Abstract
Backgrounds/Aims
Pancreaticoduodenectomy (PD) is associated with various surgical complications including healing failure of the pancreaticojejunostomy (PJ). This study intended to ensure blood supply to the pancreatic stump through extended pancreatic transection (EPT).
Methods
This study assessed whether EPT reduces PJ-associated complications and whether EPT is harmful on the remnant pancreatic function. The EPT group included 19 patients undergoing PD, pylorus-preserving PD (PPPD) or hepatopancreaticoduodenectomy. The propensity score matched control group included 45 patients who had undergone PPPD. Pancreatic transection was performed at the level of the celiac axis in the EPT group, by which the pancreatic body was additionally removed by 3 cm in length comparing with the conventional pancreatic transection.
Results
A small invagination fissure suspected as the embryonic fusion site was identified at the ventro-caudal edge of the pancreatic body in all patients undergoing EPT. A sizable fissure permitting easy separation of the pancreatic parenchyma was identified in 15 of 19 patients (78.9%). The incidence of significant postoperative pancreatic fistula was significantly lower in the EPT group than in the control group (p=0.047). There was no significant increase in the postoperative de novo diabetes mellitus in EPT group (p=0.60).
Pancreaticoduodenectomy (PD) is an aggressive surgical procedure associated with high morbidity, even with advancements in surgical techniques and perioperative management that have decreased the incidence of surgical complications. The most serious major complication after PD is the failure of healing at the pancreatico-enteric anastomosis.1234 Uncontrolled pancreatic fistula (PF) can be led to major complications including pseudoaneurysm formation and resultant bleeding, abdominal abscess and disruption of other anastomoses. Since the safety of PD surgery depends mainly on prevention of PF, many surgical and medical methods have been used to reduce the occurrence of PF. These measures do not completely prevent the incidence of PF so far.
When performing re-operation for complicated major PF after PD, we observed partial or total disruption of pancreaticojejunostomy (PJ) with marginal necrosis of the pancreatic stump. Considering that major PF and PJ disruption usually happens 4-7 days after PD, we presumed that anastomotic failure of PJ is closely associated with ischemic necrosis of the pancreatic stump. Various risk factors for anastomotic failure of PJ have been reported.12345678910 However, we have occasionally experienced patients showing major PF and PJ disruption without any recognized risk factors.
As a conceptual shift, we searched for new risk factors that can affect the blood perfusion of the remnant pancreatic stump. Thus, we focused on the anatomical variation of the pancreatic parenchyma, which is associated with the fusion status of the dorsal and ventral pancreas during the embryonic development.1112 Based on our surgical experience, we identified a potential fusion fissure at the proximal portion of the pancreatic body in a considerable proportion of patients undergoing PD. We intentionally transected the pancreatic body distal to this fusion fissure to completely remove the ventral pancreas. This was done with the hypothesis that there is a potential blood flow disturbance crossing the fusion fissure, and that extended pancreatic transection (EPT) can prevent PJ-associated complications.
In this study, we assessed the clinical usability of EPT on patients undergoing PD through a case-controlled study. The primary end-point was whether EPT induces reduction of PJ-associated complication. The secondary end-point was whether EPT induces no harmful effect on the remnant pancreatic function.
