Abstract
Backgrounds/Aims
To determine the importance of critical view of safety techniques in laparoscopic cholecystectomy.
Methods
A total of 120 patients were included in the study, between January 2015 to March 2016. Hydrodissection was performed for cases presenting with severe adhesions or cholecystitis. A critical view of safety was performed for all patients undergoing the procedure for isolation of cystic duct and cystic artery with cystic plate dissection. Demographic characteristics of the patients, as well as intraoperative and postoperative minor or major complications were recorded.
Results
A total of 81 (67.5%) female and 39 (32.5%) male patients succesfully underwent surgeries following the critical view of safety and hydrodissection technique. Acute/chronic cholecystitis, or severe adhesions in the surgical field, were detected in 34 (28.3%) patients. There were no intraoperative or postoperative biliary complications. Wound infection was detected in 5 (4.1%) patients. All patients were discharged on either the first, second or third postoperative day.
A gold standard in the treatment of cholelithiasis, laparoscopic cholecystectomy (LC) is the most common procedure in general surgery. The most commonly used surgical technique is the infundibular approach, characterized by dissection of the calot triangle, clipping the cystic artery and the cystic duct. Bile duct injuries are encountered in 0.3% to 0.5% of laparoscopic cholecystectomies, and has remained the since the introduction of laparoscopic surgery.1 In the United States, approximately 34% to 49% of surgeons have encountered a major bile duct injury during their lifetime experience.2 Misperception of intraoperative anatomy during cholecystectomy is one of the most important causes of bile duct injuries. The common bile duct is usually mistaken as the cystic duct; such biliary injuries need to be further managed by experienced hepatobiliary centers. To decrease the incidence of bile duct injuries in LC, Strasberg and his colleagues introduced the critical view of safety (CVS) technique in 1995. Hydrodissection was another technique introduced for difficult cholecystectomies.
In this study, we analysed the clinical value of CVS techniques in laparoscopic cholecystectomy.
Patients diagnosed with cholelithiasis between January 2015 to March 2016, were operated at the Fatih Sultan Mehmet Training and Research Hospital - Department of General Surgery. Patients who were successfully operated with the CVS and hydrodissection technique were included in this study. All surgeries were performed by the same surgeon. Hydrodissection was performed in patients with findings of severe adhesions or acute/chronic cholecystitis (Fig. 1).
The LC was performed by the four-port technique: the first port is a 10 mm infraumbilical camera port inserted directly or using the open technique and insufflating with CO2. The other three ports were then inserted under direct camera vision. The gallbladder was retracted up to the right axillary direction. The calot triangle was explored with the lateral retraction of Hartman's pouch. Dissection of the hepatoduodenal ligament above the cystic artery and cystic duct was performed using an electrocautary or blunt laparoscopic traction
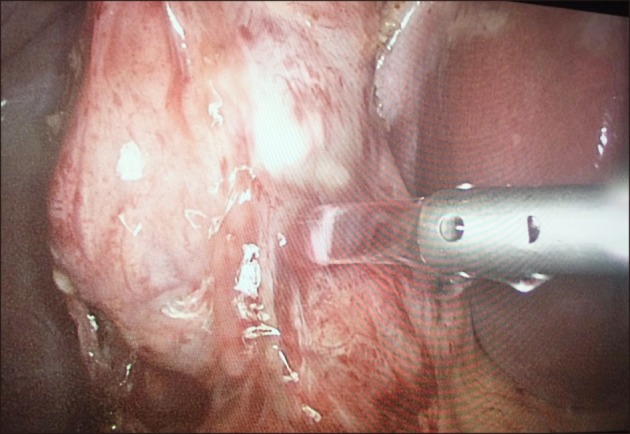
