Abstract
Purpose
This study examined degrees of irrational parenthood cognition, post traumatic stress disorder (PTSD), spousal support, and quality of life and investigated factors that influence the quality of life of infertile women.
Methods
Research design was a cross sectional correlational survey with a total of 113 female patients receiving treatment for infertility. Data were collected from August 1 to November 30, 2015. The collected data were analyzed using t-test, ANOVA, Pearson's correlation, and multiple regression analysis.
Results
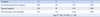
The mean score of the quality of life was 59.0±14.8. The quality of life was significantly associated with irrational parenthood cognition (r=-.70), post traumatic stress disorder (r=-.65), and spousal support (r=.56). The factors significantly affecting the quality of life in infertile women were irrational parenthood cognition (β=-.45), post traumatic stress disorder (β=-.34), and spousal support (β=.32). The explained variance by these factors was 70.4%, and the regression model was valid (F=89.81, p<.001).
Figures and Tables
Table 1
Differences in Quality of Life by General Characteristics of Subjects (N=113)
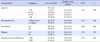
Table 2
Differences in Quality of Life by Infertility related Characteristics (N=113)

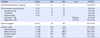
Table 3
Levels of Study Variables (N=113)
Summary Statement
▪ What is already known about this topic?
The quality of life in infertile women has been identified to have an association with depression, infertility related stress, marital adjustment, and family support.
▪ What this paper adds?
Influencing factors on the quality of life of infertile women were irrational parenthood cognition, post traumatic stress disorder, and spousal support.
▪ Implications for practice, education and/or policy
Nurses should take into consideration about irrational parenthood cognition, post traumatic stress disorder, and spousal support when taking care of the infertile couple in order to develop an intervention to improve the quality of life of infertile women.
References
1. Statistics Korea. Classified disease compensation and health care costs: 2004-2014 [Internet]. Daejeon: Author;2015. cited 2016 March 1. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=DT_35001_A071311&conn_path=I2.
2. Jeong KI. A study on hermeneutic grounded theory of women who experience infertility suffering and relief from pain. Korean J Soc Welf Stud. 2014; 45(4):5–35.
3. Boivin J, Takefman J, Braverman A. The fertility quality of life (FertiQoL) tool: Development and general psychometric properties. Fertil Steril. 2011; 96(2):409–415.

4. Valsangkar S, Bodhare T, Bele S, Sai S. An evaluation of the effect of infertility on marital, sexual satisfaction indices and health-related quality of life in women. J Hum Reprod Sci. 2011; 4(2):80–85.

5. Chachamovich JR, Chachamovich E, Ezer H, Fleck MP, Knauth DR, Passos EP. Agreement on perceptions of quality of life in couples dealing with infertility. J Obstet Gynecol Neonatal Nurs. 2010; 39(5):557–565.

6. Kim JH, Shin HS. A structural model for quality of life of infertile women. J Korean Acad Nurs. 2013; 43(3):312–320.

7. McQuillan J, Torres Stone RA, Greil AL. Infertility and life satisfaction among women. J Fam Issues. 2007; 28(7):955–981.

8. Burton RPD. Global integrative meaning as a mediating factor in the relationship between social roles and psychological distress. J Health Soc Behav. 1998; 39:201–215.

9. Matthews R, Matthews AM. Infertility and involuntary childlessness: The transition to nonparenthood. J Marriage Fam. 1986; 48(3):641–649.

10. Fekkes M, Buitendijk SE, Verrips GH, Braat DD, Brewaeys AM, Dolfing JG, et al. Health-related quality of life in relation to gender and age in couples planning IVF treatment. Hum Reprod. 2003; 18(7):1536–1543.

11. Lee HY, Si MH. Relationships between irrational beliefs and parenting stress of mothers with early children. J Fish Mar Sci Educ. 2011; 23(3):400–409.
12. White L, McQuillan J, Greil AL, Johnson DR. Infertility: Testing a help seeking model. Soc Sci Med. 2006; 62(4):1031–1041.
13. Engelhard IM, van den Hout MA, Arntz A. Posttraumatic stress disorder after pregnancy loss. Gen Hosp Psychiatry. 2001; 23(2):62–66.

15. Schwerdtfeger KL, Shreffler KM. Trauma of pregnancy loss and infertility for mothers and involuntarily childless women in the contemporary United States. J Loss Trauma. 2009; 14(3):211–227.
17. McQuillan J, Greil AL, White L, Jacob MC. Frustrated fertility: Infertility and psychological distress among women. J Marriage Fam. 2003; 65(4):1007–1018.

18. Lee JH. An analytical study on psychosocial predictors of depression and effective psychosocial intervention program for reducing depression of infertile women being in infertility treatment [dissertation]. Seoul: Korea University;2013. 124.
19. Foa EB, Cashman L, Jaycox L, Perry K. The validation of a selfreport measure of posttraumatic stress disorder: The posttraumatic diagnostic scale. Psychol Assess. 1997; 9(4):445–451.

20. Nam BR, Kwon HI, Kwon JH. Psychometric qualities of the Korean version of the posttraumatic diagnosis scale (PDS-K). Korean J Clin Psychol. 2010; 29(1):147–167.
21. Choi ES. The effects of pre and post operative education with both wives and husbands on the women's adaptation undergoing a hysterectomy [dissertation]. Seoul: Ewha Womans University;1992. 86.
22. Kim SN. A structural model for quality of life in women having hysterectomies. J Korean Acad Nurs. 1999; 29(1):161–173.

23. Aarts JWH, van Empel IWH, Boivin J, Nelen WL, Kremer JAM, Verhaak CM. Relationship between quality of life and distress in infertility: A validation study of the Dutch FertiQoL. Hum Reprod. 2011; 26(5):1112–1118.

24. Fardiazar Z, Amanati L, Azami S. Irrational parenthood cognitions and health-related quality of life among infertile women. Int J Gen Med. 2012; 5:591–596.
25. Kim JM. A study on the double faces of sexual lives in Islam. J Inst Middle East Stud. 2004; 23(2):217–244.
26. Engelhard IM, van den Hout MA, Vlaeyen JW. The sense of coherence in early pregnancy and crisis support and posttraumatic stress after pregnancy loss: A prospective study. Behav Med. 2003; 29(2):80–84.

27. Yu Y, Peng L, Chen L, Long L, He W, Li M, et al. Resilience and social support promote posttraumatic growth of women with infertility: The mediating role of positive coping. Psychiatry Res. 2014; 215(2):401–405.

28. Ha BY, Jung EJ, Choi SY. Effects of resilience, post-traumatic stress disorder on the quality of life in patients with breast cancer. Korean J Women Health Nurs. 2014; 20(1):83–91.

29. Kang EY. A review on psychosocial characteristics of infertile women. Stud Child Fam Ther. 2014; 12:1–16.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download