INTRODUCTION
Chronic pancreatitis is a progressive and permanent destruction of pancreas, resulting in disabling pain and irreversible loss of the endocrine/exocrine pancreatic function. The range of the incidence in Western countries is reported between 4.0-13.4 cases per 100,000 people, but the global incidence seems to be rising.1 Management consists of replacing the endocrine/exocrine deficiencies, use of analgesics (including opioids), and endoscopic and surgical interventions when necessary. Almost half the patients require surgery during the course of chronic pancreatitis, with indications of: (i) no relief of the intractable abdominal pain, (ii) existence of complications such as obstruction or bleeding, (iii) suspected malignancy, or (iv) combinations of the above. Here, we present a patient surgically treated for intractable pain of chronic pancreatitis, having complications of biliary obstruction and portal vein stenosis/thrombosis, resulting in cavernous transformation.
CASE
A 51 year-old male was diagnosed with chronic pancreatitis of seven months duration, having an obscure etiology. He was a non-drinker and a non-smoking. His chief symptom included several episodes daily of severe abdominal pain, and unable to stand without narcotic analgesics. The pain was mainly epigastric, but radiating to the rear. It was more severe after meals, and was relieved by leaning forward. Patient had lost weight (from 90 kg to 65 kg), and was diabetic.
The diagnosis of chronic pancreatitis was made based on the clinical presentation, radiological workups and percutaneous biopsy at another center. He had a metallic biliary stent for biliary stenosis. Endoscopic examinations revealed gastritis. A percutaneous celiac axis blockage was required for severe episodes of pain. Before referring to our center, patient had undergone laparotomy for pancreatic resection; however, because of the portal hypertension, the procedure had been capped off. The pancreatic tru-cut biopsy at this laparotomy confirmed the diagnosis of chronic pancreatitis without evidence of malignancy. He was then referred to us for surgery for pain relief.
At the time of admission, he was daily using narcotic analgesics, proton pump inhibitor, pancreas enzyme extracts and antidepressant drugs. He had mild anemia, slightly elevated liver function tests, and CA-19-9 was 202 U/ml. Computed tomography was compatible with chronic pancreatitis (heterogenous parenchyma, dilated pancreatic duct), and a 4 cm pseudocyst was seen at the tail of the pancreas (Figs. 1 and 2). Positron emission tomography revealed the pancreatic activity as 5.1 SUVmax.
We intended to make a pylorus-preserving pancreaticoduodenectomy with portal vein replacement. Before surgery, the patient and his relatives were informed of the possible surgical methods. A reverse “L” incision was used. Adhesions of the prior surgery and venous collaterals complicated the procedure. A cholecystectomy was performed, and the common bile duct was transected for bilio-enteric anastomosis to replace the biliary stent. The metallic stent in the distal bile duct was checked, but was found to be stuck and could not be removed. Subsequently, the common bile duct stump was closed. The dilated venous collaterals, particularly around the head of the pancreas, resulted in substantial blood loss during the dissection, and 3 red pack cells were transfused during the procedure (Fig. 3). It was then decided to pursue with the Frey procedure instead of pancreatic head resection. The inflamed pancreatic head was excavated, and the cavity at the pancreatic head was expanded to the distal pancreas (Figs. 4 and 5). The enlarged pancreatic duct became visible at the body and tail of the pancreas; however, the pancreatic duct at the head of the pancreas was not visible (Fig. 6). A Roux-en-Y pancreaticojejunostomy was created by 3-0 running polypropylene suture. Bilio-enteric anastomosis was done 10 cm distal of the pancreatic anastomosis with 4-0 polydiaxone interrupted sutures. Entero-enterostomy of the Roux limb was created in the usual way (Fig. 7). Totally, 40 ml absolute alcohol was injected around the celiac plexus for pain relief. Laparotomy was closed after insertion of two abdominal drains. The total operative duration was 490 minutes.
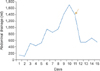
During the early postoperative period, patient was delirious in the intensive care unit, but the attacks were relieved after medications. Fortunately, the remaining postoperative course was uneventful, except for prolonged abdominal ascites drainage and intractable diarrhea that commenced on day 11, and was treated conservatively (Fig. 8). The drain amylase levels were continually in the normal ranges. Oral liquid and semisolid nourishments were started on days 5 and 7, respectively. Patient required only one dose of 60 mg meperidine in the postoperative period. He was discharged on day 28. Unexpectedly, pathological examination of the pancreatic specimen reported chronic pancreatitis accompanied with pancreatic cancer. He was then referred to the medical oncology department.