Dissection of the gallbladder peritoneum above the cystic artery with the help of electrocautery hook, is an important step in the procedure. The right side of the gallblader peritoneum was opened, and a hole above the cystic artery was thus formed. Laparoscopic dissector was used for isolating the cystic duct and artery. The cystic plate posterior to cystic artery was dissected, exposing the liver. After meticulous dissection, the cystic artery and duct were isolated (Fig. 2). They were then clipped and cut.
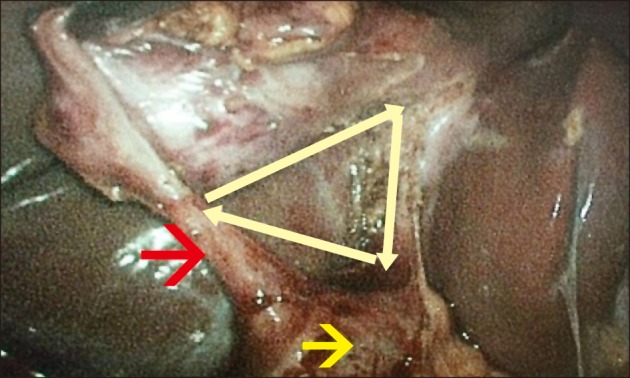
In hydrodissection, about 5-10 ml of saline solution (0.9%) was pumped into the Hartman region, Calot triangle, and medial and lateral peritoneal leafs of the gallbladder. The tissues around these region became edematous, following which dissection was performed (Figs. 3, 4, 5). The demographic characteristics of patients, and their intraoperative and postoperative biliary and nonbiliary complications, were duly recorded.
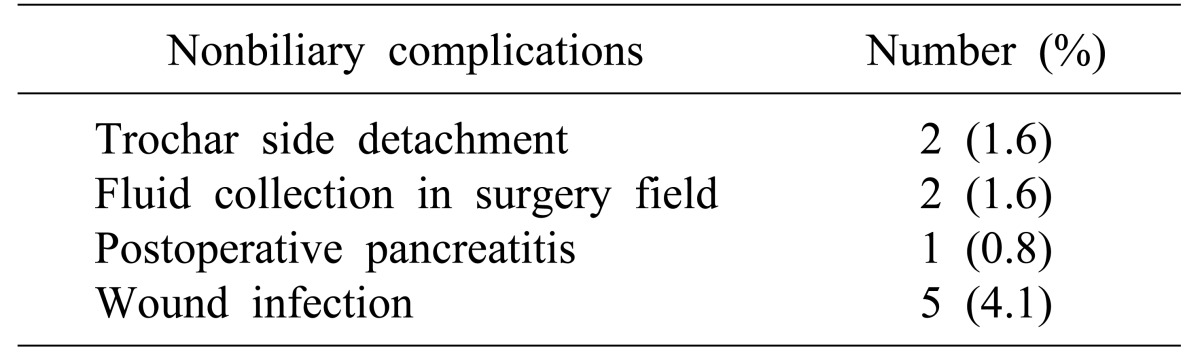
A total of 120 patients wetre enrolled in this study: 81 (67.5%) women and 39 (32.5%) men. Acute and chronic cholecystitis or severe adhesions were seen in 34 (28.3%) patients. A CVS technique was performed in all patients. Hydrodissection was performed in 34 patients with acute/chronic cholecystitis or severe adhesions. In 2 patients, accessory bile duct was detected in the gallbladder bed and clipped. There were no major intraabdominal bleeds during surgery. To date, there have been no reports of cholangiography being performed intraoperatively.The median operation time was 50 minute (range, 30 to 120 minutes). Bile was absent in patients with abdominal drains. No minor or major bile duct injuries were reported in the postoperative period. Wound infection was detected in 5 (4.1%) patients treated with oral antibiotheraphy. Only 1 patient was treated conservatively due to pancreatitis in the postoperative period. Non-biliary complications are mentioned in Table 1. Patients were discharged on the first (110 patients), second (7 patients) or third (3 patients) day after surgery.
Bile duct injuries are important complications for morbidity and mortality after LC. The most common risk factors for such injuries are experience of the surgical team, inflammed gallbladder, and nearby anatomical structures with biliary anatomical variations.34 Acute cholecystitis, a common clinical condition, has a three times more likelihood of causing a biliary injury than a standard laparoscopic procedure.5 In a retrospective study of 4,445 laparoscopic cholecystectomies, inflammation at the Calot's triangle was found to be an important risk factor for injury.6 Although most biliary injuries occur in the first 100 laparoscopic cholecystectomies performed by surgeons, it can also be seen in experienced hands.
Strasberg et al.7 first suggested a new surgical strategy called the CVS, to minimize the risk of bile duct injuries in LC. This technique has three main sections: (1) dissection of the Calot's triangle, including hepatoduodenal ligament, (2) mobilization of the lowest part of the gallbladder, and (3) isolation and identification of the two main structures (cystic duct and cystic artery). In fact, the CVS technique is a simple procedure, which can be easily applied by all surgeons cholecystectomy. This technique was implemented by us, as follows. First, the hepatoduodenal ligament was dissected with the hook cother. The lateral serosal leaf of the gallbladder was opened, following which medial dissection was carried out. We used both the hook cother and laparoscopic dissector for isolation of the cystic duct