Based on the prior personal experience of one author (SH) on >200 cases of PD, we learned that EPT at the level of the celiac axis seems to be beneficial to prevent the incidence of major PF after PD. Thus, the EPT technique has been selectively performed selectively for patients at high risk of PF, such as normally soft pancreatic parenchyma with a small main pancreatic duct. After the EPT technique was deemed worthy of clinical application, it was routinely adopted to the patients undergoing PD beginning in August 2014.
To evaluate the clinical usability of EPT, we designed a case-controlled study. For the study group, the study period was set as the 2-year period from August 2014 to July 2016. During that time, EPT was applied to 19 consecutive patients undergoing PD, pylorus-preserving PD (PPPD) or hepatopancreaticoduodenectomy (HPD) by a single surgeon (SH). These 19 patients were the study candidates and comprised the EPT group.
Considering the patient number of the study group, the patient number of the control group was estimated with a type-I error (α) of 0.10 and a type-II error (β) of 0.20 in addition to 20% difference in complication rates, by which the minimal patient number in the control group was 45. To objectively compare the incidence of PD-associated complications, we selected the control group patients through a propensity score matching method. Patient demographics, primary diseases, consistency of pancreatic parenchyma (soft nature only), diameter of the main pancreatic duct (≤3 mm) on imaging studies, types of pancreaticojejunal anastomosis (duct-to-mucosa reconstruction with internal drainage tube only), and no application of EPT were the criteria. Through a review of the medical records and follow-up imaging, we identified 45 patients during the period from January 2008 and July 2014. The medical records of these patients were retrospectively reviewed with special attention to perioperative complications after approval of the Institutional Review Board of our institution.
In the control group, the conventional level of pancreatic transection for PD was the medial border of the superior mesenteric vein (SMV). Thus, only the confluence portion of the SMV-splenic vein was exposed. We did not dissect the caudal border of the remnant pancreas under the belief that preservation of all peripancreatic connective tissues is beneficial to make PJ secure.
In contrast, in the EPT group the ventro-caudal edge of the pancreatic body was gently dissected to identify an oblique-lying fusion fissure. The length, depth and location of this fissure varied, but all were located between the levels of the SMV and the celiac axis. Thus, the pancreatic body was transected 1 cm distal to the fusion fissure, which was usually placed at the level of the celiac axis. EPT resulted in the additional removal of the pancreatic body by 3 cm in length comparing with the conventional pancreatic transection (Figs. 1 and 2).
The same surgical technique was used for PJ regardless of EPT application. The surgical technique for end-to-side duct-to-mucosa PJ was as follows. Running sutures were made at the dorsal edge of the pancreatic stump with 5-0 Prolene. Multiple interrupted sutures with 6-0 Prolene were done for duct-to-mucosa anastomosis. A size-matched silastic tube 10-15 cm in length was inserted into the remnant pancreatic duct and then transfixed with 4-0 chromic catgut or 6-0 absorbable monofilament. Finally, running sutures at the ventral edge of the pancreatic stump with 5-0 Prolene were made.
Fibrin glue sealant was applied over the PJ site. The omental graft patch was attached around the PJ site if possible. Three suction-type cigarette drains were also inserted around the PJ site. The procedures to make this drain were as follows. Multiple small side-holes were made at the 10 cm-length of each 25 cm-long and 10 mm-wide silastic Penrose drain and 50 cm-long and 4.8 mm-sized tube line of Jackson-Pratt drain tube. A Jackson-Pratt drain tube was inserted into the Penrose drain with overlapping of the side-hole portions, by which these two tubes were integrated as a conventional cigarette drain. A 4 mm-long skin incision was made and a set of Mosquito clamps was inserted to pull out the drain from the peritoneal side. The outside portion of this drain was tightly tied to prevent air leak at the skin level, while the inner drainage tube was connected to a Jackson-Pratt type suction bag.13