DISCUSSION
In the current case of chronic pancreatitis, since resection of the pancreatic head was not technically possible, excavation of the pancreas and draining the emergent cavity into the bowel (the Frey procedure) provided effective pain relief. Severe fibrosis, vascular invasions, venous collaterals and cavernous transformation around the pancreatic head prevent a safe pancreatic head resection. We therefore conclude that all these indications are good candidates for the Frey procedure.
There is no clarity in literature indicating the ideal surgical procedure for chronic pancreatitis. Although different guidelines suggest various features to select the ideal surgical procedure, these suggestion are broadly general.234 Distal pancreatectomy is indicated in patients where the disease is confined to the distal pancreas.234 Side-to-side pancreatico-jejunostomy cannot be applied when there is an inflammation at the pancreatic head or a narrow pancreatic duct.234 Total pancreatectomy is considered in rare cases having an associated problem of diabetes control.234 Surgery with the pancreatic head resection is the most widely performed method in patients with chronic pancreatitis, having two technical options: pancreaticoduodenectomy and duodenum preserving pancreatic head resection.234 Evidence based medicine reveals no difference in the mortality, adverse effects, or quality of life between both the methods.5 Recently, a comparative study on the preferred surgical method for chronic pancreatitis in Germany and United States, showed significant difference between the treatment protocols.6 The preferred surgical procedures were pancreaticoduodenectomy in the United States versus duodenum-preserving head resections in Germany. These differences seemed to be dependent upon unexplained disparities in the pathologic pancreatic anatomy between the two populations.6 Both surgical methods require the full-thickness resection of the pancreatic head; however, accomplishing the procedures in cases of venous collaterals, cavernous transformation, extensive fibrosis or porto-mesenteric stenosis or thrombosis, is not safe. In such cases, Frey procedure ensures both partial pancreatic head resection and the drainage of the pancreatic canal, and also provides sufficient pain palliation.
A recent meta-analysis showed a pooled prevalence of splanchnic vein thrombosis in 11.6% chronic pancreatitis patients. According to the location of splanchnic vein thrombosis, the pooled prevalence of portal vein, splenic vein, and mesenteric vein thrombosis was 6.2%, 11.2%, and 2.7% in pancreatitis, respectively.7 Surgical management of chronic pancreatitis in the presence of venous stenosis/thrombosis and in cavernous transformation is challenging. Although the presence of splanchnic vein stenosis/thrombosis as a complication of chronic pancreatitis per se and is not an indication for surgery, these patients sometimes require surgery for other complications of chronic pancreatitis. Adam et al.8 analyzed 16 such cases, and documented 69% intraoperative bleeding problems with a 10-fold increase in operative mortality, when compared to patients with normal splanchnic veins. They applied six pancreaticoduodenectomies, four Beger's procedures and only six Frey procedures. However, they reported that during five surgeries in which pancreaticoduodenectomy or Beger's procedure was initially planned, intraoperative bleeding led to a change to the Frey procedure.8 Despite these observations, they have not suggested that severe collaterals should be an indication for Frey procedure instead of the high risk pancreatic head resections.
The Frey procedure, first described in 1987, has pancreatico-jejunal anastomosis and entero-enterostomy for the Roux limb. The combination of biliary diversion with the Frey procedure is not a common approach. Recently, Merdrignac et al.9 demonstrated 19 Frey procedures with biliary-enteric anastomosis, and none of these cases had a splanchnic stenosis/thrombosis. They concluded that biliary diversion could be combined with Frey procedure when common bile duct stricture was present, without increasing the morbidity or affecting pain control.9 As per our knowledge, to date, there are no reported cases of Frey procedure combined with biliary diversion in a patient with portal vein stenosis and mesenteric venous collaterals.
We conclude that Frey procedure can be the favored surgical method in chronic pancreatitis patients with portal hypertension, portal venous thrombosis/stenosis or cavernous transformation. The procedure can be combined with bilio-enteric anastomosis in case of accompanying common bile duct obstruction.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download