and artery. No anatomical structures were clipped before concluding the dissection. Vettoretto et al.8 performed 90 cholecystectomies with CVS technique. They compared these patients with 84 patients operated by the classical infundibular technique. Only 1 cystic duct leak was reported in the CVS group, as against 2 intraoperative hemorrhages in patients operated by the infundibular technique. They concluded that although CVS technique has a similar rate of biliary and hemorrhagic complications, it is a gold standart in LC due to the shorter operative time.8 Honda et al.9 used the CVS technique with some modifications. They first dissected the subserosal layer of the gallbladder above the level of rouviere sulcus in the right hepatic lobe of the gallbladder. This technique was especially useful in cases with severe inflammation of the Calot's triangle.
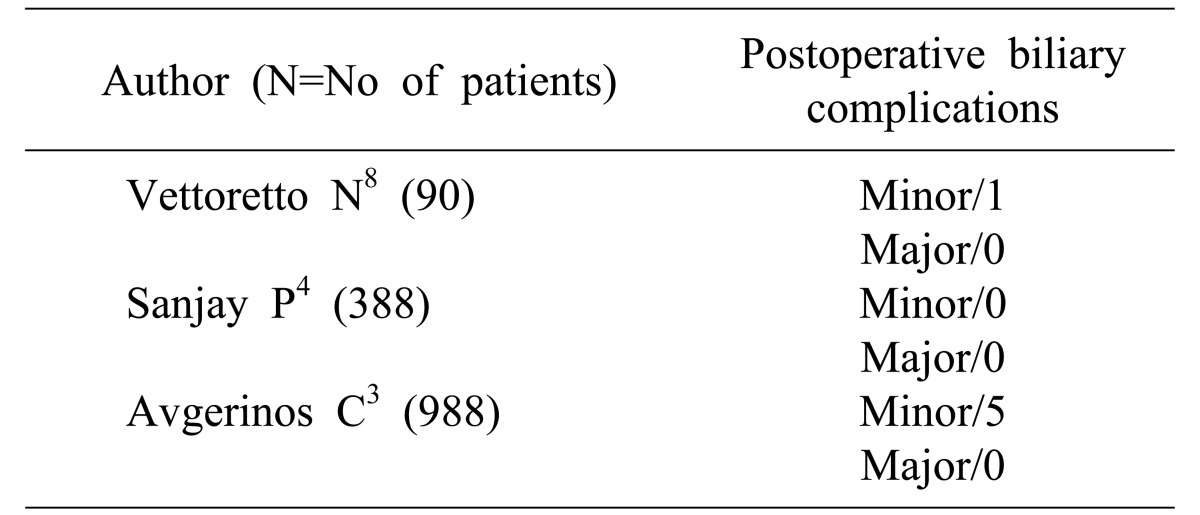
Today, the CVS technique is accepted as the most effective method for reducing morbidity and mortality associated with laparoscopic cholecystectomy. The European Association of Endoscopic Surgery (EAES) recommends the CVS as the most effective approach to prevent bile duct injury.10 Hence, the CVS approach to LC should be integrated into national guidelines and made mandatory, in particular during training of surgical residents. O Kelly performed a nationwide research in Ireland among general surgeons who perform laparoscopic cholecystectomy. The CVS was used as a single method by 31% (n=27) of surgeons. However, about 13% of surgeons were neither using CVS technique nor the infundibular approach.11 The literature with CVS is summarized in Table 2.
The fundus-down technique is a nother procedure used for cases in which the Calot's triangle is difficult to dissect. This technique initiates with the dissection of the gallbladder from the liver bed. Although a safe procedure, vascular injuries can occur near the Hartman pouch in cases with severe inflammation, with injury of the right hepatic artery and veins.5
The role of intraoperative cholangiography is still controversial in LC. While some authors believe that intraoperative cholangiography can reduce biliary duct injuries, others are of the opinion that routine application of this procedure is unnecessary and time consuming. The introduction of CVS technique is a good alternative to intraoperative cholangiography.4 In this study, intraoperative cholangiography has not been performed. Hydrodissection has been used in the past in open cholecystectomy to facilitate dissection in difficult cases. Naude et al.12 used hydrodissection technique in 133 cholecystectomies, and compared these with 48 controls. They reported that laparoscopic hydrodissection was associated with less bleeding, less gallbladder damage and stone spilling, and faster dissection time. Lubna and Masoom13 used the hydrodissection technique with a suction irrigation probe. They injected 5 ml saline solution, and performed dissection using a suction aspiration probe. Hydrodissection was performed successfully in 34 patients in this serial.
In conclusion, biliary duct injury during laparoscopic cholecystectomy is an important complication. In this study, we show that the CVS and hydrodissection techniques minimize the bile duct injury during laparoscopic cholecystectomy, including in difficult cases.
References
1. Yegiyants S, Collins JC. Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg. 2008; 74:985–987. PMID: 18942628.

2. Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001; 234:549–558. discussion 558-559. PMID: 11573048.
3. Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg. 2009; 13:498–503. PMID: 19009323.

4. Sanjay P, Fulke JL, Exon DJ. ‘Critical view of safety’ as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. J Gastrointest Surg. 2010; 14:1280–1284. PMID: 20535578.

5. Russell JC, Walsh SJ, Mattie AS, Lynch JT. Bile duct injuries, 1989-1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1996; 131:382–388. PMID: 8615723.
6. Ooi LL, Goh YC, Chew SP, Tay KH, Foo E, Low CH, et al. Bile duct injuries during laparoscopic cholecystectomy: a collective experience of four teaching hospitals and results of repair. Aust N Z J Surg. 1999; 69:844–846. PMID: 10613280.

7. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125. PMID: 8000648.
8. Vettoretto N, Saronni C, Harbi A, Balestra L, Taglietti L, Giovanetti M. Critical view of safety during laparoscopic cholecystectomy. JSLS. 2011; 15:322–325. PMID: 21985717.

9. Honda G, Iwanaga T, Kurata M, Watanabe F, Satoh H, Iwasaki K. The critical view of safety in laparoscopic cholecystectomy is optimized by exposing the inner layer of the subserosal layer. J Hepatobiliary Pancreat Surg. 2009; 16:445–449. PMID: 19259610.

10. Eikermann M, Siegel R, Broeders I, Dziri C, Fingerhut A, Gutt C, et al. Prevention and treatment of bile duct injuries during laparoscopic cholecystectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2012; 26:3003–3039. PMID: 23052493.

11. O'Kelly JA, De Marchi JA, Joyce WP. The critical view of safety in laparoscopic cholecystectomy: towards a national consensus. Ir Med J. 2015; 108:26. PMID: 25702354.
12. Naude GP, Morris E, Bongard FS. Laparoscopic cholecystectomy facilitated by hydrodissection. J Laparoendosc Adv Surg Tech A. 1998; 8:215–218. PMID: 9755913.

13. Lubna H, Masoom MR. Hydro-dissection - A simple solution in difficult laparoscopic cholecystectomy. Mymensingh Med J. 2015; 24:592–595. PMID: 26329960.
Fig. 1
The hydrodissection technique was performed in difficult cholecystectomy cases. The Hartman pouch (black arrow) of the gallbladder was seriously adhered to the duodenum (white arrow).
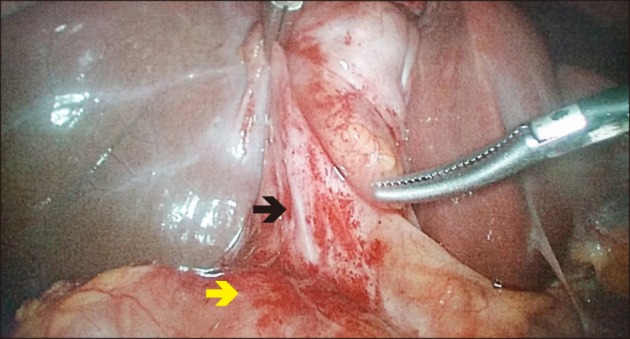
Fig. 4
The tissues became eudomatous after isotonic instillation. The common bile duct (white arrow) was easily separeted from the Hartman pouch of gallbladder (black arrow) with hydrodissection.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download