Multidetector dynamic abdominal computed tomography (CT) was performed at 5-7 days, 10-14 days and every week during admission. We set the hospitalization period to be 3 weeks after PD even in patients without any complication, thus all patients underwent CT scan at least three times after PD during admission. The status of PJ site was evaluated with comparison of the interval changes of CT findings, with special attention to the perfusion status of the pancreatic stump.
For the diagnosis of pancreatic leak, the concentrations of amylase and lipase in the drains were measured daily or every other day for more than 10 days until drain removal. For the diagnosis of PF, an amylase concentrations in the drain of more than three times of the serum value on day 3 or more after surgery was used to define patients with positive drain amylase. Postoperative pancreatic leakage was graded according to the classification of the International Study Group on Pancreatic Fistula (ISGPF).141516
For assessment of the endocrine function of the remnant pancreas, the 6-month incidence of de novo diabetes mellitus was assessed.
The pancreatic resection rate was assessed through perioperative measurement of the pancreas volume by using CT volumetry software (Petavision and Dr. Liver software). The reconstruction status of PJ was assessed with three-dimensional reconstruction software (Horos version 2.0; open-source free medical image viewer).
Numeric data are presented as the means with standard deviation or as medians with a range. Continuous variables were compared using Student's t-test. Variables reporting incidences were compared using the χ2 test or Fisher's exact test. A p-value <0.05 was considered to be statistically significant. The eligible number of patients in the control groups was calculated using MedCalc (version 15.11.4; MedCalc Software, Ostend, Belgium). Statistical analyses were performed using SPSS version 22 (SPSS Inc., Chicago, IL, USA).
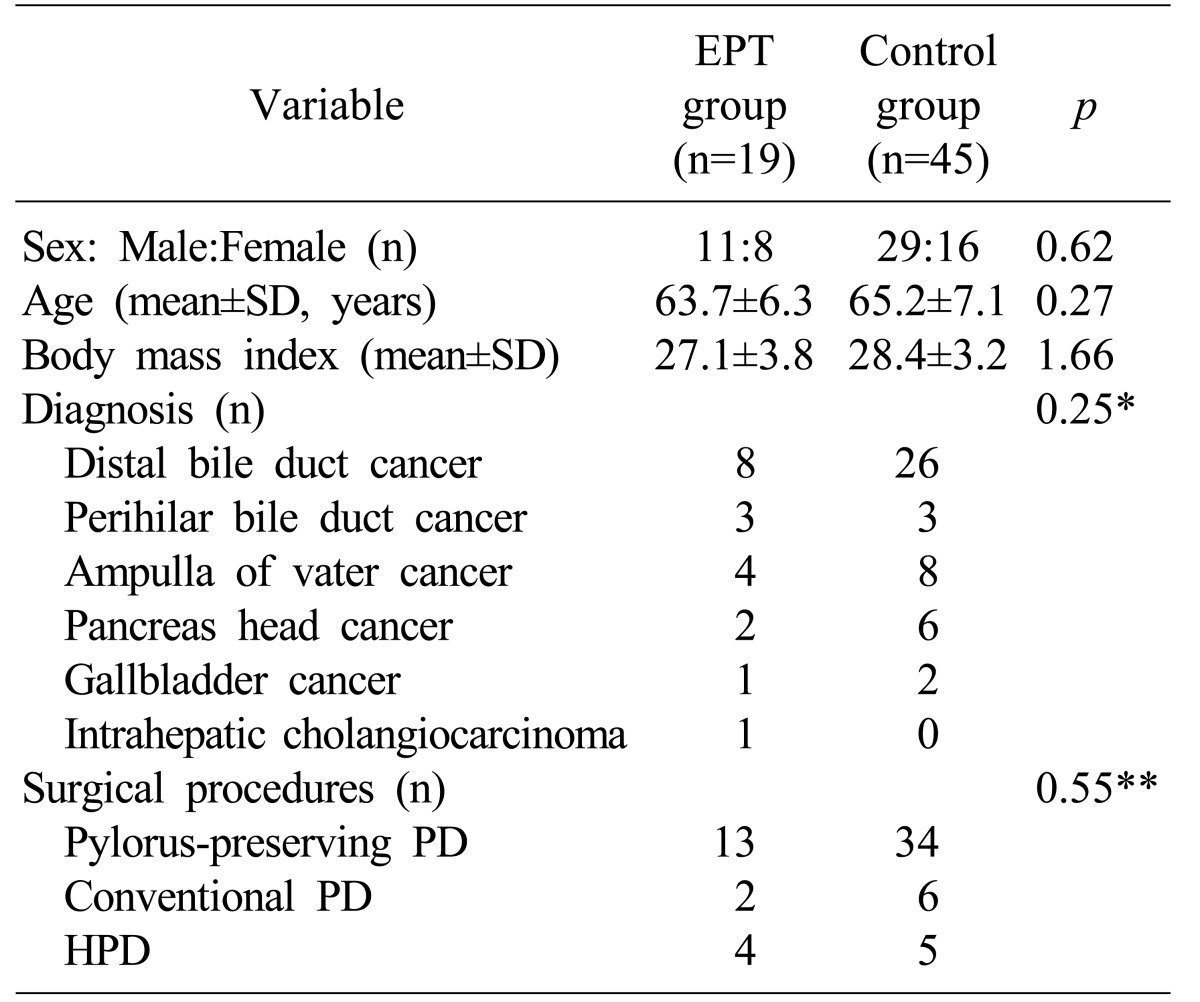
The demographic characteristics and surgical profiles of the EPT and control groups are summarized in Table 1. There were no significant differences in age, sex, body mass index, diagnosis and surgical procedures. In the EPT group, PPPD, conventional PD and HPD were done in 13, 2 and 4 patients, respectively.
A small fusion fissure was identified at the ventro-caudal edge of the pancreatic body in all 19 patients undergoing EPT (Figs. 1 and 2). A noticeable fissure permitting easy separation of the pancreatic parenchyma for 5 mm or more in length was identified in 15 of 19 patients (78.9%) in the study group.
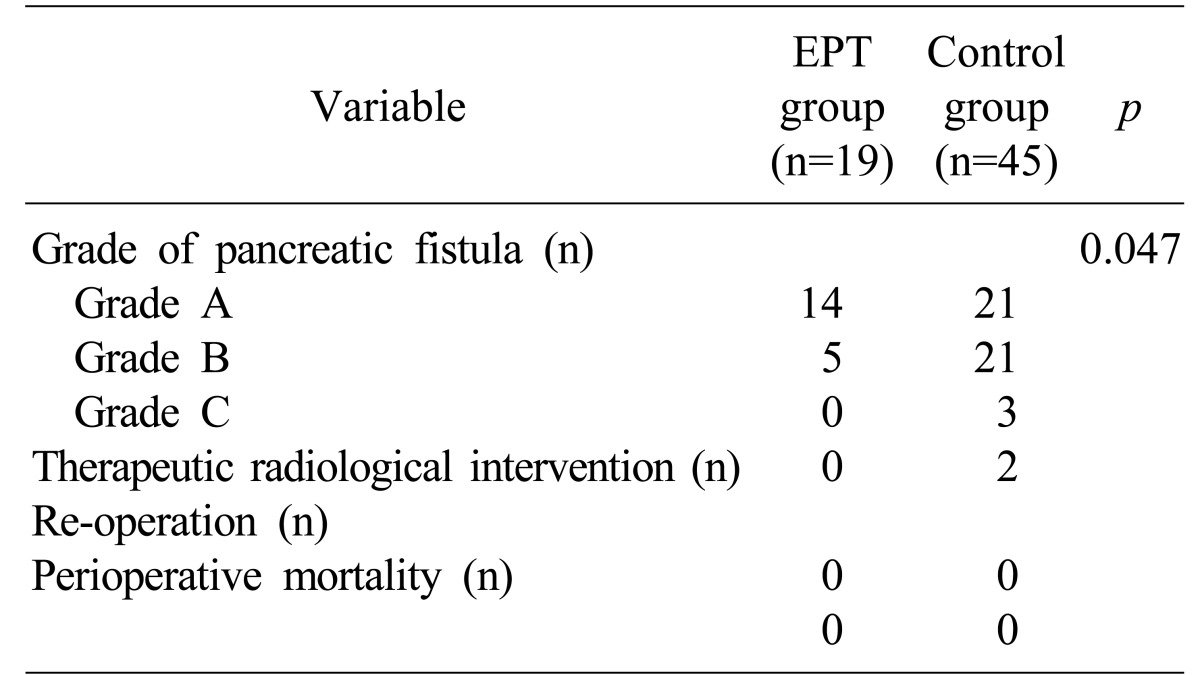
Incidences of postoperative complications focused on the incidence of PF in the study and control groups are summarized in Table 2. In the EPT group, postoperative PF was grade A, B and C in 14, 5 and zero patients, respectively. The incidences of PF grade B and C were significantly lower in the EPT group than in the control group (p=0.047). There was no case of reoperation and perioperative mortality within 3 months in the EPT and control groups.
We serially followed-up the status of the PJ site with dynamic CT scans to delineate the perfusion status of the pancreatic stump (Figs. 3 and 4). Pancreatic resection rates were compared between the study and control groups. Analysis of the 1-week CT scan images revealed secure approximation between the pancreatic stump and jejunal limb wall with unimpaired pancreatic perfusion in 17 of 19 patients (89.5%) in the EPT group and 33 of 45 patients (73.3%) in the control group.
