Abstract
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has recently been introduced as a new surgical technique to increase future liver remnant in patients with marginal liver volume contemplating major liver resection. We herein present two cases. Case 1: a 68-year-old male patient with colorectal liver metastasis was referred to our department. The future liver remnant (FLR) was 22%. We performed first-stage ALPPS and colorectal surgery concurrently and second stage operation was performed 8 days later. The patient discharged 28 days after the first-stage ALPPS procedure. Case 2: a 69-year-old male patient with a huge hepatic mass was referred for hepatic surgery. The FLR was 19%. After the first stage of the ALPPS procedure, acute renal failure and posthepatectomy liver failure occurred. The patient began to recover on the 5th postoperative day. At 10 days after the first stage, the patient completed the second-stage procedure. The patient discharged 23 days after the first-stage ALPPS procedure. So far many studies are currently underway to identify factors associated with the morbidity and mortality of the ALPPS procedure, it is necessary to continue follow-up studies and observe the results.
Surgical resection is the only treatment for patients with primary or metastatic hepatic malignancies. The treatment is especially recommended in the absence of extrahepatic malignancies. However, this approach is limited by the amount of functional future liver remnant (FLR) after hepatic resection. Surgeons want to preserve adequate FLR to avoid posthepatectomy liver failure. Removal of up to 75% of the total liver volume is feasible in a young patient with normal liver function. In the cases of underlying liver disease, such as chemotherapy-related injury or cirrhosis, an FLR of 40% or greater is required.12
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has been introduced recently, as a new surgical technique to increase FLR in patients with marginal liver volume contemplating major liver resection.3 The main indication for ALPPS is extensive bilobar colorectal liver metastases with an FLR less than 25%.4
The researchers hereby report two cases of ALPPS. The first case concerns simultaneous ALPPS and colorectal surgery, for a patient with extensive bilobar colon cancer liver metastases and a small predicted FLR. The second case concerns a patient with a mass larger than 15 centimeters, who underwent an ALPPS procedure.
A healthy and asymptomatic 68-year-old male patient was referred to our institution with synchronous hepatic metastasis of left colon cancer. The initial imaging studies showed seven metastases in the right lobe of liver and two metastases in the left lobe. The largest, which was in segment 6, measured 6.5 cm×5.5 cm×6 cm (Fig. 1). The physicians of the department of gastroenterology planned treatment with combination of bevacizumab and FOLFIRI (5-fluorouracil, leucovorin, and irinotecan) therapy. Over four months, the patient received seven cycles of bevacizumab and FOLFIRI combination therapy. After four months, the sizes of the hepatic metastases were decreased, with the largest one measuring 3.5 cm×3 cm (Fig. 2). To achieve hepatic clearance, a right hemihepatectomy with partial hepatectomy in left lobe was necessary.
The total liver volume (TLV) was 1,536 ml, the volume of the left lobe, and the FLR volume was 340 ml (22%). Liver function evaluation revealed albumin 3.9 g/dl, creatinine 1.25 mg/dl, international normalized ratio (INR) 0.89, serum bilirubin 0.40 mg/dl, and indocyanine green retention rate at 15 minutes (ICG-R15) 11.5%. The patient had no ascites and a platelet count of 272×103/mm3. Therefore, the researchers decided to achieve sufficient hypertrophy through ALPPS procedure. Three weeks after the last cycle of chemotherapy, the first stage of ALPPS with left hemicolectomy was performed.
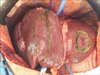
The operation started with a left hemicolectomy for left colon cancer, followed by ALPPS. After identification of the portal structures, the right portal vein was transected. The right hepatic artery and right hepatic vein were marked with vessel loops. The parenchyma was transected, through a demarcated line, for the right hemiliver and the right border of the middle hepatic vein. Enucleation was performed for lesions on the left lobe. Blood loss in the first stage was 650 ml (Figs. 3 and 4).
Computed tomography (CT) volumetry on day 7 after the first stage revealed 35% FLR. Therefore, we performed second-stage ALPPS on day 8 following first-stage ALPPS (Fig. 5). There were no intraoperative complications and the blood loss was less than 50 ml. The postoperative histology revealed seven metastatic adenocarcinomas, with the largest one measuring 5.5 cm×3.3 cm (Fig. 6). The postoperative course was uneventful and the patient was discharged at 28 days after the first-stage ALPPS procedure.
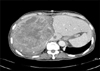
A 69-year-old male presented with epigastric discomfort and weight loss. He underwent radical subtotal gastrectomy because of stomach cancer, two years previously. The postoperative histology was advanced gastric carcinoma and histologic type was hepatoid adenocarcinoma. The cancer stage was T2N0M0, stage I. A contrast-enhanced CT revealed a large tumor, measuring 16 cm×15 cm in segments 5-8, middle hepatic vein invasion, and no signs of liver cirrhosis. Liver function evaluation revealed albumin at 3.6 g/dl, creatinine at 0.66 mg/dl, international normalized ratio (INR) of 1.18, and serum bilirubin at 1.08 mg/dl. The patient had no ascites, no encephalopathy, and a platelet count of 272×103/mm3. The alpha-fetoprotein (AFP) level was 10,264 ng/ml and the prothrombin induced by vitamin K absence-II (PIVKA-II) level was 2,869 mAU/ml. The total liver volume was 2,044 ml, and the FLR volume was 385 ml (19%) (Fig. 7). Based on these findings, the researchers decided to achieve sufficient hypertrophy through an ALPPS procedure.
After a preoperative evaluation, the patient underwent surgery. During the first-stage operation, the right portal vein was dissected and divided with a vascular stapler. Transection of the liver parenchyma was performed at 1 cm on the right side of the falciform ligament, using a Cavitron ultrasonic surgical aspirator. An intermittent Pringle maneuver was performed during the parenchyma transection. The middle hepatic vein was divided during the transection, preserving the right and left hepatic veins. Blood loss during the first-stage ALPPS procedure was 1,500 ml. After the first stage of the ALPPS procedure, acute renal failure and posthepatectomy liver failure occurred and continuous renal replacement therapy was necessary. The patient began to recover on the 5th postoperative day.
At nine days postoperatively, an abdominal CT showed significant hypertrophy of the left lateral section (Fig. 8). The second operation started with the same abdominal incision and warm saline irrigation. The plastic bag was removed from the right extended lobe of liver. The right hepatic artery was then ligated and divided. The right bile duct and right hepatic vein were divided using vascular staplers. Two silicone drains were placed and the abdomen was closed.
Histopathology confirmed a 17 cm×14 cm×11 cm-sized probably metastatic hepatoid adenocarcinoma, from the stomach and presence of vascular invasion (Fig. 9). After the second procedure, the patient developed moderate ascites, mild elevation of serum bilirubin (3.51 mg/dl), and mild prolongation of prothrombin time (21.1 sec). The remaining postoperative course was uneventful and the patient was discharged 23 days, after the first procedure.
ALPPS has recently been developed to induce rapid liver hypertrophy to reduce posthepatectomy liver failure. In 2012, Schnitzbauer et al.3 reported that the technique of “right portal vein ligation combined with in situ splitting, induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings”. Also in 2012, de Santibañes and Clavien proposed the acronym ALPPS, for this novel surgical technique of associating liver partition and portal vein ligation for staged hepatectomy.5 ALPPS is still considered to be in an early developmental phase and its surgical indications and techniques have not yet been standardized.
The study's second case showed posthepatectomy liver failure and acute renal failure, after the first stage of ALPPS. Although these recovered after postoperative day 5, they were considered complications of Clavien-Dindo grade III or more.6 Some clinicians oppose the ALPPS procedure, due to its high morbidity and mortality. The initial experience of ALPPS was impeded by a high incidence of postoperative complications such as bile leakage, infections, and high mortality.7 Although the short-term results of ALPPS are improving due to the development of improved surgical techniques and accumulated experience, morbidity rates after ALPPS are 15.3-100%. These rates are exhibited with ≥Clavien-Dindo grade III morbidity rates of 13.6-44%. Mortality rates are reported to be 0-29%.6
Since many studies are currently underway to identify the factors associated with the morbidity and mortality of the ALPPS procedure, it is necessary to follow-up with additional studies. The first report of the International ALPPS Registry presented a 90-day mortality of 9% and a severe complication rate (Clavien-Dindo grade IIIb) of 27% in 202 patients. However, postoperative outcomes were significantly better in patients younger than 60 years and in those with colorectal liver metastasis (CRLM).4
In the first case, the researchers successfully performed ALPPS and colorectal surgery concurrently in a patient over 60 years of age. However, Kerollos et al. reported a severe complication rate of 23%, and 90-day mortality of 15% in a study of both ALPPS and colorectal surgery.8 The use of ALPPS for CRLM is expected to increase. Since ALPPS surgery for CRLM is performed in patients with no steatosis and no cirrhotic liver, liver hypertrophy and functional recovery after liver resection should be superior to those exhibiting cirrhotic liver. Research to reach consensus on a standardized surgical technique is necessary to improve results, after simultaneous ALPPS and colorectal surgery. Evidence-based criteria are essential to realize the potential advantages of ALPPS without increased morbidity or mortality.
Figures and Tables
Fig. 1
Preoperative computed tomography shows the largest metastasis located at the segment 6, measuring 6.5 cm×5.5 cm×6 cm.
Fig. 2
Preoperative computed tomography after 4 months, shows that the sizes of the hepatic metastases decreased, with the largest one measuring 3.5 cm×3 cm.
Fig. 4
Intraoperative photograph shows that the right hepatic artery and right hepatic vein were marked with vessel loops.

