications. ANZ J Surg. 2013; 83:280–286.
9. Sewnath ME, Birjmohun RS, Rauws EA, Huibregtse K, Obertop H, Gouma DJ. The effect of preoperative biliary drainage on postoperative complications after pancreaticoduodenectomy. J Am Coll Surg. 2001; 192:726–734.
10. Iacono C, Ruzzenente A, Campagnaro T, Bortolasi L, Valdegamberi A, Guglielmi A. Role of preoperative biliary drainage in jaundiced patients who are candidates for pancreatoduodenectomy or hepatic resection: highlights and drawbacks. Ann Surg. 2013; 257:191–204.
11. Velanovich V, Kheibek T, Khan M. Relationship of postoperative complications from preoperative biliary stents after pancreaticoduodenectomy. A new cohort analysis and meta-analysis of modern studies. JOP. 2009; 10:24–29.
12. Hodul P, Creech S, Pickleman J, Aranha GV. The effect of preoperative biliary stenting on postoperative complications after pancreaticoduodenectomy. Am J Surg. 2003; 186:420–425.
13. Smith RA, Dajani K, Dodd S, Whelan P, Raraty M, Sutton R, et al. Preoperative resolution of jaundice following biliary stenting predicts more favourable early survival in resected pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2008; 15:3138–3146.
14. Pisters PW, Hudec WA, Hess KR, Lee JE, Vauthey JN, Lahoti S, et al. Effect of preoperative biliary decompression on pancreaticoduodenectomy-associated morbidity in 300 consecutive patients. Ann Surg. 2001; 234:47–55.
15. Hatfield AR, Tobias R, Terblanche J, Girdwood AH, Fataar S, Harries-Jones R, et al. Preoperative external biliary drainage in obstructive jaundice. A prospective controlled clinical trial. Lancet. 1982; 2:896–899.
16. Sewnath ME, Karsten TM, Prins MH, Rauws EJ, Obertop H, Gouma DJ. A meta-analysis on the efficacy of preoperative biliary drainage for tumors causing obstructive jaundice. Ann Surg. 2002; 236:17–27.
17. van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ, van der, Kubben FJ, et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med. 2010; 362:129–137.
18. Glomsaker T, Hoff G, Kvaløy JT, Søreide K, Aabakken L, Søreide JA, et al. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg. 2013; 100:373–380.
19. Martignoni ME, Wagner M, Krähenbühl L, Redaelli CA, Friess H, Büchler MW. Effect of preoperative biliary drainage on surgical outcome after pancreatoduodenectomy. Am J Surg. 2001; 181:52–59.
20. Mohammed S, Evans C, VanBuren G, Hodges SE, Silberfein E, Artinyan A, et al. Treatment of bacteriobilia decreases wound infection rates after pancreaticoduodenectomy. HPB (Oxford). 2014; 16:592–598.
21. Gerke H, White R, Byrne MF, Stiffier H, Mitchell RM, Hurwitz HI, et al. Complications of pancreaticoduodenectomy after neoadjuvant chemoradiation in patients with and without preoperative biliary drainage. Dig Liver Dis. 2004; 36:412–418.
22. Heslin MJ, Brooks AD, Hochwald SN, Harrison LE, Blumgart LH, Brennan MF. A preoperative biliary stent is associated with increased complications after pancreatoduodenectomy. Arch Surg. 1998; 133:149–154.
23. Howard TJ, Yu J, Greene RB, George V, Wairiuko GM, Moore SA, et al. Influence of bactibilia after preoperative biliary stenting on postoperative infectious complications. J Gastrointest Surg. 2006; 10:523–531.
24. Srivastava S, Sikora SS, Kumar A, Saxena R, Kapoor VK. Outcome following pancreaticoduodenectomy in patients undergoing preoperative biliary drainage. Dig Surg. 2001; 18:381–387.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download