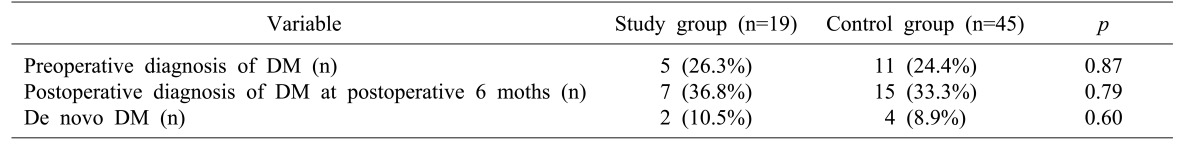
Perioperative diabetes mellitus data are summarized at Table 3. Postoperative de novo diabetes mellitus involved 2 patients (10.5%) in the EPT group and 4 patients (8.9%), with no difference (p=0.60).
PD has been regarded as the standard procedures for various malignant lesions in the periampullary region. Although the techniques of PD have improved considerably, a considerable proportion of patients still experience major surgical complications. PJ leakage is the main cause of morbidity and mortality after PD. Pancreatic leakage can result in various kinds of surgical complications, including pseudoaneurysm formation and anastomotic disruption.1416 It also leads to prolonged hospitalization, increased health care costs and even mortality.17 There are many factors in literature that can influence pancreatic leakage after PD include age, gender, preoperative jaundice, operative time, intraoperative blood loss, type of pancreatic reconstruction, anastomotic technique, consistency of the pancreatic stump, pancreatic duct diameter, use of somatostatin and surgeon's experience.141718
Surgical techniques for PD have evolved and matured over a long time. The majority of clinical studies regarding the surgical aspects of PD have primarily focused on the techniques of pancreatic reconstruction per se. Little attention has been paid to the site of pancreatic transaction, which is the site of pancreatic reconstruction. The arterial blood supply of the pancreatic neck and body from the dorsal pancreatic artery and transverse pancreatic arteries is well described in detail in anatomy textbooks. Yet, we have occasionally experienced scanty arterial bleeding at the pancreatic stump during transection, especially at the ventro-caudal cross-sectional area. The imaging analysis on the PJ site in the present study revealed that this area at the pancreatic stump appears to be vulnerable to ischemic change.
Many hepato-pancreato-biliary surgeons believe that the pancreas is one integrated organ with an abundant arterial blood supply, through which any resection of pancreas including segmental resection of the pancreatic body is feasible without risk of ischemia. In contrast, anatomical variations in the pancreatic anatomy, such as accessory pancreatic duct and annular pancreas, develop at the time of fusion of the dorsal and ventral pancreas during embryonic development. If the fusion process is not perfect, we presume that it can leave some rudimentary structures at the fusion site. We found a fissure with invagination of the pancreatic capsule at the pancreatic body. We presumed it to be rudimentary evidence of embryonic pancreatic fusion, and so arbitrarily named it fusion fissure. We hypothesized that arterial development beneath this fissure is less abundant than other pancreatic areas. This hypothesis led us to postulate that it may be beneficial to completely remove the pancreatic parenchyma associated with this fissure. Such pancreatic fusion-associated variation can be overcome by the use of EPT.
The location of the main pancreatic duct is not at the center all along the pancreatic body. Its location is eccentric at the neck portion and tends to be more concentric at the body portion. This anatomical feature indicates that more concentrically located pancreatic duct stump can be obtained through pancreatic transection at the level of celiac axis like EPT comparing with the conventional pancreatic transection. This concentric location must be beneficial to perform secure reconstruction of PJ. Thus, the theoretical advantages of EPT are the unimpeded pancreatic stump blood supply and the creation of a more concentric remnant pancreatic duct.