Fig. 5
Computed tomography volumetry on day 7, after the first-stage operation revealed future liver remnant volume was 35% of the total liver volume.

Fig. 6
Gross photograph of the specimen revealed seven metastatic adenocarcinomas, with the largest one measuring 5.5 cm×3.3 cm.

References
1. Loss M, Jung EM, Scherer MN, Farkas SA, Schlitt HJ. Surgical treatment of liver metastases. Chirurg. 2010; 81:533–541.
2. Clavien PA, Petrowsky H, DeOliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med. 2007; 356:1545–1559.
3. Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012; 255:405–414.
4. Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, et al. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg. 2014; 260:829–836. discussion 836-838.
5. de Santibañes E, Alvarez FA, Ardiles V. How to avoid postoperative liver failure: a novel method. World J Surg. 2012; 36:125–128.
6. Lau WY, Lai EC, Lau SH. Associating liver partition and portal vein ligation for staged hepatectomy: the current role and development. Hepatobiliary Pancreat Dis Int. 2017; 16:17–26.
7. Schadde E, Ardiles V, Slankamenac K, Tschuor C, Sergeant G, Amacker N, et al. ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg. 2014; 38:1510–1519.
8. Wanis KN, Buac S, Linecker M, Ardiles V, Tun-Abraham ME, Robles-Campos R, et al. Patient survival after simultaneous ALPPS and colorectal resection. World J Surg. 2017; 41:1119–1125.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download