This article has been corrected. See "Erratum: Correction of Abstract. Development and Effects of Simulation Practice Program about Family centered Delivery Care" in Volume 25 on page 234.
Abstract
Purpose
This study was conducted to investigate the relationship of knowledge, attitudes and needs of sex education in high school students.
Methods
There were 258 participants who were high school students in S high school in G city. Data were collected from October 1 to October 31, 2011, and analyzed using SPSS/WIN 19.0.
Figures and Tables
Table 1
Homogeneity Test for General Characteristics between Experimental and Control Group (N=53)
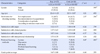
Table 2
Homogeneity Test of Knowledge of Delivery Care and Problem Solving Ability between Experimental and Control Group (N=53)
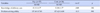
| Variables | Exp. (n=27) | Cont. (n=26) | t or Z | p |
|---|---|---|---|---|
| M±SD | M±SD | |||
| Knowledge of delivery care | 15.15±1.77 | 15.58±1.77 | −0.88 | .382 |
| Problem solving ability | 157.48±17.00 | 157.42±16.80 | 0.13 | .990 |
Table 3
Comparison of Dependent Variables between Experimental and Control Group (N=53)

Summary Statement
▪ What is already known about this topic?
Simulation-based practice is an effective learning method in maternity nursing and considered a complementary training method to compensate for circumstances that limit real-world clinical practicum.
▪ What this paper adds?
The simulation practice program about family centered delivery care provided a chance to learn by more practical experience with increased knowledge of delivery care and clinical performance ability of family centered delivery of nursing students.
▪ Implications for practice, education and/or policy
The simulation practice program about family centered delivery care is regarded as a method that can overcome limitations in clinical practice. It could be helpful in improving confidence on nursing performance in delivery room with patients and family.
References
1. Lee KH. Change of the childbearing culture: Family centered delivery. Nurs Sci. 2000; 12(2):11–16.
2. Lee MK, Hur MH. Effects of the spouse's aromatherapy massage on labor pain, anxiety and childbirth satisfaction for laboring women. Korean J Women Health Nurs. 2011; 17(3):195–204.

3. Choi MS, Kim GJ. Effects of paters` duola touch during labor on the paternal attachment and role confidence to neonate and couple attachment. Korean J Women Health Nurs. 2011; 17(4):426–437.

4. Oh JH, Lee HJ, Kim YK, Min J, Park KO. The effect of childbirth education and family participated delivery in a labor-delivery-recovery room on primiparas' anxiety, labor pain and perception of childbirth experience. Clin Nurs Res. 2006; 12(2):145–156.
5. Shim CS, Park MK, Kim JH. Effects of simulation-based delivery education regarding to obstetric clinical practice before and after of nursing students. J Korean Soc Matern Child Health. 2014; 18(1):125–133.
6. Lim KC. Directions of simulation-based learning in nursing practice education: A systematic review. J Korean Acad Soc Nurs Educ. 2011; 17(2):246–256.

7. Lee SO, Eom MR, Lee JH. Use of simulation in nursing education. J Korean Acad Soc Nurs Educ. 2007; 13(1):90–94.
8. Chung CW, Kim HS, Park YS. Effects of high-fidelity simulation-based education on maternity nursing. Perspect Nurs Sci. 2011; 8(2):86–96.
9. Lee SJ, Roh YS, Kim JO, Jang KI, Ryoo EN, Park YM. Comparison of multi-mode simulation and SimMan® simulation on evaluation of nursing care for patients with dyspnea. J Korean Acad Soc Nurs Educ. 2010; 16(1):51–60.
10. Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 2005; 27(1):10–28.
11. Lee WS, Kim M. Effects and adequacy of high-fidelity simulation-based training for obstetrical nursing. J Korean Acad Nurs. 2011; 41(4):433–443.

12. Kim KA. The Effect on education programwith hybrid simulation for delivery nursing care [Dissertation]. Seoul: The Catholic University of Korea;2014. p. 55.
13. Hong SY. The Effect on education programwith hybrid simulation for delivery nursing care [Dissertation]. Daegu: Kyungpook National University;2015. 68.
14. Kim SH. Effects of simulation-based practice using standardized patients for the care of women with postpartum hemorrhage on nursing student's clinical performance competence and critical thinking deposition. Korean Parent-Child Health J. 2012; 15(2):71–79.
15. Kim SA, Lee SK, Chae HJ. Effects of clinical practice and simulation-based practice for obstetrical nursing. Korean J Women Health Nurs. 2012; 18(3):180–189.

16. Song YA. Effect of Simulation-based practice by applying problem based learning on problem solving process, self-confidence in clinical performance and nursing competence. Korean J Women Health Nurs. 2014; 20(4):246–254.

17. Lee SJ, Jang YK, Lee HN, Park GY. Study on the development of life-skills: Communication, problemsolving, and self-directed learning. Research Report. Seoul: Korean Educational Development Institute;2003. RR2003-15-03.
18. Jeffries PR. A framework for designing, implementing, and evaluating simulation used as teaching strategies in nursing. Nurs Educ Perspect. 2005; 26(2):96–103.
19. Lewis DY, Ciak AD. The impact of a simulation lab experience for nursing students. Nurs Educ Perspect. 2011; 32(4):256–258.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download