These theoretical advantages of EPT are validated in this study as being the primary end-point, which was whether EPT can effectively reduce the incidence of PJ-associated complication. The incidence of grade A PF was similar in the study and control groups, but the risk of grade B and C PF was significantly lower in the EPT group because grade A PF is often encountered during the early postoperative period but spontaneously resolved a few days later. Thus, we believe that EPT is beneficial to reduce PJ-associated complication effectively. At first, we had meticulously explored the presence of a fusion fissure and then determined the pancreatic transection line case by case. After performing EPT in first 10 cases, we recognized that the estimated pancreatic transection line was uniformly located at the celiac axis level. So we determined the pancreatic transection line in advance and then searched for the fusion fissure in a retrograde fashion.
Our imaging analysis regarding the blood supply at the pancreatic stump revealed nearly no ischemic portion after EPT, but a small area of marginal ischemia was detected in 25% of patients in the control group. This finding is strong evidence that EPT is beneficial to prevent impaired blood supply at the pancreatic stump.
EPT has a potential disadvantage from the additional removal of the pancreatic parenchyma because it is intended only to secure pancreatic reconstruction, but is not related to the oncological aspect. Thus, we assessed whether EPT is detrimental to the exocrine and endocrine function of the remnant pancreas as the secondary end-point of the study. EPT resulted in additional pancreatic resection of 10-15% compared with the control group. No patient suffered from intractable steatorrhea in both the study and control groups. Under normal conditions in adults, approximately 1,000 ml of pancreatic juice is excreted daily. We previously reported that the mean daily amount of excreted pancreatic juice after PPPD through an external pancreatic drainage tube is 229±99 ml.1920 Although the amount of pancreatic juice may be correlated with the volume and quality of the remnant pancreas, we believe that additional pancreatic resection of 10-15% does not result in a significant reduction of pancreatic secretion. Regarding the pancreatic endocrine function, 10.5% of patients developed de novo diabetes mellitus at postoperative 6 months. Considering that pancreatic islets are more abundant at the pancreatic tail, additional pancreatic resection of 10-15% may not deteriorate the pancreatic endocrine function significantly. The incidence of de novo diabetes mellitus was quite comparable between the EPT and control groups.
Effective management of major PF is a major concern. Firstly, effective drainage must be important, but postoperative insertion of percutaneous catheter seems to be often risky. We think that the conventional Jackson-Pratt type suction drain is not effective to drain thick or sticky materials that are a product of pancreatic leakage and subsequent necrosis. We devised a customized closed-suction drain with combination of Jackson-Pratt suction drain and cigarette drain tip. This drain works effectively for more than 2-3 weeks in the situation of major PF.
The present study has several limitations. First, this is a retrospective case-controlled study although EPT was performed as a part of prospective trial. Second, the case number of study group was not large enough to demonstrate the fusion fissure as a new landmark of the pancreatic anatomy. Further validation of our results regarding the benefit of EPT and anatomical significance of the fusion fissure is necessary through studies with large patient populations from multiple centers.
In conclusion, the results of our study demonstrate that EPT enables the complete removal of the ventral pancreas, which contributes to the reduction of major PF without impairment of the remnant pancreatic function. We believe that EPT is worthy of clinical application routinely, or at least in patients with a known risk of PJ leak.
References
1. Trede M, Schwall G. The complications of pancreatectomy. Ann Surg. 1988; 207:39–47. PMID: 3276272.

2. Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992; 127:945–949. PMID: 1353671.
3. Yeo CJ. Management of complications following pancreaticoduodenectomy. Surg Clin North Am. 1995; 75:913–924. PMID: 7660254.
4. Aranha GV, Aaron JM, Shoup M, Pickleman J. Current management of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2006; 140:561–568. PMID: 17011903.

5. Strobel O, Brangs S, Hinz U, Pausch T, Hüttner FJ, Diener MK, et al. Incidence, risk factors and clinical implications of chyle leak after pancreatic surgery. Br J Surg. 2017; 104:108–117. PMID: 27763684.

6. Fu SJ, Shen SL, Li SQ, Hu WJ, Hua YP, Kuang M, et al. Risk factors and outcomes of postoperative pancreatic fistula after pancreatico-duodenectomy: an audit of 532 consecutive cases. BMC Surg. 2015; 15:34. PMID: 25887526.

7. Relles DM, Burkhart RA, Pucci MJ, Sendecki J, Tholey R, Drueding R, et al. Does resident experience affect outcomes in complex abdominal surgery? Pancreaticoduodenectomy as an example. J Gastrointest Surg. 2014; 18:279–285. PMID: 24222321.

8. Burkhart RA, Relles D, Pineda DM, Gabale S, Sauter PK, Rosato EL, et al. Defining treatment and outcomes of hepaticojejunostomy failure following pancreaticoduodenectomy. J Gastrointest Surg. 2013; 17:451–460. PMID: 23292459.

9. Xiong JJ, Altaf K, Mukherjee R, Huang W, Hu WM, Li A, et al. Systematic review and meta-analysis of outcomes after intraoperative pancreatic duct stent placement during pancreaticoduodenectomy. Br J Surg. 2012; 99:1050–1061. PMID: 22622664.

10. Haga Y, Wada Y, Takeuchi H, Ikejiri K, Ikenaga M. Prediction of anastomotic leak and its prognosis in digestive surgery. World J Surg. 2011; 35:716–722. PMID: 21184072.

11. Guo P, Preuett B, Krishna P, Xiao X, Shiota C, Wiersch J, et al. Barrier function of the coelomic epithelium in the developing pancreas. Mech Dev. 2014; 134:67–79. PMID: 25266457.

12. Godlewski G, Gaubert J, Cristol-Gaubert R, Radi M, Baecker V, Travo P, et al. Moving and fusion of the pancreatic buds in the rat embryos during the embryonic period (carnegie stages 13-17) by a three-dimensional computer-assisted reconstruction. Surg Radiol Anat. 2011; 33:659–664. PMID: 21614602.

13. Hwang S, Ha TY, Kim JS, Cheong O, Kim KH, Lee SG. Clinical application of sution-type cigarette drain for hepatopancreatoabiliary surgery. J Korean Surg Soc. 2004; 67:428–431.
14. Bassi C, Falconi M, Molinari E, Mantovani W, Butturini G, Gumbs AA, et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery. 2003; 134:766–771. PMID: 14639354.

15. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID: 16003309.

16. Facy O, Chalumeau C, Poussier M, Binquet C, Rat P, Ortega-Deballon P. Diagnosis of postoperative pancreatic fistula. Br J Surg. 2012; 99:1072–1075. PMID: 22539219.

17. El Nakeeb A, Salah T, Sultan A, El Hemaly M, Askr W, Ezzat H, et al. Pancreatic anastomotic leakage after pancreaticoduodenectomy. Risk factors, clinical predictors, and management (single center experience). World J Surg. 2013; 37:1405–1418. PMID: 23494109.

18. Strasberg SM, Drebin JA, Soper NJ. Evolution and current status of the Whipple procedure: an update for gastroenterologists. Gastroenterology. 1997; 113:983–994. PMID: 9287993.

19. Jung DH, Hwang S, Lee SG. An analysis on the amount of excreted pancreatic juice after pancreatoduodenectomy. Korean J Gastroenterol. 2004; 43:309–315. PMID: 15156118.
20. Yoo D, Hwang S, Kim KH, Ahn CS, Moon DB, Ha TY, et al. Pancreatic atrophy relative to external versus internal drainage of the pancreatic duct after pylorus-preserving pancreaticoduodenectomy. J Gastrointest Surg. 2014; 18:1604–1609. PMID: 25002021.

Fig. 1
Case 1 details. A 57-year-old male patient undergoing pylorus-preserving pancreaticoduodenectomy with extended pancreatic transection technique for distal bile duct cancer. (A) An invagination fissure (arrow) is identified. (B) The pancreatic body was transected at the celiac axis level. (C) A small pancreatic duct located at the center of the pancreatic stump was identified. (D) Duct-to-mucosa pancreaticojejunostomy was performed.
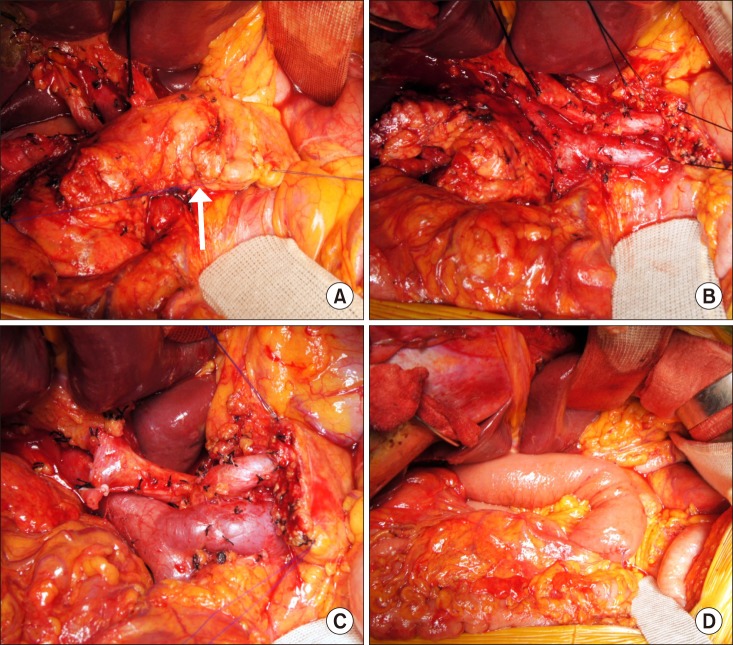
Fig. 2
Case 2 details. A 62-year-old male patient undergoing hepatopancreaticoduodenectomy including right hepatectomy, caudate lobectomy, pylorus-preserving pancreaticoduodenectomy with extended pancreatic transection technique, and portal vein resection and interposition graft for intrahepatic cholangiocarcinoma. (A) An invagination fissure (arrow) is identified. (B) The pancreatic body was transected at the celiac axis level.

Fig. 3
Computed tomography follow-up of case 1. (A) Preoperative image shows abundant pancreatic parenchyma with a small pancreatic duct. (B) Post-operation 1-week image shows secure attachment of the jejunal limb wall at the pancreatic stump.

Fig. 4
Computed tomography follow-up of case 2. (A) Preoperative image shows abundant pancreatic parenchyma with a small pancreatic duct. (B) Post-operation 1-week image shows secure attachment of the jejunal limb wall at the pancreatic stump. (C) Post-operation 1-year image shows intact perfusion status of the remnant pancreas with mild pancreatic parenchymal atrophy.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download